* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download JNC 7 Organizational Structure - Karachi Institute of Heart Diseases
Survey
Document related concepts
Transcript
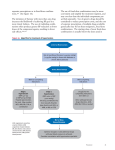
Current Concepts in Pharmachotherapy in Hypertension Brig Afsar Raza FCPS (Medicine), FCPS( Cardiology), MRCP(UK), CCST Cardiology (UK) Commandant Army Cardiac Centre Consultant Cardiologist & Physician Army Cardiac Centre Lahore Pakistan Hypertension : High Prevalence & Growing Incidence in Pakistan • Accounts for over 100,000 deaths a year or 12% of all cause mortality . • Overall 18% of adults in Pakistan suffer from hypertension: 21.5% in urban areas and 16.2% in rural areas. • One in every 3 adults over age 45 suffer from hypertension. • Very few Pakistanis with hypertension (<3%) have their B.P controlled. PROCOR: 7/25/99 The National Health Survey in Pakistan published in 1998 by (PMRC) Levels of blood-pressure control in different countries: Only 3% controlled in Pakistan Percent of Patients Controlled * 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% US Germany Finland Spain Australia * Controlled defined as <140/90 mm Hg; other countries <160/95 mm Hg J Hum Hypertens 1997;11(4):213-220 ** 3% controlled: Data from Pakistan Hypertension League Scotland Canada India England Pakistan** Benefits of Lowering BP Average Percent Reduction Stroke incidence 35–40% Myocardial infarction 20–25% Heart failure 50% Benefits of Lowering BP Heart Failure Reduction: 50% Stroke Reduction: 35-40% 5 MI Reduction: 20-25% Ref : EWPHE, LANCET, 1985; 1349-1954 SHEP, JAMA’ 1991; 265: 3255-3264 To Prevent Target Organ Damage Heart • Left ventricular hypertrophy • Angina or prior myocardial infarction • Prior coronary revascularization • Heart failure Brain • Stroke or transient ischemic attack Chronic kidney disease Peripheral arterial disease (PVD) Eye: Retinopathy Benefits of Lowering BP In stage 1 HTN and additional CVD risk factors, achieving a sustained 12 mmHg reduction in SBP over 10 years will prevent 1 death for every 11 patients treated. Goals of Therapy Reduce CVD and renal morbidity and mortality. Treat to BP <140/90 mmHg or BP <130/80 mmHg in patients with diabetes or chronic kidney disease. Achieve SBP goal especially in persons >50 years of age. 8 Blood Pressure Classification BP Classification SBP mmHg BP mmHg Normal <120 and <80 Prehypertension 120–139 or 80–89 Stage 1 Hypertension 140–159 or 90–99 Stage 2 Hypertension >160 or >100 Treatment Overview Goals of therapy Lifestyle modification Pharmacologic treatment • Algorithm for treatment of hypertension Followup and monitoring Is it just BP control which is required or ...... Traditional Treatment Approach New Treatment Approach Hypertension systemic disease Hypertension disease of blood vessels Hemodynamics altered Vascular biology altered Treat Blood Pressure Control BP & Treat vasculature (Endothelium) CV Risk Factors affect Prognosis & Guide Treatment (JNC 7 Report) >95% of hypertensives have Other CV risk factors* High-risk Hypertension 95% •Cigarette smoking •Obesity •Physical inactivity •Dyslipidemia •Diabetes mellitus •Microalbuminuria or estimated GFR <60 mL/min •Age (>55 years for men, >65 years for women) •Family history of premature CVD Hypertension with CV risk factors: Patients highly vulnerable for JAMA, target JNC 7 Report Mayorgan 21, 2003-damage Vol 289, No. 19 *Stern N, et al. J Intern Med. 2000;203-210 Identifiable Causes of Hypertension Sleep apnea Drug-induced or related causes Chronic kidney disease Primary aldosteronism Renovascular disease Chronic steroid therapy and Cushing’s syndrome Pheochromocytoma Coarctation of the aorta Thyroid or parathyroid disease Lifestyle Modification Modification Weight reduction Approximate SBP reduction (range) 5–20 mmHg/10 kg weight loss Adopt DASH eating plan 8–14 mmHg Dietary sodium reduction 2–8 mmHg Physical activity 4–9 mmHg Moderation of alcohol consumption/Smoking 2–4 mmHg Classification and Management of BP for adults BP classification Normal SBP* mmHg DBP* mmHg Lifestyle modification <120 and <80 Encourage Initial drug therapy Without compelling indication Prehypertension 120–139 or 80–89 Yes No antihypertensive drug indicated. Stage 1 Hypertension Yes Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination. Yes Two-drug combination for most† (usually thiazide-type diuretic and ACEI or ARB or BB or CCB). Stage 2 Hypertension 140–159 or 90–99 >160 or >100 *Treatment determined by highest BP category. †Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension. ‡Treat patients with chronic kidney disease or diabetes to BP goal of <130/80 mmHg. With compelling indications Drug(s) for compelling indications. ‡ Drug(s) for the compelling indications.