* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download (BCHCFT) Formulary - Birmingham Community Healthcare
Focal infection theory wikipedia , lookup
Remineralisation of teeth wikipedia , lookup
Harm reduction wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Special needs dentistry wikipedia , lookup
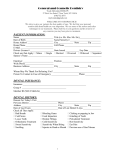
Drug Application Process & BCHCFT Formulary Version 1.0 If this is a paper copy of the document, please ensure that it is the most recent version. The most recent version is available on the Intranet/internet Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 1 of 21 Commencement of Consultation Date: November 2015 Consultation History: The following Committees, groups or individuals have been consulted in the development of this version of this Formulary: Name: David Harris (Chief Pharmacist) Johanne Deeks (Learning Disabilities Pharmacist) Melanie Dowden (Lead Pharmacist Community Health) Sudha Balakrishnan (Rehabilitation Consultant) Karen Mitchell-Meades (Head Pharmacist Moseley Hall Hospital) Carol Eadie (Head Pharmacist West Heath Hospital) Neal McCathie (Consultant Community Paediatrician) Dr Falope (Rehabilitation Consultant) Dr Chit Ko Ko (Consultant Physician in Rehabilitation Medicine) Rebecca Martin (Service Lead Tissue Viability) Andrea Richards (Consultant Oral Physician) Harriet Anstey (Consultant Oral Surgeon) Olayinka.M.Fadahunsi-Oluwole (Speciality Doctor Community Paediatrics) Medicines Management Committee Date: November 2015 December 2015 January 2016 January 2016 January 2016 January 2016 February/May 2016 February 2016 February 2016 March 2016 April 2016 April 2016 April 2016 March, April, May, June, July 2016 Previous Version History Version No. NA Lead Date Change Implemented Reason for Change New for BCHCFT This replaces consolidated Formulary (2014) and Community Hospitals Formulary (2012) Consultation Process Lead Clinicians are an integral part of the formulary development process and will provide expert clinical advice and support when a new drug formulary application is made. This information will be submitted to the Medicines Management Committee (MMC) in the first instance for first approval. Relevant Divisional Committees Proposed drugs to be considered for addition to BCHCFT formulary may be consulted at divisional committees before bringing to MMC for consideration. Area Prescribing Committee (APC) For medicines that BCHCFT services prescribe on FP10 or would like GPs to prescribe require final consultation and approval at the APC. Medicines must be approved by Medicines Management Committee prior to taking to the APC for consideration. Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 2 of 21 Section Page 1. Purpose 4 2. Scope 4 3. Responsibilities of Clinicians 4 4. Drug Application Process & BCHCFT Formulary 4.1 Formulary Revision Process 4.2 New Drug Application Process 4.3 BCHCFT Formulary 4 4 5 References/Evidence/Glossary/Definitions 12 5. Appendices 1. Example of an APC Drug Application Form 13 Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 3 of 21 1. Purpose The aim of the formulary is to encourage safe, rational and cost-effective prescribing, and to have a unified choice of treatment for patients. It will ensure seamless transition of care for patients between Birmingham Community Healthcare Foundation Trust (BCHCFT) and General Practice. It is a locally maintained document and it also sets out the process to be followed when requests are made for a medicine to be added to the formulary. 2. Scope This formulary will apply across the whole of BCHCFT within all divisions. 3. Responsibilities of Prescribers All prescribers are expected to take into account whether the medicine they intend to prescribe is on the formulary. BCHCFT prescribers should consult the Area Prescribing Committee Formulary and BCHCFT Formulary. 4. Drug Application Process & BCHCFT Formulary 4.1 Formulary Revision Process Drugs on the current BCHCFT formulary do not need to go through the drug application process. If there is any change to the way a drug is prescribed this would then need to go through the application process outlined below (4.2). The BCHCFT Formulary and the Drugs List (page7) should be reviewed at least every two years. A representative from each division should be present at Medicines Management Committee to review the drugs for their specialist area. If there are any significant changes, the appropriate information and evidence to support this will be required and bought to committee using the documentation in Appendix 1. 