* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biosafety in Research Laboratories Refresher Training Post-Test
Sexually transmitted infection wikipedia , lookup
Brucellosis wikipedia , lookup
Hepatitis C wikipedia , lookup
Henipavirus wikipedia , lookup
Oesophagostomum wikipedia , lookup
Herpes simplex virus wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Hepatitis B wikipedia , lookup
Marburg virus disease wikipedia , lookup
History of biological warfare wikipedia , lookup
Biological warfare wikipedia , lookup
United States biological defense program wikipedia , lookup
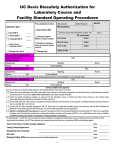
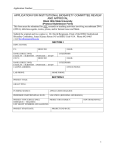
E-Mail Quiz Print Quiz Environmental Health and Safety Biosafety in Research Laboratories Refresher Training Post-Test Name: Title: Department: PI/Supervisor: Work (BLDG/RM): Email: *NOTE* By completing this test, you are confirming that you have viewed the entire training presentation. 1. One of the recognized lab acquired infections (LAI) in the presentation noted a thumb laceration from a scalpel used with a West Nile Virus infected bird. The wound was washed with soap and water. Which of the following should not be done? A. Proceed to Occupational Health Clinic or Emergency Department for treatment. B. Inform your supervisor of the accident. C. Complete the experiment prior to seeking treatment on the same day. 2. You investigated the accident in the above scenario and recommended a change in personal protective equipment (PPE) to help prevent the risk of a similar injury in the future. Which of the following do you recommended? A. The use of Nitrile coated Kevlar gloves B. The use of Solid front, fluid barrier gown C. The use of a N95 mask or other piece of properly fitted aerosol protection 3. Your research, which involves recombinant DNA, is funded by the private Massachusetts Lions Eye Research Fund. Do you need to comply with the NIH Guidelines? A. Yes B. No 4. Which of the following routes of exposure has the potential to lead to a LAI (Laboratory Acquired Infection)? A. B. C. D. E. F. Aerosol inhalation Abrasions Splash to the eyes Mouth pipetting None of the above All of the above Biosafety in Research Labs Refresher Training Test v.2 |2013 5. You are working with baculovirus to express recombinant protein in insect cells. This work must be registered with the Institutional Biosafety Committee (IBC). A. True B. False 6. Human cell lines derived from primary human material are covered by the OSHA Bloodborne Pathogen Standard while human cell lines purchased from the American Type Culture collection (ATCC) or Coriell Institute are not. A. True B. False 7. Which of the following is not part of an Agent Risk Assessment? A. B. C. D. Availability of funding Infectious dose Severity of disease Person-to-person disease transmission 8. Which of the following can disrupt air flow in the biosafety cabinet? A. Two people working simultaneously and independently B. Placing items on the front grille C. A person walking rapidly by the biosafety cabinet (BSC) when someone is working inside D. Having an open flame E. All of the above 9. The LAI (Laboratory Acquired Infection) with Sabia Virus in the presentation may have occurred when the rotor was opened. What can be done to minimize aerosol exposure related to centrifugation? A. Load/unload rotor inside a BSC when the rotor is light enough to move B. Close rotor and centrifuge upon discovering a spill. Place DO NOT DISTURB sign on the centrifuge. Initiate clean up in half an hour. C. Clean up immediately. Someone else is waiting to use the centrifuge. D. A and B 10. The NIH Office of Biotechnology Activities (OBA) requires notification when an exposure involves recombinant DNA even if that exposure does not lead to illness. Which does not need to be reported to OBA? A. A splash to the eye of a recombinant adenoviral vector B. Exposure of a clinical laboratory worker to Muchupo virus when a blood tube breaks in the centrifuge. 2|Page 200 Harrison Avenue, Boston, MA 02111 ι TEL: 617.636.3615 ι FAX: 617.636.2419 Biosafety in Research Labs Refresher Training Test v.2 |2013 11. An ideal container for bags filled with biowaste prior to autoclaving or vendor disposal would be one that has the following characteristics: A. B. C. D. Hard-sided A lid that can be closed when not being used Easily decontaminated All of the above 12. How should biological materials that need to be transported from the lab to the animal facility be handled? A. Transport material in your pocket while wearing a lab coat B. Carry the material in your hands while wearing gloves C. Transport the materials in a sealed leak-proof, shatter resistant primary and secondary container D. Transport the materials in a primary container stored in an open ice bucket 13. A post-doc asks you to ship a slant of Shigella to a colleague at a different University. You will need to: A. Put parafilm on the slant cover, surround it in bubble wrap and put it in a FedEx envelope. B. Find out about Federal shipping training requirements. Classes are listed on the TEHS website. 