* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 18: The Endocrine System
Hormonal contraception wikipedia , lookup
History of catecholamine research wikipedia , lookup
Cryptorchidism wikipedia , lookup
Mammary gland wikipedia , lookup
Triclocarban wikipedia , lookup
Xenoestrogen wikipedia , lookup
Menstrual cycle wikipedia , lookup
Breast development wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Hyperandrogenism wikipedia , lookup
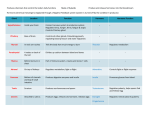
Crowther’s Tenth Martini, Chapter 18 Summer 2015 Chapter 18: The Endocrine System Chapters 12 through 17 were all about the nervous system. In Chapter 18, we leave the nervous system behind (sort of). The endocrine system is an alternative system for communicating messages through the body. Although it interfaces with the nervous system, its cells and messages are fairly distinct from those of the nervous system. 18.0: Outline 18.1: Types of intercellular communication There are 4 basic types of intercellular communication: direct, synaptic, paracrine, and endocrine. 18.2: Types of hormones and responses In terms of chemical structure, hormones are amino acid derivatives, peptides, or lipid derivatives. Hormone receptors can be on the cell surface and can cause changes in intracellular second messengers like cAMP and Ca2+, or they can be intracellular and and change gene expression. 18.3: The hypothalamic-pituitary axis: multi-level negative feedback! The hypothalamus secretes releasing hormones that control the release of other hormones from the anterior pituitary gland. These other hormones then stimulate other endocrine tissues to release still other hormones, which limit production of the upstream hormones via negative feedback. 18.4: Overview of the body’s major hormones The anterior pituitary gland secretes adrenocorticotropic hormone (ACTH), follicle stimulating hormone (FSH), growth hormone (GH), luteinizing hormone (LH), prolactin (PRL), and thyroidstimulating hormone (TSH). The posterior pituitary gland secretes antidiuretic hormone (ADH; also called vasopressin) and oxytocin (OXT). The thyroid glands secrete calcitonin and thyroid hormones (T 3 and T4). The parathyroid glands secrete parathyroid hormone (PTH). The cortex of the adrenal gland secretes aldosterone and glucocorticoids (cortisol, corticosterone). The medulla of the adrenal gland secretes epinephrine (also called adrenaline). The pancreas secretes insulin and glucagon. The kidneys secrete erythropoietin and calcitriol. The ovaries produce estrogens and progesterone. The testes produce androgens like testosterone. 18.5: Hormone synergy during growth, stress, and reproduction Growth during childhood depends critically on hormones like growth hormone (GH), insulin, and calcitonin. Stressful situations require adjustments in hormones like epinephrine and glucocorticoids. Reproduction is dependent on hormones like follicle stimulating hormone (FSH), testosterone, luteinizing hormone (LH), oxytocin (OXT), and prolactin (PRL). 18.6: Recommended review questions 1 Crowther’s Tenth Martini, Chapter 18 Summer 2015 18.1: Types of intercellular communication In any multicellular animal, the cells must be able to communicate with each other. At a cellular level, “communication” refers to the passing of a chemical from one cell to another. There are four general ways in which this may occur, as summarized by 10th Martini Table 18-1 (Mechanisms of Intercellular Communication). They are: Direct communication (discussed in Chapter 4, mentioned again in Chapter 12, and to be mentioned again in Chapter 20): chemicals pass directly from one cell to the next via gap junctions (protein channels that span the membranes of both cells). Synaptic communication (discussed in Chapter 12): neurotransmitters travel across synapses. Paracrine communication: this is similar to synaptic communication – chemicals released by one cell affect other nearby cells – but involves non-neuronal cells. Examples of paracrine signals include the cytokines used by the immune system (Chapter 22). Endocrine communication: the focus of this chapter. Similar to paracrine communication, but occurs over longer distances. Note that all of these mechanisms of communication depend on (intracellular or extracellular) protein receptors to receive the chemical messages that are released. Both the nervous system and the endocrine system maintain the body’s homeostasis, using negative feedback to keep regulated variables within certain limits. An important difference between the two is the time scale over which they operate. The nervous system is faster; messages may pass