4.2 New Drug Application Process The following algorithm sets out how new drugs will be considered for addition to the formulary for use within BCHCFT and for prescribing in primary care by GPs. Applications for the inclusion of a medication to the BCHCFT Formulary must be initiated by a consultant or other appropriate senior healthcare professional. Requests for products to be added to the formulary require approval from the Medicines Management Committee (MMC) followed by the APC approval process. If relevant a new drug application can be discussed at a divisional committee (e.g. Dental Drugs and Therapeutics Committee) prior to consultation at MMC. Medicines Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 4 of 21 for use within BCHCFT services only are not required to go through the APC application process. Flow chart showing BCHCFT & APC Drug Application Process Complete Formulary Application (See APC*) Medicines Management Committee Not Approved Approved for BCHCFT use Is APC approval required? (i.e. Do GPs want to prescribe this drug or is it for BCHC prescribing only?) * Application form to be obtained from [email protected] See Appendix 1 as an example No ** Complete ESCA or RICAD if necessary. APC can provide more information - see APC website Add to BCHCFT approved list of medicines APC: Area Prescribing Committee RICAD: Rationales for Initiation, Continuation and Discontinuation ESCA: Effective Shared Care Agreement 4.3 Yes APC** Not Approved Approve d BCHCFT Formulary Birmingham Community Healthcare Foundation Trust is a community trust providing treatment to patients in community settings, hospitals and specialist care. In the majority of cases, drug treatments will have already been initiated by the patient’s GP or by another trust and if appropriate BCHCFT will continue. The BCHCFT Formulary comprises of two elements: (i) the Birmingham, Sandwell, Solihull and environs Joint Formulary otherwise referred to as the Area Prescribing Committee (APC) Formulary (ii) specified drugs in List A and B (page 7 to 12). The APC Formulary represents the drugs that Trusts and Clinical Commissioning Groups across the region have jointly agreed to prescribe in preference to other treatment options. It is expected the majority of prescribing will follow the APC formulary but this does not restrict a trust to prescribe or administer other such drugs where this is clinically indicated. The APC Formulary can be accessed here: http://www.birminghamandsurroundsformulary.nhs.uk/default.asp Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 5 of 21 Any prescriber who wishes to use a product outside of formulary should either make a formal application for it to be considered at APC or request an individual funding request (IFR) to the commissioner. Prescribers should note that if a non-formulary medicine is commenced without the necessary approval, the Trust could be charged the ongoing costs. All drugs included in the APC Formulary are allocated a traffic light status. The red amber green ratings offer guidance on where clinical and prescribing responsibilities lie in regard to the initiation and maintenance of prescribing. Key to APC Formulary Recommendations Initiation and maintenance of prescribing by Specialists, GPs and other qualified clinicians Initiation and maintenance of prescribing by Specialists and transfer to Primary Care prescribing when appropriate, or initiation and maintenance of prescribing in Primary Care following recommendation from a Specialist. Some amber medicines require agreement with the local (internal) medicines committee prior to initiation; others may require a framework to support safe transfer and maintenance of care such as a RICaD or ESCA. The Formulary will be annotated to reflect these requirements. Initiation and maintenance of prescribing by BCHCFT Specialists only. Positive NICE TA; awaiting local clarification on place in therapy. Non Formulary; may be prescribed following approval by individual hospital Medicines Management Committees for specific patients. (The term 'Specialist' refers to Consultants, Non-Medical Prescribers and General Practitioners with a Specialist Interest) Medicines listed in the tables below are for use within this Trust only so that prescribing or administration remains with BCHCFT clinicians. There are two lists of medicines: List A: Medicines not on the APC formulary but approved for prescribing or administration within BCHCFT e.g. anaesthetics, unlicensed medicines. These medicines cannot be prescribed by GPs unless approved by the APC. List B: Medicines currently part of the APC formulary but used within BCHCFT for an unlicensed indication or off-label e.g. beclometasone inhaler for oral ulcerative conditions; erythromycin as a prokinetic agent. Some unusual forms of administration may require an APC application if Specialists would like GPs to prescribe. Prescribing may be declined by a GP on the grounds they are not sufficiently familiar with the drug treatment to accept clinical responsibility for agents that are used off label or are unlicensed. Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 6 of 21 Note: These drug lists are correct at the time of writing. Please cross reference with the APC formulary for the most up to date information. List A: Medicines not in the APC Formulary approved for use in BCHCFT Name of drug approved in BCHCFT formulary Service Area Indication/Notes Adrenaline injection Articaine Atracurium injection Atropine injection Adults, Dental Dental Dental Adults, Dental AS Saliva Orthana Dental Benzocaine 20% gel (Ultracare Oral Bubble Gum ) Baclofen liquid (some strengths) BioXtra Gel and Mouthrinse Dental Acute anaphylaxis Anaesthetic Neuromuscular blockade Premedication; Intra-operative bradycardia; Control of muscarinic side-effects of neostigmine in reversing neuromuscular blockade Xerostomia, Sicca Syndrome/ Sjogren’s Syndrome, following Radiotherapy Topical anaesthesia Botulinum toxin B Budesonide nasal spray Bupivacaine 0.5% Calcium chloride injection Adults, Rehab Dental Adults, Rehab, Dental Dental Adults, Rehab, Dental Adults Carnoy’s solution (ethanol, chloroform, glacial acetic acid) Chloracetic acid crystals in solution Dental Chlorhexidine gluconate 2.5 mg (Periochip) Chlorhexidine gluconate surgical scrub (Hydrex) Chlorhexidine sachets (Unisept) Chlorhexidine 2% in Isopropyl Alcohol 70% (ChloraPrep) Co-codamol 8/500 Dental Dantrolene injection Dehydated alcohol Adults Skeletal muscle relaxant Xerostomia, Sicca Syndrome/ Sjogren’s Syndrome, following Radiotherapy Spasmodic torticollis; masseteric hypertrophy Oral ulcerative conditions Anaesthetic Hyperkalaemia, hypocalcaemia Odontogenic keratocyst Dental Treatment of hard corns and verrucae Antimicrobial treatment for chronic periodontal disease Surgical scrub Dental Dental Skin disinfection Skin disinfection Adults, Rehab, Dental Dental Dental Analgesic Malignant hyperthermia Trigeminal neuralgia Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 7 of 21 Diphtheria tetanus pertussis (acellular) and hib vaccine Dopamine Dobutamine solution for infusion Dosulepin Adults Dental Dental LD, Dental Ephedrine injection Esomeprazole injection Ethyl chloride spray Dental Adults Dental Ferric subsulphate 70% solution (Monsel’s solution) Flumazenil Gaviscon Advance Gelofusine infusion Glandosane spray Dental Dental, Rehab Adults Dental Dental Glucose infusion Glycopyrrolate Guanfacine hydrochloride (Intuniv) Hepatitis B vaccine Dental Rehab Children Adults Human Papillomavirus vaccine Children Hydrocortisone /Chlorhexidine /nystatin (Nystaform HC) Influenza vaccine (inactivated and live intranasal) Intralipid Isoflurane Ketorolac injection Levobupivacaine Lidocaine injection Lidocaine 2% in ethyl chloride Lidocaine 5% ointment Lidocaine + chlorhexidine (Instillagel) Lidocaine +/- adrenaline Lidocaine+prilocaine (Oraqix, Emla) Magnesium sulphate paste Medical gases (e.g. oxygen, nitrous oxide) Measles Mumps Rubella vaccine Dental Adults/Children Dental Dental Dental Rehab Rehab Adults Dental Adults Dental, Rehab Dental Rehab Adults, Dental Children Immunisation Inotropic agent Inotropic agent For Dental - facial pain: Antidepressant Sympathomimetic Gastroesophageal disease Topical anaesthetic; vitality testing Topical haemostatic agent Conscious sedation Gastrointestinal symptoms Plasma substitute Xerostomia, Sicca Syndrome/ Sjogren’s Syndrome, following Radiotherapy Hypoglycaemia Hypersalivation ADHD in children Immunisation against hepatitis B Prevention of cervical cancer and premalignant cervical lesions Oral ulcerative conditions Prevention of seasonal flu Reversal of local anaesthetic overdose Anaesthesia Post operative pain Anaesthesia Anaesthesia Anaesthesia Anaesthesia Catheterisation Anaesthesia Local anaesthetic Superficial skin infections Treatment of hypoxaemia; anaesthesia Prevention against measles, mumps, rubella Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 