14. The NIH Guidelines are now applicable to research with synthetic nucleic acids. Which of the following is NOT TRUE? A. The Guidelines recognize that appropriate biosafety containment of an agent is necessary regardless of the technology used the generate the agent. B. The chemical synthesis process is now regulated. C. The Guidelines are applicable only after nucleic acids are placed in a biological system (e.g. cell) D. Synthetic nucleic acids that cannot replicate or do not contain or origin of replication are exempt from the Guidelines. *NOTE* By completing this test, you are confirming that you have viewed the entire training presentation. Return completed test to Tufts EHS ([email protected]). If you are unable to send via email, please print out and send interdepartmentally to: Environmental Health & Safety; Posner 105, 200 Harrison Avenue; Boston To Be Completed By TEHS Staff: Completion Date: 3|Page Expiration Date: Score: 200 Harrison Avenue, Boston, MA 02111 ι TEL: 617.636.3615 ι FAX: 617.636.2419 Biosafety in Research Labs Tufts University/Tufts Medical Center January 2013 Learning Objectives Become familiar with the Regulatory Agencies and Institutional Committees governing use of Biological Material. Understand key elements of Risk Assessment Familiarity with Biosafety Level 1 and Biosafety Level 2 practices and procedures. Recognize biosafety practices and procedures extend to work in the animal facility. Recognize when there is the need to wear Personal Protective Equipment (PPE) and be able to determine what PPE should be worn. Learning Objectives Become familiar with use of Biosafety Cabinet Recognize the risk of using a centrifuge incorrectly and requirements when used with infectious agents. Understand spill response procedures. Review collection, storage, transport and inactivation of biological material Know that shipping research materials requires strict procedures to protect everyone in the transportation chain. Understand your responsibilities when working with biological material. 1 Training Summary Biosafety Related BRL – 3 yrs OSHA BBP annually Shipping – 2 yrs PI Training on NIH Guidelines online Other Areas – Some are Institution Specific TU – General Lab Safety via LearnCenter TMC – HIPAA, BBP for Infection Control Key Links http://www.tufts.edu/central/resear ch/IBC/ (Vice Provost) http://publicsafety.tufts.edu/ehs/ Left column Accident & Incident Reporting Forms Biological Safety Biological Safety References TU/TMC Biosafety Manual The Goal of Biosafety Minimize the risk of exposure to biohazardous agents using: Engineering Controls Work Practice Controls Exposure Response Plans Personal Protective Equipment (PPE) Preventing/minimizing occupational exposure 2 Biohazardous Materials Definition An agent of biological origin that has the ability to cause disease in a human, animal, plant, or insect. Recombinant DNA (i.e. viral vectors) Viruses Bacteria Parasites Fungi Prions Human source material Human cell lines Laboratory Acquired Infections Infections from laboratory-related activities whether symptomatic or asymptomatic Four primary routes of exposure Inhalation of aerosols Percutaneous inoculation (needle and syringe, Contact between mucous membranes and cuts, abrasions and animal bites) contaminated material (hands or surfaces) Ingestion (aspiration through a pipette, smoking or eating or after inhalation) Laboratory Acquired Infections Studies on the incidence of LAIs: Pike and Sulkin Surveyed 4,000 labs 50% response 4,079 LAI from 1935-1978 Harding and Byers 1979-2005 1,141 with 24 deaths 46% clinical labs 50% research labs 3 Causes of LAIs Accidents Failure to apply SOP Failure to Identify Risk Routine work/commonly used agent Misidentification Failure of pre or post preventive measures No immunization None or wrong prophylaxis Majority of Occupational Infections are without known exposure incident LAI -Recognized Exposure West Nile Virus August 2002 and October 2002 Laceration of thumb from scalpel while removing brain tissue from a bird Needle stick when harvesting brain tissue from infected mouse Wounds washed with soap and water immediately after