from the brain to the toes via the nervous system in a fraction of a second. In contrast, adjustments to endocrine system generally occur over seconds to days. 18.2: Types of hormones and responses Hormones are defined by 10th Martini as the chemical messengers of endocrine communication; they “are released in one tissue and transported in the bloodstream to alter the activities of specific cells in other tissues.” Hormones can thus be distinguished from paracrine messengers, which do not generally travel in the blood. According to their chemical structures, hormones are grouped into three categories: amino acid derivatives, peptide hormones, and lipid derivatives. These categories are depicted in 10th Martini Figure 18-2 (Structural Classification of Hormones). Amino acid derivatives are created from two amino acids in particular: tyrosine, which gives rise to thyroid hormones and epinephrine, and tryptophan, from which melatonin is created. Peptide hormones are all bigger than the amino acid derivatives because they consist of multiple amino acids linked together. They range in length from 9 amino acids (antidiuretic hormone and oxytocin) to >200 amino acids (thyroid-stimulating hormone, luteinizing hormone, and follicle-stimulating hormone). Lipid derivatives are made from lipids, as their name indicates. There are two distinct sub-categories: eicosanoids and steroids. Eicosanoids are most important as paracrine messengers, but some have endocrine functions as well. Steroids are molecules that are 2 Crowther’s Tenth Martini, Chapter 18 Summer 2015 chemically similar to cholesterol, with its characteristic 4-ring structure, and include the female and male sex hormones (estrogens, progesterone, and androgens like testosterone). The chemical structures of these hormones influence the location of their protein receptors. Since amino acid derivatives are hydrophilic, and peptide hormones are large (and hydrophilic), they can’t pass through cell membranes, so their receptors reside on the surface of the cell. Conversely, lipid derivatives CAN pass through cell membranes, so their receptors are found inside the cell. These different locations of hormones’ receptors correspond to different types of responses to each hormone. Actions triggered by the cell-surface receptors are illustrated in 10th Martini Figure 18-3 (G Proteins and Second Messengers). In short, binding of an amino acid-derived or peptide hormone causes the receptor to change shape such that a G protein connected to it is affected as well. G proteins have many effects, but most of them result in changes in intracellular levels of cyclic AMP (cAMP) or calcium (Ca2+). cAMP and Ca2+ are known as “second messengers” because they carry the messages of the hormones (the first messengers) into the interior of the cell. Actions triggered by intracellular hormone receptors, in contrast, are shown in 10th Martini Figure 18-4 (Effects of Intracellular Hormone Binding). Here the hormone-receptor complex travels to the DNA and alters transcription of specific genes, ultimately changing the expression of the corresponding proteins. 18.3: The hypothalamic-pituitary axis: multi-level negative feedback! Hormones are produced by many different tissues of the body, as shown in 10th Martini Figure 18-1 (Organs and Tissues of the Endocrine System). Many of the most important hormones are part of what is often called the hypothalamic-pituitary axis (CTM Figure 18.1). This name reflects the fact that hypothalamic secretions control anterior pituitary secretions, which in turn govern other secretions. The final hormone of the pathway – “Hormone 2” in the figure – generally inhibits secretion of the Releasing Hormone and Hormone 1, which then lowers secretion of Hormone 2. In this way, hormones often limit their own secretion. An example is inhibin, a hormone produced by the testes and ovaries in response to Follicle Stimulating Hormone (FSH). Inhibin inhibits release of Gonadotropin Releasing Hormone (GnRH) and FSH. Thus, high inhibin levels lead to a lowering of inhibin levels, and vice versa. 3 Crowther’s Tenth Martini, Chapter 18 Summer 2015 CTM Figure 18.1: The hypothalamic-pituitary axis. This is a rearrangement of some parts of 10th Martini Figure 18-8 (Feedback Control of Endocrine Secretion). Left: The general pattern of hormonal control. The hypothalamus sends a Releasing Hormone (RH) to the anterior pituitary, which then secretes a hormone (Hormone 1) that prompts an endocrine gland to secrete another hormone (Hormone 2). Hormone 2 then negatively feeds back on the hypothalamus and anterior pituitary so that secretion of the Releasing Hormone and Hormone 1 is reduced. Right: Specific examples, colored and spaced according to the general pattern on the left. For example, Thyrotropin Releasing Hormone (TRH) made by the hypothalamus stimulates the anterior pituitary to secrete Thyroid Stimulating Hormone (TSH; Hormone 1), which then prompts the thyroid gland (endocrine organ) to secrete thyroid hormones (Hormone 2). 