8 of 21 Mepivacaine 3% Meningococcal ACWY (MenACWY) Adults, Dental Adults Midazolam1mg/1ml injection, intranasal (+ lidocaine) Midazolam 10mg/ml buccal Minocycline 2% periodontal gel (Dentomycin) Neostigmine injection Dental, Rehab LD, Dental Dental Phenol Aqueous 6%injection Phenol in Glycerol 5% injection Phenol liquid PEP (Kaletra, Truvada, raltegravir) Rehab Rehab Adults Dental Pneumococcal polysaccharide vaccine Adults Povidone Iodine 7.5% surgical scrub/ Prilocaine Prilocaine Hydrochloride with Felypressin (Citanest) Propofol Pyrogallol 40% in WSP Dental Reversal of neuromuscular blockade Reversal of neuromuscular blockade Anaesthesia; sedation Acute hypotension Neuropathic pain Diagnostic agent Recurrent Aphthous Stomatitis; Osteoradionecrosis Nerve ablation Intrathecal for spasticity Ablation of the nail bed Prevention of HIV needle stick injury Immunisation against disease caused by Streptococcus pneumoniae Skin disinfection Dental Dental Anaesthesia Anaesthesia Dental Adults Rocuronium injection Salicylic acid 60% in WSP Dental Adults Saliva Stimulating Tablets (SST) Dental Sativex spray Rehab Sevoflurane Shingles vaccine (Zostavax) Sodium bicarbonate injection Sodium chloride mouthwash Dental Adults Adults Dental Anaesthesia; sedation Treatment of neurovascular corns Neuromuscular blockade Treatment of hard corns and verrucae Xerostomia, Sicca Syndrome/ Sjogren’s Syndrome, following Radiotherapy Refractory spasticity in patients with MS Anaesthesia Immunisation against shingles Metabolic acidosis Mucosal ulceration & inflammation Neostigmine/glycopyrronium Nitrous oxide Noradrenaline injection Nortriptyline Omnipaque (Iohexol) Pentoxifylline Dental Anaesthesia Vaccination against meningococcal disease Premedication/ conscious sedation Seizures Chronic adult periodontitis Dental Dental Dental Dental, Rehab Dental Dental Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 9 of 21 Sodium chloride infusion/injection Sodium lactate infusion (Hartmanns) Sodium fluoride varnish/ tablet Sugammadex (Bridion) Dental Dental Fluid replacement/Flush Hyperchloraemic acidosis Dental Dental Suxamethonium injection Sterile glycerin Tetracaine gel (Ametop) Tetrafluoroethane spray Dental Adults Dental Dental Thiopental Tiagabine Tranexamic acid injection/oral solution Xerotin spray Dental LD Dental Prevention of dental caries Reversal of neuromuscular blockade Neuromuscular blockade Neutralisation of phenol Local anaesthesia Production of topical cryoanaesthesia in the oral cavity Anaesthesia Seizures Fibrinolysis during dental procedures; mouthwash Xerostomia, Sicca Syndrome/ Sjogren’s Syndrome, following Radiotherapy Psychoses Zuclopenthixol acetate (Acuphase) injection Dental LD List B: Medicines in the APC Formulary used for an unlicensed indication/offlabel approved for use in BCHCFT Name of drug approved in BCHCFT formulary Service Area Indication/Notes Amantadine Amitriptyline Atropine eye drops Azathioprine Beclometasone dipropionate inhaler (Clenil Modulite) Beclometasone dipropionate nasal spray Betamethasone tablet Rehab Dental Rehab Dental Dental Neurostimulant Facial pain Hypersalivation Severe ulcerative conditions Mucosal ulceration and inflammation Oral ulcerative conditions Betamethasone valerate cream and ointment (Betnovate) Bromocriptine Dental Carbamezepine Dental Dental Rehab Dental, Children Oral inflammation and ulceration (used as a mouthwash) Oral ulcerative conditions Neurostimulant in prolonged disorder of consciousness minimally conscious state; Treatment of apathy symptoms after brain injury Facial pain; mood stabiliser Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 10 of 21 Citalopram Children Panic and anxiety Clindamycin capsule Dental Clobetasone butyrate cream and ointment (Eumovate) Clobetasone butyrate/nystatin/oxytetracycline (Trimovate) Colchicine Dental Severe bone infections; antibiotic prophylaxis in oncology patients Oral ulcerative conditions Dental Oral ulcerative conditions Dental Clobetosol propionate cream and ointment (Dermovate) Clonidine Co-careldopa Cyclizine Dapsone Dental Oral ulceration and inflammation Oral ulcerative conditions Dexamethasone injection Doxycycline Erythromycin suspension Fluoxetine Fluticasone propionate spray/nasules Gelclair Hyoscine patch Hydroxochloroquine Hydrocortisone cream with miconazole (Daktacort) Lamotrigine Melatonin (note some products/strengths are unlicensed e.g. Kidnap) Methylphenidate (including Matoride) Midazolam Oromucosal