exposure incident 3 days post exposure both individuals developed signs of WNV Both recovered fully within 7 days Old Title vs NIH Guidelines for Research Involving Recombinant DNA Molecules New Title NIH Guidelines for Research Involving Recombinant or Synthetic Nucleic Acid Molecules Implement by 3/3/13 4 Is chemical synthesis covered? synthesizer Not until in a … Oversight of Biohazardous Work NIH Guidelines for work Recombinant DNA http://oba.od.nih.gov/oba/rac/Guidelines/NIH_G uidelines.htm Responsibilities of TU/TMC, IBC, PI, BSO Containment levels for work in tissue culture & animal models Requires notification of Overt Exposures to rDNA handled at BSL-2/ABSL-2 or above IBC review based on Risk Assessment III-D: IBC Approval Prior to Initiation of Work III-E: IBC Notice Simultaneous with initiation III-F: Exempt from NIH rDNA Guidelines III-F Registrations Nothing exempt in Boston Using nonhazardous plasmids (pBR) to clone gene of interest into host (nonpathogenic E.coli) Often the first step in creating a transgenic animal New exemptions for synthetic nucleic acids No origin of replication, no integration… 5 Oversight of Biohazardous Work TU/TMC Institutional Biosafety Committee Review and approval of: Recombinant DNA Human Gene Transfer Clinical Trials (TMC) Infectious Agents Select Agents and Toxins Human Source Material including Human Cell Lines (TU) Develop Exposure Response Plans for Biohazardous Agents Investigation of accidents/exposures with agents IBC Website: http://www.tufts.edu/central/research/IBC/ Registration Form Before work Approval may include NIH Infectious Exempt Deadlines Committee decision sent by IBC office NIH Guidelines: Definition of rDNA Molecules constructed by joining nucleic acids & can replicate in a living cell 6 NIH Guidelines: synthetic Nucleic acids that can base pr w naturally occurring nucleic acids NIH Definitions Continued Molecules resulting from replication of rDNA or synthetic nucleic acids in past two slides Other Changes AAV serotypes needing review Transfer of drug resistance traits Human Gene Transfer w nucleic acids 7 Guidelines Relevance Research performed at or sponsored by Tufts due to receipt of funds Term & condition of NIH funding Noncompliance – suspension, limitation etc Oversight of Biohazardous Work OSHA Bloodborne Pathogen Std 42 CFR 1910.1030 (www.osha.gov – B) Compliance required for all work with Bloodborne Pathogens or OPIM. BBPs: Capable of causing Human Disease: HBV HCV HIV Human Source Material / Human Cell Lines Transmitted by direct contact Annual training No charge Researchers Use Human cell lines & materials 1o human material ATCC: ATCC Biosafety Level is specific for DOT transportation requirements and not the BSL that the human cell lines should be used at. Key points screening/testing viral inactivation 8 ATCC Example CCL-2 aka HeLa Products: keratin Comments: human papillomavirus 18 sequences cause of cervical cancer most cases clear w/o med. intervention Biosafety Level: 2 OSHA BBPs and Universal Precautions An Approach to Infection Control all blood & tissues are guilty assumed to carry disease no way to assure complete absence Body Substance Isolation/Standard Precautions Exposure Control Plan access and updates Hepatitis Signs/Symptoms None B – 30% C – 80% Jaundice Fatigue Loss of appetite Yellowness of skin / eyes/body fluids due to deposition of bile pigment from excess bilirubin hemolytic anemia gallstones alcoholic cirrhosis 9 Bloodborne Pathogen - HBV Hep B Virus and Vaccine Virus infective after drying on surface Blood Wound exudates Due to childhood vaccination (1991) ~95% new infections in adults Booster not recommend w/ normal immune status Consider if suppressed Occ Exposure HBIG Bloodborne Pathogen - HCV Most common chronic BBP infection in the US Seroconversion - infected sharps ~1.8% Rare with mucous membrane exposure Survive and transmit for 6 hours but not longer than 4 days No vaccine 10 Bloodborne Pathogen - HCV Long term effects chronic infection: 75-85% chronic liver disease: 70% leading indication for adult liver transplants Treatment Expect genotyping Waiting 12 weeks to begin treatment allows for more spontaneous resolution than 6 months Combo therapy w/ pegylated interferon and ribivarin-30-40% resolve + protease inhibitors approved 5/2011 ~75% 12/11 CDC symposium – can we improve screening with more effective drugs? Bloodborne Pathogen - HIV 6/5/81 MMWR 5 previously healthy gay men pneumoncystis pneumonia Within yr Within 2 yrs Called AIDS Agent ID - HIV Bloodborne Pathogen - HIV Risk after percutaneous injury 0.3% mucous membrane exposure 0.09% PEP (post exposure prophylaxis) HAART(highly active antiretroviral therapy) Suppresses viral replication for decades Less infective to others Drug therapy 1995 1997-1998 Decline in diagnoses and deaths began leveling in 1999 11 LAI - Known Exposure Human colonic adenocarcinoma 1986 Percutaneous injury to hand from needle used for the injection of human cancer cell line into an animal 19 year old with no identified immune deficiencies Sustained growth of tumor nodule http://www.nejm.org/doi /pdf/10.1056/NEJM19861 2043152314 Exposure - Transplant Transmission (2002) Kidney – 50 yr old F, stroke; recip – 37 yr old M, diabetic Autopsy after transplant CDC- 1% organ suspected of disease trans Local Oversight of Biohazardous Material MA Department of Public Health Boston Public Health Commission Biohazardous Waste Disease Surveillance BPHC Lab Regulation Boston Fire Department Ordinance for Research Labs 12 The Risk Assessment Agent Review Key to safe use of biological material before work with biological agent performing new technique New equipment Combined effort of PI, Lab employee, Biosafety Officer, and IBC Severity of disease Transmission Infectious Dose Incubation period Signs and Symptoms of Disease Increased susceptibility PPE to lower exposure Exposure response Procedures Risk Assessment & Synthetics % of genome from each parent Fn/purpose of each sequence Assume same fn as original host? Synergism between sequences & transgenes What’s a Biosafety Level? Risk Assessment End Result A combination of Laboratory practice Safety equipment Facility design Biosafety Levels 1-4 defined in BMBL 5th Ed NIH Guidelines Risk Groups 1-4 defined in NIH rDNA Guidelines. 13 Biosafety levels BL1: Organisms that are not associated with disease in healthy human adults. Don’t eat it BL2: Organisms associated with human diseases which are rarely serious and for which preventive or therapeutic interventions are often available. Don’t touch it Examples BL1 BL2 yeast two hybrid pBR & pUC based plasmids K12 based E. coli nonpathogenic helper free adenoassociated virus pathogens Borrelia viral vectors Retrovirus/len tivirus BBP material NHPrimate material Oncogenes BL1 Lab design 14 BL1- Highlights Lab designed to be easily cleaned Each lab has a sink for hand washing 1. after using rDNA materials 2. before leaving the lab Work surfaces decontaminated once a day and when spills occur Usual disinfectant? No eating, drinking, food storage BL2: Lab Design BL2-Highlights All BL1 Facilities/Practices & more stringent control of lab access, processes and waste Doors closed and posted Autoclave / disinfect waste Report spills, accidents, potential exposures. Minimize the creation of aerosols. All equipment contained in the room as much as feasible. 15 Animal Biosafety Don/doff PPE Decon of work area Transporting & handling animals Work with sharps Engineering Controls Isolate or remove In - syringes, razor blades, contam. glass No – chucks, pipette wrapper ¾ full Plastic/mylar coated capillary tubes Optimizing Engineering Controls “Single most useful piece of equipment for prevention of lab acquired infections.” Pike Annual inspection Air flow keep grilles clear no whooshing recycle - not for chems 16 BSC Film Clips Engineering - The Biosafety Cabinet Design Protecting air flow Bsc is designed to be used by only 1/X Daily practices Other poor practices in previous slide Total Exhaust BSC Primarily for toxic chemicals & biologic work Depends on building exhaust Energy savings problems HNRCA 17 Engineering - BSC - Organize Liquid Waste Practices Chemically disinfect 10% mercury free bleach Less than a week old Chlorine concentration Wait 20 minutes Pour down drain Secondary Containment Nonporous Holds entire contents 18 Centrifugation – Avoid Aerosols Wipe down outside of sealed rotor or safety cup w/ disinfectant before removing from BSC Double Barrier Prevent the release of aerosols Environmental contamination is an effective method of disease transmission Avoid Mechanical Failure Centrifuges are designed to contain the rotor in event of a failure Documented rotor failures Personnel injury Property damage 19 Centrifuges Rotors Stress from centrifugal force Fatigue – stretching and relaxing causes cracks Exp or safe service dates Corrosion User error causes many malfunctions Secure rotor lid Secure rotor to drive Improper balancing Overloading Buckets can’t swing freely Open in BSC LAI - Without Recognized Exposure Sabia Virus Purification: Yale 1994 6 x 250 ml screw cap bottles w/ O-Ring, sealed rotor Rotor opened – one bottle wet & liquid pooled at the bottom of rotor No obvious bottle breakage