* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download neck infection File - Ain Shams University
Hepatitis C wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Trichinosis wikipedia , lookup
Neonatal infection wikipedia , lookup
Herpes simplex wikipedia , lookup
Onchocerciasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Marburg virus disease wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Typhoid fever wikipedia , lookup
Gastroenteritis wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Oesophagostomum wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
Antibiotics wikipedia , lookup
Hepatitis B wikipedia , lookup
Rocky Mountain spotted fever wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Schistosomiasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Neck Infections
Magdy Amin Riad
Professor of Otolaryngology . Ain Shams University
Senior Lecturer in Otolaryngology. University of Dundee
Etiology
•
Infectious
– Viral:Adenovirus, Epstein Barr
virus, Coxsackie A, Herpes
simplex
– Bacterial: Group A Strep, other
Streptococci, Mycoplasma,
Fungal: Candida
•
•
•
•
•
•
•
Peritonsillar abscess
,Parapharyngeal
abscess,Retropharyngeal abscess
Neoplasm
Gastric Reflux
Mouth-breathing
Smoking
Sinusitis
Foreign Body
Sore throats
Pharyngitis
infective
viral : herpetic, influenza, HIV
fungal : candida
non-infective
fumes, smoking
nasal obstruction
reflux
leukaemia
foreign body
Sore throats
• Tonsillitis
• bacterial : strep (gonococcus, diphtheria)
• viral : EBV
• Epiglottitis
• Neoplasm
• Post tonsillectomy
Tonsillitis
• Acute
• Recurrent acute
• Chronic (?)
Pharyngitis and Tonsillitis.
• Most sore throats are caused by viruses and thus
don't require antibiotics.
• Acute tonsillitis and pharyngitis present with
throat pain that may radiate to the ears and
dysphagia.
• Fever is more commonly associated with group A
beta-hemolytic streptococci (Streptococcus
pyogenes), which accounts for about 15% of all
cases.
Pharyngitis and Tonsillitis.
• The proportion of pharyngitis and tonsillitis
that is cause by group A streptococci is
related to the patient's age.
• In children 6 to 15 years of age,
approximately 50% of the pharyngitis that
presents for care is caused by streptococci.
Classic streptococcal symptoms
• include sore throat, dysphagia, fever,
malaise, and headache in the absence of
other URI symptoms.
• Occasional patients will have abdominal
pain and vomiting.
• Signs include exudative erythema, palatal
petechiae, and tender anterior cervical
adenopathy.
Other causes of exudative
pharyngitis
• include Mycoplasma, Epstein-Barr virus,
adenovirus, influenza virus,
Arcanobacterium hemolyt-icum, gonococcal
pharyngitis,
Noninfectious causes of
Sore throat
• include mouth-breathing secondary to nasal obstruction (as with a
URI).
• Mouth breathing classically presents as a sore throat that is worst in the
morning and abates as the day progresses.
• carotidynia, an ill-defined entity characterized by tenderness over the
carotid artery, painful swallowing, and pain radiating to the ears.
• Carotidynia will respond to NSAIDs; antibiotic treatment is not
indicated.
• Consider adult epiglottitis in the febrile adult with severe sore throat,
trouble in swallowing and anterior neck tenderness.
• Also consider peritonsillar abscess.
Acute tonsillitis - investigations
• FBC
– WCC : lymphocytes, neutrophils
• Glandular fever screening test
– eg Monospot
• Microbiology (?)
– swab, pus aspirate
• CT (?)
• Tonsil biopsy (??)
Testing for streptococci.
• Rapid streptococcal tests demonstrate a
sensitivity of approximately 95%.
• Avoid false negatives with proper sampling
technique (i.e., vigorous samples of both
tonsils and posterior pharynx while
avoiding the uvula and soft palate as they
dilute the sample).
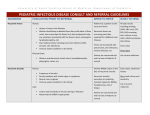
Who to treat.
• The central question in pharyngitis is
deciding which patients require antibiotics
and doing so in a cost-effective manner
keeping in mind antibiotic resistance.
Adults.
• A reasonable approach in adults is to treat
all patients with fever, systemic symptoms,
and tonsillar exudate with antibiotics
because they are likely to have
streptococcal pharyngitis.
Adults.
• Patients exhibiting little or no evidence
suggestive of bacterial pharyngitis (those
with concurrent URI symptoms, obvious
cause such as mouth breathing, little or no
visual evidence of pharyngitis, absent
adenopathy) may be reassured and treated
symptomatically with lozenges or
addressing the underlying problem
(humidity, nasal congestion, etc.).
Adults.
• Streptococcal cultures or quick
streptococcal tests can be reserved for those
patients in whom the diagnosis is not clear
or has an intermediate probability.