‡ Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed. Special Considerations Compelling Indications Other Special Situations •Obesity and the metabolic syndrome • Peripheral arterial disease • Hypertension in older persons • Postural hypotension • Hypertension in women •Hypertension urgencies and emergencies Compelling Indications Compelling Indications for Individual Drug Classes Compelling Indication Initial Therapy Options Clinical Trial Basis Heart failure THIAZ, BB, ACEI, ARB, ALDO ANT ACC/AHA Heart Failure Guideline, MERIT-HF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, ValHEFT, RALES Postmyocardial infarction BB, ACEI, ALDO ANT High CAD risk BB, ACE, CCB ACC/AHA Post-MI Guideline, BHAT, SAVE, Capricorn, EPHESUS ALLHAT, HOPE, ANBP2, LIFE, CONVINCE Compelling Indications for Individual Drug Classes Compelling Indication Initial Therapy Options Clinical Trial Basis Diabetes ACE, ARB, CCB , THIAZ, NKF-ADA Guideline, UKPDS, ALLHAT Chronic kidney disease ACEI, ARB, CCB NKF Guideline, Captopril Trial, RENAAL, IDNT, REIN, AASK Recurrent stroke prevention ACEI,ARBs, THIAZ, PROGRESS Other Special Situations Hypertension in Older Persons More than two-thirds of people over 65 have HTN. This population has the lowest rates of BP control Threshold for treatment Diastolic > 90mm Hg and systolic > 150-160 mm Hg over 3-6 months observation(despite life style intervention) Lower initial drug doses may be indicated to avoid symptoms Thiazide or CCB(Dihydroyridine). ACE or ARB may be added Postural Hypotension Decrease in standing SBP >10 mmHg, when associated with dizziness/fainting, more frequent in older SBP patients with diabetes, taking diuretics or venodilators drugs. BP in these individuals should be monitored in the upright position. Avoid volume depletion and excessively rapid dose titration of drugs. Hypertension in Women Oral contraceptives may increase BP, and BP should be checked regularly. In contrast, HRT does not raise BP. Development of HTN—consider other forms of contraception. Pregnant women with HTN should be followed carefully. Methyldopa, BBs, and vasodilators, preferred for the safety of the fetus. ACEI and ARBs contraindicated in pregnancy. Hypertension in Pregnancy May be due to pre existing essential HTN or pre-eclampsia. Methyl dopa is safe B Blockers are effective & safe in 3rd trimester Modified release prep of Nifedepine IV Labetalol for hypertensive crises ACE and ARBs best avoided Accelerated Hypertension (Diasstolic >140 mm Hg) Requires hospitalization. IV not necessary Rapid reduction not recommended can reduce organ perfusion; cerebral or myocardial ischemia Long acting CCB(Amlodipine or modified release Nifedipine) or B Blocker to start with to reduce BP 100-110 mm Hg. Then ACE/ARB may be added Na Nitroprusside by infusion is the drug of choice if IV necessary Pheochromocytoma Long term remedy is surgery. Alpha Blockers(Phenoxybenzamine) for short term management of episodes Tachycardia can be controlled with careful use of BBs Phentolamine for short term during surgery Causes of Resistant Hypertension Improper BP measurement Excess sodium intake Inadequate diuretic therapy Medication • Inadequate doses • Drug actions and interactions (e.g., nonsteroidal anti-inflammatory drugs (NSAIDs), illicit drugs, sympathomimetics, oral contraceptives) • Over-the-counter (OTC) drugs and herbal supplements Excess alcohol intake Identifiable causes of HTN ESH/ESC & ADA Guidelines ADA Treatment Recommendations for Diabetic Patients with Hypertension Recommended target blood pressure • Systolic <130 mm Hg • Diastolic <80 mm Hg Drug therapy mandatory above 140 mm Hg systolic and 90 mm Hg diastolic Recommended first-line agents for patients with microalbuminuria or clinical albuminuria • ARBs and ACE-Is ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker. American Diabetes Association. Diabetes Care. 2002;25(Suppl 1):S71-S73. ADA Treatment Recommendations for Diabetic Nephropathy Both ACE-Is and ARBs are first-line agents for treatment of albuminuria/nephropathy Initial choice in diabetic nephropathy for hypertensive and nonhypertensive patients with type 1 diabetes • ACE-Is Initial choice in diabetic nephropathy for hypertensive patients with microalbuminuria or clinical albuminuria and type 2 diabetes • ARBs If one class is not tolerated, the other should be substituted American Diabetes Association. Diabetes Care. 2002;25(Suppl 1):S85-S89. ACE-I = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker. ACE Inhibition Beyond Hypertensive Control Endothelium-Focus of New Research Arteriole lumen Endothelium Largest organ of the human body Causes and consequences of Endothelial Dysfunction Heart failure Vasospasm (coronory, cerebral) Diabetes Reocclusion Hypertension Endothelial dysfunction Hyperhomocystenemia Reperfusion injury Peripheral artery disease Hyperlipidemia Immune reaction Inflammatory disease Atherosclerosis Adopted from Rubanyi GM. J Cardiovasc Pharmacol. 1993;22(suppl 4):S1-S4 Additional Considerations in Antihypertensive Drug Choices Potential favorable effects Thiazide-type diuretics useful in slowing demineralization in osteoporosis. BBs useful in the treatment of atrial tachyarrhythmias/fibrillation, migraine, thyrotoxicosis (short-term), essential tremor, or perioperative HTN. CCBs useful in Raynaud’s syndrome and certain arrhythmias. Alpha-blockers useful in prostatism. Spironlactone in Conn,s syndrome Additional Considerations in Antihypertensive Drug Choices Potential unfavorable effects Thiazide diuretics should be used cautiously in gout or a history of significant hyponatremia. BBs should be generally avoided in patients with asthma, reactive airways disease, or second- or third-degree heart block. ACEIs and ARBs are contraindicated in pregnant women or those likely to become pregnant. ACEIs should not be used in individuals with a history of angioedema. Aldosterone antagonists and potassium-sparing diuretics can cause hyperkalemia. Conclusion According to baseline BP and presence or absence of complications, therapy can be initiated either with a low dose of a single agent or with a low-dose combination of 2 agents Most patients with hypertension will require 2 or more antihypertensive drugs to achieve BP goals Choice of therapy has to be individualized keeping in view the associated co morbid conditions Chobanian AV et al. JAMA. 2003;289:2560-2572. Guidelines Committee. J Hypertens. 2003;21:1011-1053. Thank You Trends in Awareness, Treatment, and Control of Hypertension in the US* 100 1976-1980 90 1988-1991 80 73% 70 Percentage of Population 60 1991-1994 68% 70% 55% 54% 51% 1999-2000 59% 50 40 29% 27% 34% 31% 30 20 10% 10 0 Aware Treated Controlled† *Data for 1999-2000 were computed (M. Wolz, unpublished data, 2003) from the National Heart, Lung, Blood Institute and data for National Health and Nutrition Examination Surveys II and III (phases 1 and 2) are from The Sixth Report of the Joint National Committee on Prevention Detection, Evaluation and Treatment of High Blood Pressure. High blood pressure is systolic blood pressure of 140 mm Hg or diastolic blood pressure 90 mm Hg, or taking antihypertensive medication. †Systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg. Chobanian AV et al. JAMA. 2003;289:2560-2572. Effect of Systolic and Diastolic Blood Pressure on Coronary Heart Disease Mortality: MRFIT 48.3 37.4 31.0 43.8 25.5 23.8 20.6 38.1 16.9 25.3 13.9 10.3 25.2 12.6 8.8 90-99 24.9 12.8 11.8 100+ 80.6 11.8 8.5 80-89 9.2 75-79 160+ 140-159 120-139 70-74 <70 Adapted from Neaton JD, Wentworth D. Arch Intern Med. 1992;152:56-64. <120 CVD Risk Factors Hypertension* Cigarette smoking Obesity* (BMI >30 kg/m2) Physical inactivity Dyslipidemia* Diabetes mellitus* Microalbuminuria or estimated GFR <60 ml/min Age (older than 55 for men, 65 for women) Family history of premature CVD (men under age 55 or women under age 65) *Components of the metabolic syndrome. CVD Risk HTN prevalence ~ 50 million people in the United States. The BP relationship to risk of CVD is continuous, consistent, and independent of other risk factors. Each increment of 20/10 mmHg doubles the risk of CVD across the entire BP range starting from 115/75 mmHg. Prehypertension signals the need for increased education to reduce BP in order to prevent hypertension. ESH/ESC 2003: Cardiovascular Risk Stratification Blood Pressure (mm Hg) Other Risk Factors and Disease History No other risk factors 1-2 risk factors ≥3 risk factors, target organ damage, or diabetes Associated clinical conditions Normal SBP 120-129 or DBP 80-84 High-Normal SBP 130-139 or DBP 85-89 Grade 1 SBP 140-159 or DBP 90-99 Grade 2 SBP 160-179 or DBP 100-109 Grade 3 SBP ≥180 or DBP ≥110 Average risk Average risk Low added risk Moderate added risk High added risk Low added risk Low added risk Moderate added risk Moderate added risk Very high added risk Moderate added risk High added risk High added risk High added risk Very high added risk High added risk Very high added risk Very high added risk Very high added risk Very high added risk Guidelines Committee. J Hypertens. 