PPE – solid front disposable gown, gloves (double during clean up), and surgical mask Exposure likely occurred via inhalation of aerosol when rotor was opened or during decon PAPR was available but not used Initially BL3; now BL4 Biological Spills Assist injured/exposed Notifications if necessary Limit access to area Don PPE, gather supplies Ring spill with absorbent Cover with more absorbent & disinfect Clean up Disinfect area again Dispose of materials 20 Broken Glass in Spills Spill Kit • Basic •Paper towels •Concentrated disinfectant •Expanded •Caution •Other tape items •Assemble rather than purchase Work Practice Controls W - reduce exposure risk by changing task performance 21 Work Practices per Mom & OSHA Immediately after removal of gloves or other PPE Limited circumstances ok for antiseptic hand cleanser / towellettes Most not effective vs. adenovirus WP- Medical and Biological Waste Waste causes /contributes to an increase in mortality, increase in serious irreversible or incapacitating reversible illness Pose substantial potential hazard to human health or the environment when improperly treated, stored, transported, disposed of, or otherwise managed Examples: Cultures and Stocks of Agents and their associated Biologicals, Pathological Waste, Contaminated Animal waste, Sharps, Biotechnology effluents, Blood and Blood products Treatment Options Onsite Chemical liquids Autoclave Offsite Packaged and Transported R Med Waste Approved vendor TU/TMC differences Decontamination – reduction or removal so safe to handle 22 Storage Closed and flyproof Secondary containment for transport to autoclave Bag must be open for steam penetration Autoclave Operations Each Load/Cycle must be Evaluated Calibrated Annually by Trained Individual Quarterly Qualitative (growth/no growth) Biological Challenge Testing Test each Cycle if BSL-3/ABSL-3 Waste Method Approved by IBC Record-Keeping Log Autoclave Explosion 23 Autoclave PPE/Practices Heat resistant gloves Keep your Face away from the door Long Pants Protective footwear Focus on PPE Protect others Soiled/used lab clothing is autoclaved before laundering? Am J Inf Contol 9/2011 ABC New – neckties 24 At the request of your colleagues “Staged” poor fit with alternatives Exposure Response Plans Some ERPs available on the IBC website Review with all staff prior to work Key information: Background information on agent. Signs and symptoms of disease. Pre-exposure Health Screening Actions Before an Exposure Incident Action immediately after exposure incident Medical Evaluation and Follow up 25 Exposure Documentation First Report of Injury / Supervisors Accident Report / Employee Incident Report workers compensation forms on the EH&S website TMC intranet, EHO, BSO TU FUP @ recommended intervals Update OSHA 300 log if later diagnosed with BBP disease Post Incident Reporting Biosafety Officer is notified of any incident, accident, or exposure involving rDNA NIH notification Report Overt exposure or release into the environment of any rDNA at BL2 or above Minor incidents within 30 days Response made Prevention of a reoccurrence IBC Notification NIH Notification made by Office of the Vice Provost Transport of Biohazardous Material Trained & certified prior to offering specs for transport Includes Dry ice Infectious Sub. Animal & human Genetically modified org formalin IATA vs. DOT 26 Select Agents and Toxins (SATs) Department of Health & Human Services (DHHS) regulates the possession, use and transfer of Select Agents and Toxins SATs considered to have the capability of being used by a terrorist to negatively impact human, animal, and plant health Latest changes involve “tiering” Effective 12/12 (published 10/5/12) Overall reduction in # of agents Select Agent Ripples Work subject to SA maybe not NIH Guidelines Vendors requesting proof you allowed to possess esp w synthetics Ricin 100 mg Staph Entero 5 mg Visits Annually Active participation – usually scheduled Scope of work as described in BMR Best practices Regulatory changes 27 LAI - Without A Recognized Exposure Tularemia Boston University 2005 3 Lab employees infected Believed using Francisella tularensis LVS at BSL-2 Really wt F. tularensis –a BSL-3 agent Investigation cited failure of several safety practices. Strong argument for confirmatory testing of high risk agents prior to use at BSL-2 Now for the Quiz! This quiz is needed to document that you have completed and understand all sections of this training. A passing score of 80% is required. A Certificate of Training will be sent to you if the test was passed. Please be sure to keep this certificate for your records. 28