• Testing for mononucleosis can be reserved
for those with appropriate adenopathy and
those who do not respond to conservative
treatment
Children.
• Antibiotics should NOT be given in the absence
of a definite diagnosis. This selects for resistance,
carries a risk of allergy, and creates unnecessary
cost.
• Antibiotics started within 9 days of onset are
effective in preventing renal failure and rheumatic
fever.
Children.
• Many clinicians advocate empiric therapy
with antibiotics and systemic analgesia
while awaiting culture results.
• quick streptococcal test followed by a
pharyngeal culture for group A betahemolytic streptococci if the quick
streptococcal test is negative.
Complications of tonsillitis
•
•
•
•
•
Peritonsillar cellulitis
Peritonsillar abscess (quinsy)
Parapharyngeal abscess
Cervical node abscess
Airway obstruction
• Recurrent / chronic tonsillitis
• Tonsillolith formation
Acute tonsillitis - treatment
• Antibiotics
– eg penicillin (NB not amoxycillin/augmentin)
•
•
•
•
Analgesia
Fluids
Steroids (?)
Surgery
– drainage of pus
– tonsillectomy
Treatment.
• Treat for entire 10-day course.
• Clinical/bacteriologic cure >90% (shorter courses
less effective).
• There are no isolates of group A beta-hemolytic
streptococci that are penicillin resistant. However,
there are some isolates resistant to macrolides
• Some resistance to treatment may be noted if the
patient is simultaneously colonized with H.
influenzae that is beta-lactamase producing.
Treatment.
• The first drugs of choice are penicillin (that is, Pen-VK
500 mg PO BID or TID or Penicillin G Benzathine 1.2
million U IM in adults, 600,000 U IM in children)
• Erythromycin 250 to 500 mg PO Q6h for 10 days.
• Consider amoxicillin for young children since it is more
palatable.
• If these fail, a first-generation cephalosporin (such as
cephalexin 250 mg PO QID or 500 mg PO BID) may be
used.
• Alternatives include amoxicillin/clavulanate, azithromycin,
clarithromycin, cefixime, cefuroxime and clindamycin
Indications for tonsillectomy
• Recurrent acute tonsillitis
– 6 in 1 year
– 4 per year for 2 years
(depending on age and severity)
• Obstruction
– OSA, airway obstruction (acute)
– Dysphagia, speech difficulty
• Recurrent quinsy
• Biopsy
Supportive measure
1. Supportive measure: rest, fluids, analgesics, Tantum oral
rinse
2. Return for reassessment in 48 hrs if no better
3. Children may return to school after 72 hours of therapy.
4. Suggest that patients obtain a new toothbrush since strep
can be harbored on toothbrushes and lead to recurrent
disease.
5.Treating other family members empirically is controversial.
When to treat with antibiotics?
• Tonsillar exudate
• Enlarged anterior cervical nodes
• Fever > 38oC
Infectious Mononucleosis
Etiology
• Epstein Barr virus
Clinical course
•
•
•
•
Incubation period: 4-8 weeks
Prodrome: Malaise, anorexia, fever
Few days later: Pharyngitis and lymphadenopathy
Signs:
–
–
–
–
Fever up to 40oC in 90%
Cervical lymphadenopathy in 90%
Pharyngitis in most, exudative commonly
Maculopapular eruption with ampicillin in 90% of those to whom it's
given
– Splenomegaly in 50%
– Others: hepatomegaly, palatal petechiae, rash, periorbital edema (not
common)
• Course: Pharyngitis lasts 7-10 days, Lymphadenopathy 7-14 days,
Malaise 4 weeks or more
Diagnosis.
• Diagnosis is by CBC revealing a lymphocytosis with
atypical lymphocytes.
• This will be present in most of the mono syndromes.
• A positive heterophil antibody (monospot test) may or may
not be present in the early stages of the disease (only 60%
by 2 weeks) but will eventually become positive in 90% of
young adults.
• The heterophil test rarely becomes positive in those <5
years of age.
• If there is any doubt, an EBV antibody titer can be
performed.
• Liver enzymes are almost uniformly elevated.
Heterophil negative mononucleosis
• the same symptoms may be caused by other
organisms including CMV, Toxoplasma, acute
HIV infection, or leptospirosis.
• Mononucleosis is most common in young adults,
and most of the adult population has had clinically
inapparent EBV disease as evidenced by antibody
titers.
• If patients with mononucleosis are treated with
ampicillin or similar drug, they will almost
uniformly develop a morbilliform rash.