18.4: Overview of the body’s major hormones In its usual fashion, 10th Martini provides very detailed information about the 30 or so hormones produced by the human body. We will highlight a few points here, working our way through SOME of the producers of these hormones. Hypothalamus As noted above, the hypothalamus produces several releasing hormones that stimulate the anterior pituitary gland to release hormones. Examples are shown in CTM Figure 18.1. 4 Crowther’s Tenth Martini, Chapter 18 Summer 2015 Pituitary Gland The pituitary, a pea-sized gland located directly under the hypothalamus, is often called the “master gland” because its hormones control so many other parts of the endocrine system. It has two distinct lobes, the anterior pituitary (adenohypophysis) and posterior pituitary (neurohypophysis). They are fairly distinct from each other histologically; the anterior pituitary is full of endocrine cells, while the posterior pituitary contains the axons of hypothalamic neurons (hence the name “neurohypophysis”). o The anterior pituitary releases hormones such as the following: Adrenocorticotropic hormone (ACTH): stimulates production of corticosteroids from the cortex of the adrenal gland. Follicle Stimulating Hormone (FSH): stimulates secretion of estrogens from ovaries; stimulates development of ovarian follicles. Growth hormone (GH): controls growth of the body. Luteinizing Hormone (LH): stimulates secretion of progesterone from the ovaries and testosterone from the testes; stimulates ovulation and formation of the corpus luteum. Prolactin (PRL): controls milk production in nursing mothers. Thyroid-stimulating hormone (TSH): stimulates production of thyroid hormone by the thyroid gland. o The axon termini of the posterior pituitary release two major hormones: Antidiuretic hormone (ADH; also called vasopressin): causes reabsorption of water so that it is not lost in the urine. Oxytocin (OXT): stimulates contractions of the uterus; also involved in sexual arousal. Thyroid Glands (2) In response to TSH from the anterior pituitary gland, the thyroid glands secrete two iodine-containing hormones (see 10th Martini Figure 18-1 to confirm the presence of iodine, whose chemical abbreviation is I). They are named for the number of iodine atoms they contain; triiodothyronine (or T3) contains three, while tetraiodothyronine (or T4) contains four. As you may be aware, table salt is “iodized,” meaning that a small portion of it is NaI rather than NaCl, thus ensuring that your diet includes adequate iodine. Collectively, T3 and T4 are often referred to simply as “thyroid hormones.” Their overall function is to speed up cellular metabolism. As we saw in Chapter 6, the thyroid glands also produce calcitonin, which promotes bone-building activity by osteoblasts. Parathyroid Glands (4) As we saw in Chapter 6, the parathyroid glands secrete parathyroid hormone (PTH) in response to low levels of calcium in the blood. PTH leads to bone resorption by osteoclasts, releasing more calcium back into the blood. It also increases the kidney’s retention of calcium and the kidney’s production of calcitriol, thus increasing calcium absorption by the digestive tract. 5 Crowther’s Tenth Martini, Chapter 18 Summer 2015 The combined actions of calcitonin and PTH were shown in 10th Martini Figure 6-15 (Factors That Alter the Concentration of Calcium Ions in Blood) and are also shown in 10th Martini Figure 18-13 (The Homeostatic Regulation of Calcium Ion Concentrations). Adrenal glands (2) If you can remember that renal refers to the kidneys, then you should be able to remember that the adrenal glands are just above the kidneys (ad = “near”). Like other tissues such as bones and the brain, the adrenal gland has an outer region called the cortex and an interior region called the medulla. o The adrenal cortex produces aldosterone, which increases Na+ retention in the kidney, and glucocorticoids such as cortisol and corticosterone, which alter the release and usage of lipids, amino acids, and glucose by the liver, adipose tissue, and skeletal muscles. o The adrenal medulla produces epinephrine (also called adrenaline – a name which reminds us of its source) and the related compound norepinephrine (noradrenaline), which