Solution (Buccolam) Mycophenolate Ondansetron injection Oxcarbazepine Children Rehab Dental Dental Dental Dental Rehab Dental Dental Dental Children Dental Dental Dental Rehab, Children LD, Children LD Dental Dental Dental ADHD and Tourettes Neurostimulant Nausea/vomiting Vesiculobullous disorders, Lichen Planus, Linear IgA disease Anti-inflammatory agent Aphthous ulcers Prokinetic agent Facial pain Oral ulcerative conditions Relieve the pain of oral mucositis Drying secretions Oral mucosal inflammatory conditions (Chronic ulcerative stomatitis; Oral Lichen Planus) Oral ulcerative conditions Facial pain Sleep problems in brain injury; sleep problems in children ADHD in adults and children Seizures in adults Lichen Planus, Pemphigus, Pemphigoid, Orofacial granulomatosis under specialist supervision Prevention nausea/vomiting Treatment of trigeminal/ glossopharyngeal neuralgia Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 11 of 21 Paroxetine Phenytoin Pizotifen Prednisolone soluble Dental Dental Dental Dental Facial pain Neuropathic pain Neuropathic pain Oral ulceration & inflammation Pregabalin Dental Trigeminal neuropathic pain Propranolol Children Risperidone oral Sodium valproate Tacrolimus ointment Tocopherol (Vitamin E) Triamcinolone acetonide for injection Trihexyphenidyl Venlafaxine 6. Children Dental, Children Dental Dental Dental Children Dental Anxiety and migraine Aggressive behaviour Facial pain; mood stabiliser Severe ulcerative conditions Osteoradionecrosis of the jaws (in conjunction with pentoxifylline) Oral ulcerative conditions Dystonia (e.g. palsy) Facial pain in cerebral References/Definitions Birmingham, Sandwell, Solihull and environs Formulary Unlicensed use or off label use: licensed medicines used outside the terms of its Marketing Authorisation e.g. medicine licensed specifically for adults but used in children. Unlicensed medicine: medicines that have no Marketing Authorisation (licence) for use in the UK. Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 12 of 21 Appendix 1 Birmingham,Sandwell,Solihull and Environs Area Prescribing Committee DRUG APPLICATION FORM All essential information in support of this application must be attached to this application form with full references provided electronically. Applications from Trust or CCG Medicine Committees should be emailed to the APC Secretary: [email protected] To discuss application enquiries please call the APC Secretary at Midlands and Lancashire CSU who will signpost you to an appropriate pharmacist. Phone: 0121 612 4109 Section 1: Information on the Medicinal Product a) Brand/generic name b) Pharmaceutical form c) Strength d) Administration route e) Dosage/ frequency f) Course length, if applicable g) Manufacturer h) BNF section number i) Licensed indication for use , in the UK j) Proposed indication for use and dose (if different from license) If product is unlicensed or to be used 'off label', provide references to support dosage k) Brief summary of the condition being treated (including morbidity, quality of life and mortality estimates) Section 2: Evidence of Comparative Efficacy a) Is the proposed medicinal product covered by NICE technology appraisal guidance? If so, which? If the answer to section 2a is Yes then please go to section 8 and complete the declarations. If the answer is No then please continue with the rest of the application. b) Report clinical outcomes in preference to surrogate markers; absolute and relative risk/hazard ratios; and numbers needed to treat (NNTs); quality-of-life measures as a minimum, where available: Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 13 of 21 Vs placebo Vs current “best available therapy” Vs other comparators c) What are your views on the efficacy of this medicinal product compared to the available therapy? Please provide the most recent and main peer reviewed papers with relevant supporting literature, including efficacy, safety and cost effectiveness. Cite comparative studies to existing therapies where available. Section 3: Evidence of Comparative Safety & Use a) Please report the incidence of adverse effects in both active and comparator arms of trials, absolute and relative risk increases and number needed to harm (NNHs), where available. b) How does the safety of this proposed drug compare to treatment options currently in use? c) What concerns are there over the safety of this product? List the principal/ significant concerns for each part below: i) Adverse effects ii) Cautions iii) Contra-indications iv) Drug interactions v) Toxicity e.g. narrow therapeutic index vi) Potential for misuse d) How many clinical trials have you assessed for this medicinal product? e) Please indicate approximate number of subjects who have been exposed to the product during high quality clinical trials. Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 14 of 21 f) Were any significant patient groups excluded from clinical trials? g) Are there groups of patients for whom the product is not suitable? h) Please detail any specific pretreatment requirements (e.g. baseline LFT) i) What are the monitoring requirements? j) How and when would you propose to audit/monitor use of the new therapy? k) Who will be responsible for monitoring? l) Would you recommend any prescribing restrictions e.g. microbiological advice, consultant use only? m) Are there any other processes or approval required before use e.g. microbiologists, safety groups? n) Have prescribing guidelines been produced (please attach) or do these need to be developed to support safe implementation of prescribing? o) Will the drug complement existing treatments? If yes, give details p) Please detail any relevant safety concerns in relation to storage/prescribing/preparation/ use/administration/disposal q) What are your views on the adverse drug reactions (ADRs) of this medicinal product compared to the available therapy? Section 4: Proposed position of therapy Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 15 of 21 a) Will the proposed drug replace an existing drug on the formulary? If yes describe why it should be used in preference. b) What are the other treatment options? c) What are the patent expiry dates of the products being replaced by this proposed medicinal product? d) Horizon Scanning: are similar drugs likely to be licensed in the near future? e) Please indicate clearly, where within the current drug treatment pathway/algorithm the product should be used (i.e. Options for 1st/ 2nd/ 3rd tier treatments)? f) Please indicate if there is a subgroup of patients in whom this product has demonstrated particular benefit or would be a preferred option. g) Is this medicine likely to be prescribed in an out-patient setting? h) Is Effective Shared Care Agreement (ESCA) or a Rationale for Initiation, Continuation and Discontinuation (RICaD) required? i) Has MTRAC ESCA Guidance been issued? Confirm the outcome: - Suitable for GP prescribing - Effective Shared Care Agreement (ESCA) required Not appropriate for primary care j) How would a change or implementation of the new therapy be communicated? k) What is your proposed position in formulary? Please mark one response from below: GREEN: Prescribable within primary and secondary care. AMBER: Initiation by specialist, or recommendation for GP initiation by specialist and conditions for safe transfer of Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 16 of 21 prescribing to primary care eg RICAD, ESCA, place for monitoring. RED: These drugs are for specialist prescribing only. Prescribing retained in secondary care and should not be prescribed in primary care. Section 5: Expected level of use and potential expenditure across the Health Community Please provide information for both Secondary and Primary Care settings a) Cost of product per patient per 28 days’ treatment at most common dosage (or other if appropriate – please specify) b) Where appropriate, what is the cost of the product(s) which this will replace - per patient per 28 days’ treatment at most common dosage (or other if appropriate, please specify) Primary Care (use standard drug tariff price or BNF cost): Primary Care (use standard drug tariff price or BNF cost): c) Cost of the product:£per annum, £per treatment course d) Comparative cost of existing treatment £per annum, £per treatment course e) Are there differences in non-drug costs (or savings) associated with use of the new product, for example diagnostic tests, monitoring? f) Estimated number of patients to be treated per annum (based on XXXX population of approx XXXXXX giving consideration to incidence, prevalence and expected place in therapy) population of approximately Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 17 of 21 g) What is the financial cost/saving resulting from the introduction of the therapy?If there is a cost pressure, how will this be funded? h) Can the cost of this be covered by a reduction in expenditure on anything else? Please give details i) Within your area of practice, what else would