• Rarely EBV may cause genital ulcerations
Lab investigations
• Heterophile antibodies (Paul Bunnell or
Monospot tests)
• Atypical lymphocytosis
• Elevated hepatic transaminases
Complications
• Hematologic: autoimmune hemolytic
anemia, thrombocytopenia
• Hepatitis
• Splenic rupture (no contact sports for 8
weeks after onset of illness)
• Neurological: Cranial nerve palsies,
encephalitis
• Airway obstruction
Treatment
• Treatment is symptomatic, and the illness
generally resolves within 2 weeks.
• Supportive (rest, analgesics, antipyretics, fluids,
etc.)
• Steroids for: airway obstruction, autoimmune
hemolytic anemia/thrombocytopenia . prednisone
has been shown to reduce the length of the illness.
Treatment
• A steroid burst of 30 to 60 mg of prednisone PO per day
for 3 days or 4 mg of methylprednisolone PO TID for a
week may be used but should be reserved for treating the
complications of mononucleosis, including respiratory
obstruction, myocarditis-pericarditis, aseptic meningitis,
and hemolysis-thrombocytopenia.
• Contact sports or activities producing other forms of
trauma should be avoided because of the risk of splenic
rupture.
• Spontaneous rupture can occur in 0.1%-0.5% of
documented mononucleosis
Peritonsillar Abscess (Quinsy)
• Unilateral peritonsillar
suppuration, predominantly
between tonsillar capsule and
muscular wall of pharynx
(superior constrictor)
• Pushes the uvula across the
midline.
• Trismus (masseter spasm so
they can't open their mouth).
Clinical Features
Typical picture:
• Unilateral throat pain, dysphagia, drooling,
muffled voice ("hot potato" voice), and
fever
• sore throat not resolving despite antibiotics
• Not necessarily associated with recurrent
tonsillitis (only 30% have history)
Diagnosis
• Pus can be aspirated with a needle
• Pus can be visualized with CT scan or
intraoral ultrasound (neither is used
routinely, except in excluding other
conditions or assessing spread of
suppuration )
What causes it?
• Typically a mixed bacterial infection, most
common species are Bacteroides (anaerobe)
and Streptococci (aerobe).
Management
The 3 main methods are:
• 1. Needle aspiration of pus
• 2. Incision and drainage
• 3. Abscess Tonsillectomy (either unilateral or
bilateral)
• 4. Antibiotics (penicillin + flagyl ) or
Clindamycin since anaerobes are so common).
• 1. and 2. are often combined with tonsillectomy
several weeks later (once acute infection is
resolved).
1. Needle aspiration
• Pro: Easy to do, safe and Inexpensive;
Requires only local anesthesia; >90%
resolution rate
• Con: Up to 15% require 2nd aspiration to
resolve; Requires patient cooperation
2. Incision & drainage
• Pro: Requires only local anesthesia; Get
wider drainage than needle aspiration
• Con: Increased morbidity over needle
aspiration;
3. Abscess Tonsillectomy
• Pro: Get complete drainage; Prevents
recurrence; Fewer days of morbidity than if
tonsils are removed after resolution of acute
infection; Literature shows no increased
morbidity over elective tonsillectomy (ie:
blood loss, complications are comparable)
• Con: require experienced surgeons;
difficulty intubating
Prognosis
• 15% recur, and these are typically young
(age 16-30) and have a history of recurrent
tonsillitis
For recurrent disease
streptococcal disease
• Attempt to identify carrier in family with
throat and nasal cultures.
• Treat any identified carriers.
• Consider IM treatment to rule out
noncompliance as a reason for treatment
failure.
• Change all toothbrushes.
Scarlet fever.
• Scarlet fever is a self-limited systemic manifestation of
streptococcal pharyngitis.
• Symptoms include "strawberry tongue" (a red tongue with
red or whitish papillae), a fine "sandpaper" rash that
appears as a diffuse erythema beginning and concentrating
in the skin folds (especially axillary) but spares the palms
and soles.
• Frequently, there is circumoral pallor.
• A fine desquamation that begins on the fingers and toes
may occur.
• The differential diagnosis includes Kawasaki's disease.
Tonsillectomy
Indications
1. Obstructive tonsils: associated with sleep apnea, dysphagia, speech defects, failure to
thrive
2. Recurrent sore throats
–
–
–
6 sore throats in 1 year
4 in each of 2 years
3 in each of 3 years
Associated with:
–
–
–
–
Fever > 38oC
Swollen anterior cervical nodes
Tonsillar exudate
or Positive Strep culture
Key feature: recurrent sore throats which have significant impact on patient's life:
lots of missed time from work or school, association with febrile seizures,
development of multiple antibiotic allergies, development of Strep complications
etc.