increase heart rate and blood pressure. Pancreas As we will see in Chapter 24, most cells of the pancreas promote digestion via secretion of enzymes and bicarbonate. However, the pancreas also includes small patches of cells, called islets, which secrete hormones such as insulin and glucagon. Insulin promotes removal of excess glucose from the blood, while glucagon promotes addition of glucose to the blood. Diabetes mellitus is a condition where either inadequate insulin is produced (type I diabetes mellitus) or cells do not respond efficiently to insulin (type II diabetes mellitus). Kidneys (2) Like the pancreas, the kidneys are not primarily endocrine organs. Their major functions of waste removal and water balance are covered in Chapters 26 and 27. However, the kidneys also secrete two important hormones: erythropoietin (epo for short), which stimulates red blood cell production in red bone marrow, and calcitriol, which stimulates absorption of calcium and phosphate by the digestive tract. Recall that calcitriol is produced via a complicated pathway also involving the skin and liver, as diagrammed in 10th Martini Figure 5-6 (Sources of Vitamin D3). Gonads (2) The male gonads, the testes, secrete androgens (such as testosterone – the name indicates that it is produced by the testes), which promote sperm development, protein synthesis in skeletal muscles, and the development of male sexual characteristics such as facial hair. The female gonads, the ovaries, secrete estrogens – which promote maturation of ovarian follicles and the development of female sexual characteristics such as breast enlargement – and progesterone – which prepares the uterus for implantation of a fertilized egg. 6 Crowther’s Tenth Martini, Chapter 18 Summer 2015 18.5: Hormone synergy during growth, stress, and reproduction In reading the above descriptions of what the various hormones do, you might imagine that several of them cooperate to meet complex physiological demands … and indeed they do! Here are a few examples of scenarios requiring the action of multiple hormones. Growth. Growing children require, among other things, growth hormone (GH) to promote development of tissues such as muscle and bone, insulin to promote uptake of glucose (which provides energy needed for growth), and calcitonin to promote calcium absorption for building bones. Stress. In a “fight or flight” situation, epinephrine from the adrenal gland helps raise heart rate and blood pressure; it also promotes release of glucose and fatty acids into the blood so that exercising muscles are well-fueled. For longer-term stress lasting hours or days, glucocorticoids from the adrenal cortex adjust the body’s metabolism to conserve and replace valuable glucose reserves, promoting synthesis of new glucose by the liver and promoting the use of lipids and proteins as energy sources, rather than glucose. Reproduction. We will explore reproduction more fully in Chapter 28. For now, we can simply note the critical roles of several hormones listed above. Eggs (oocytes) are surrounded by supporting follicle cells, and the whole thing (egg + follicle cells) is known as a follicle. Follicle development is guided by follicle stimulating hormone (FSH). Meanwhile, sperm maturation in the testes is guided by testosterone produced by the testes. Luteinizing hormone (LH) triggers release of an egg from the ovary into its fallopian tube – an event called ovulation. The now-ruptured follicle, now called the corpus luteum, secretes progesterone, which builds up the lining of the uterus in anticipation of possible implantation of the egg. During labor and delivery, oxytocin (OXT) stimulates contractions of the uterus. Milk production by the mammary glands of new mothers is promoted by prolactin (PRL). 18.6: Recommended review questions If your understanding of this chapter is good, you should be able to answer the following 10th Martini questions at the end of Chapter 18: #1, 2, 3, 4, 5, 6, 13, 15, 18, 23, 24, 25, 27, and 28. (Note that these are NOT the Checkpoint questions sprinkled throughout the chapter.) Explanation This document is my distillation of a chapter of the textbook Fundamentals of Anatomy & Physiology, Tenth Edition, by Frederic H. Martini et al. (a.k.a. “the 10th Martini”). While this textbook is a valuable resource, I believe that it is too dense to be read successfully by many 7 Crowther’s Tenth Martini, Chapter 18 Summer 2015 undergraduate students. I offer “Crowther’s Tenth Martini” so that students who have purchased the textbook may benefit more fully from it. No copyright infringement is intended. -- Greg Crowther 8