you like to spend this amount of money on? Which provides the greatest level of benefit to patients? j) Is this medicine excluded from Payment by Results tariff (PbR)? k) Other costs and considerations l) Who will initiate prescriptions? m) Who will undertake maintenance prescribing? n) Is there clinical trial evidence that demonstrates resource benefit? o) If there are comparative trials against the standard therapy: was there an additional benefit/convenience? p) What are your views on the costeffectiveness of this medicinal product compared to available therapy? q) Please confirm the names of local clinical leads in support of this application (in your own or other local Trusts or networks) Section 7: Application Sponsor By signing this application you are confirming that: Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 18 of 21 a) You have agreement from Consultants within your directorate (and if appropriate other directorates who may have an interest in using this product) regarding the proposed place in the treatment pathway of this product as well any proposal you may have made to replace any existing product. b) You will cascade the result of this formulary application to your Directorate colleagues. c) You understand that this application is for formulary approval across Birmingham, Sandwell and Solihull area. d) Your Clinical Director, and/ Directorate Pharmacist support the proposed clinical benefit of this preparation. e) The information supplied is correct to the best of your knowledge at the time of submission. Section 8: Application details and declaration a) Do you wish to attend the APC to discuss application? In person/representative: b) Has the application been discussed and supported by a Multidisciplinary Team (MDT) /other forum within your trust or across the area? To avoid any concern that commercial interests might have influenced your request to the Committee, you must indicate if you have an interest that may influence, or be perceived to influence, your request. c) Do you have any conflict of interest to declare? No - I have no conflict of interest Examples include: - Consultancy with the drug company; - Department receives research funds from the drug company; - Staff within the department are funded by the drug company; - You or your staff receive funding for attendance at scientific meetings from this company Yes - Please give details: Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 19 of 21 d) Has the drug company been directly involved in completing this application? No Yes- Please confirm which companies have been involved and state which sections the drug company has helped to complete: You must fully disclose: clinical trial work; other paid or sponsored research or audit (clinical or non clinical); meeting(s) sponsored in part or whole; meeting attendances paid or sponsored in part or whole; Advisory panel or consulting work or other employment; paid lecturing; gifts, meals, hotel accommodation or other hospitality; any other potential conflict of interest (including shares held). Articles of low intrinsic value, i.e. less than £50, such as diaries or calendars, need not be declared. Modest hospitality, such as meals, does not need to be declared provided that the individual cost per year is less than £50. However, if more than one gift or meal is made from the same or a related source within a 12 month period totalling more than £50, they should be declared. Declaration of funding source should include financial interests over the three years to date, and should include prospectively agreed research income for the next year. Declarations do not distinguish between personal payment and payment to a Trust fund or research account and should include financial association of immediate family members. Circle/ code relationships as follows:i) >£50 and <£5,000ii) £5,000 - £20,000iii) >£20,000 Applicants Details / Counter-signatory Details Name of requesting Clinician: Job title: Department / Specialty: Work base: Signature: Date: Name of sponsoring Clinical Pharmacist: Signature: Date: Name of Finance Lead: Signature: Date: Name of Drugs and Therapeutics Committee Chair (or Medical Director) Signature: Date: Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 20 of 21 Section 9: Decision summary APC to complete Assessment Support Tool and record decision summary Drug application Process & BCHCFT Formulary v1.0 July 2016 Bilkis Islam-Ali (Clinical Training & Policy Development Pharmacist) Page 21 of 21