3. Suspicion of tonsillar cancer
Tonsillectomy
• Patient is laid supine and operator sits at head of
bed
• Inserts mouth gag
• Grasps tonsil with a tenaculum, retracts it
medially, and dissects it from tonsil bed
(constrictor muscles)
• Hemostasis in tonsil bed (various methods:
cautery, pressure, ligatures, etc.)
• Suctions clear oropharynx
Complications
1. Hemorrhage (most common complication; estimated at 23%)
–
–
–
–
Intra-op
Primary (within first 24 hrs)
Secondary (between 24 hrs and usually at most 10 days)
Treatment of bleeds:
1. Local pressure with towel holder and gauze (can use
epinenephrine on gauze)
-Hold for 10-20 minutes
2. Chemical or electric cautery
3. Cold water rinses
4. Start IV fluid and antibiotics
Complications
2. Dehydration (common in kids who won't
eat due to pain)
3. Weight loss (also common in kids who
won't eat due to pain)
4. Fever (not common: usually related to local
infection)
Complications
5. Post-op airway obstruction (due to edema,
hematoma, aspirated material)
6. Local trauma to oral tissues
7. Tonsillar remnants
8. Death (uncommon; usually related to
bleeding or anesthetic complications)
Post-op Care
1. Pain control
2. Hydration
3. Adequate diet
There's no evidence that a special diet is required;
obviously soft foods will go down easier
4. No smoking (delays healing)
5. No heavy lifting/ exertion for 10 days (associated with late
hemorrhage)
6. Warn patients that pain will first abate over 5 days or so,
then will increase for a day or 2 before completely
disappearing (related to eschar separation)
Bacterial Cervical Adenitis
• Tender, enlarged nodes
• Organisms- Staphylococcus, Group A
Streptococcus
• Treatment- Beta-lactamase resistant
antibiotic
• Fine Needle Aspiration
Infectious and Inflammatory Lesions
• 40% of infants have palpable LAD
• 55% of pediatric patients.
• Most commonly involving the
submandibular and deep cervical nodes.
Branchial Cleft Cysts
Branchial Cleft Cysts
• Branchial cleft anomalies
• 2nd cleft most common (95%) – tract medial
to cnXII between internal and external
carotids
• 1st cleft less common – close association
with facial nerve possible
• 3rd and 4th clefts rarely reported
• Present in older children or young adults
often following URI
Branchial Cleft Cysts
• Most common as smooth, fluctuant mass
underlying the SCM
• Skin erythema and tenderness if infected
• Treatment
– Initial control of infection
– Surgical excision, including tract
• May necessitate a total parotidectomy (1st
cleft)
Thyroglossal Duct Cyst
Thyroglossal Duct Cyst
•
•
•
•
•
Most common congenital neck mass (70%)
50% present before age 20
Midline (75%) or near midline (25%)
Usually just inferior to hyoid bone (65%)
Elevates on swallowing/protrusion of
tongue
• Treatment is surgical removal (Sis trunk)
after resolution of any infection
Aphthous Ulcers
• Aphthous ulcers are recurrent painful
lesions of non-keratinized mucosa that vary
in size and may appear as solitary lesions or
in clusters (herpetiform ulcerations).
• The typical appearance is of an
erythematous periphery with a white or
yellow depressed center.
• Healing within 10 to 14 days is the rule.
Aphthous Ulcers
Causes.
• Viral (coxsackievirus, herpesvirus),
• systemic illness (Crohn's disease, lupus, Behçet's
disease, erythema multiforme),
• toothpaste (sodium lauryl sulfate),
• stress, and smoking.
• Dental trauma,
• vitamin B12, folate, and iron deficiency have also
been implicated in some cases.
Treatment.
• Symptomatic relief can be obtained by the use of
diphenhydramine elixir as a mouth rinse that is not
swallowed.
• Alternatively, viscous lidocaine 2% can be used in
the adult.
• This may suppress the gag reflex, however, and
may result in systemic toxicity in children.
• The application of a topical steroid (triamcinolone
as 0.1% in Orabase) or steroid mouth rinse
(betamethasone syrup) may accelerate recovery.
Treatment.
• Herpetiform ulcerations may respond to
tetracycline syrup, which is used as a mouth rinse
and then swallowed.
• oral prednisone may be required in some cases.
• A mixture of nystatin 12,500 U, diphenhydramine
1.25 mg, and hydrocortisone 0.25 mg/ml has been
used as a "shotgun" solution. Some also include
tetracycline syrup in the mixture.
Herpes simplex virus
• infrequently causes recurrent intraoral herpes.
• The lesions occur as a cluster of vesicles that
rupture leaving superficial ulcerations that remain
for 3 to 10 days.
• Keratinized tissues, attached gingiva, and the hard
palate are often involved, and such features
distinguish herpes from aphthous ulcers.
• Treatment with acyclovir may decrease healing
time.