2003;21:1011-1053. JNC Classification of Blood Pressure for adults age 18 and older Category Systolic (mmHg) Diastolic (mmHg) Optimal Normal High-normal <120 <130 130-139 and or and 85-89 140-159 160-179 >180 or or or 90-99 100-109 110 Hypertension Stage 1 Stage 2 Stage 3 <80 <85 Relative risk of death In hypertension With Controlled BP Mortality Risk is Still Higher Than in Normotensive 2 Male Female 1.5 1 1 1 1.36 1.3 0.5 Normotensives Hypertensives, treated and controlled 1.82 1.97 Hypertensives treated and not controlled 0 High risk of mortality in patients with controlled BP points out to other causes of target Organ damage (e.g endothelial dysfunction) Hawlk RJ et al, Hypertension. 1989;13(suppl):1-20-1-32. Algorithm for Treatment of Hypertension Lifestyle Modifications Not at Goal Blood Pressure (<140/90 mmHg) (<130/80 mmHg for those with diabetes or chronic kidney disease) Initial Drug Choices Without Compelling Indications With Compelling Indications Stage 1 Hypertension Stage 2 Hypertension (SBP 140–159 or DBP 90–99 mmHg) Thiazide-type diuretics for most. May consider ACEI, ARB, BB, CCB, or combination. (SBP >160 or DBP >100 mmHg) 2-drug combination for most (usually thiazide-type diuretic and ACEI, or ARB, or BB, or CCB) Not at Goal Blood Pressure Optimize dosages or add additional drugs until goal blood pressure is achieved. Consider consultation with hypertension specialist. Drug(s) for the compelling indications Other antihypertensive drugs (diuretics, ACEI, ARB, BB, CCB) as needed. ACE InhibitorsBenefits Beyond Anti Hypertensive Effects “ Data collected from various studies suggested that treatment of hypertension with ACE Inhibitors could prevent endothelial dysfunction independent of systemic anti hypertensive effect.” Medical clinics of North America 1998 Circulating vs tissue ACE Circulating ACE (endocrine) •Plasma Tissue ACE (autocrine/paracrine) •Vasculature (endothelium) •CNS •Adrenal •Heart •Kidney •Reproductive organs •Lung Circulating ACE 10% Tissue ACE 90% Tissue ACE Mainly Responsible For Target Organ Damage Dzau VJ.Arch Intern Med. 1993;153:937-942 ACE Inhibition Vasculoprotective Effect Kininogens Angiotensinogen Kallikreinin Renin Angiotensin I Bradykinins ACE Inhibition Angiotensin II Inactive Peptides ACE Inhibition in vascular endothelium Ang II; Bradykinin; NO Laboratory Tests Routine Tests • Electrocardiogram • Urinalysis • Blood glucose, and hematocrit • Serum potassium, creatinine, or the corresponding estimated GFR, and calcium • Lipid profile, after 9- to 12-hour fast, that includes high-density and low-density lipoprotein cholesterol, and triglycerides Optional tests • Measurement of urinary albumin excretion or albumin/creatinine ratio More extensive testing for identifiable causes is not generally indicated unless BP control is not achieved (JNC 7) Importance of Endothelium in Vascular Damage In patients with hypertension permeability of endothelium is altered Endothelium - Source of a host of Vasoactive Substances & growth regulating peptides • Angiotensin II • Bradykinin Healthy Endothelium • Endothelin • Nitric Oxide • Insulin Growth Factor • Platelet Derived Growth Factor Many of these factor have been incriminated in the pathogenesis of Vascular Damage Damaged Endothelium Medical Clinics of North America Vol 18, # 5, 1997 -1117 Endothelial Function / Vascular Health Healthy endothelium maintains a balance between opposing states : • Dilation vs constriction • Growth inhibition vs growth promotion • Antithrombosis vs prothrombosis • (antifibrinolysis vs profibrinolysis) • Anti-inflammation vs pro-inflammation • Antioxidation vs pro-oxidation Lusher TF, Barton M. Clin Cardiol. 1997;10 (supplII):11-3-11-10.Vane JR et al.N Eng J Med. 1990;323:27-36. Harrison DG. Clin Cardiol. 1997;10(suppl):II-11-II-17
























































![[ Insert Title Here ]](http://s1.studyres.com/store/data/008479268_1-03ff748536c27aeae665c17a72e89ec4-150x150.png)