* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Acute chest pain
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Cardiovascular disease wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Cardiac surgery wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
Transcript
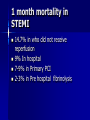
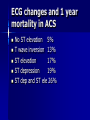
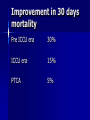
Acute Coronary (Confusional) Syndrome Dr.A.M.Thirugnanam MD.,MSICP.,Ph.D.,FSCAI.(USA) Interventional Cardiologist IPCARD Heart Institute Global Hospitals- Hyderabad. Date: 09-02-2008 ACS- the confusion kills the Patients 1. One in six patients with ACS treated as atypical chest pain. 2. one in three acute MI goes into complications. 3. 25% of the acute MI did not get proper reperfusion. 4. At least one half die within 1 hr of symptoms onset or before reaching the hospital. 5. 24% men and 42% women die within one year. 6. 66% fail to achieve full recovery. 7. 21% men and 30 women develops CHF within 6 years. ACS the confusion kills the patients-Global registry of acute coronary events Median time from symptoms onset to presentation was 2-3 hrs for age <45, and 3 hrs for >85 years age. Atypical presentation, a worse prognosis with 3 fold higher risk of mortality due to delay in diagnosis and treatment. Atypical presentation of ACS-Worcestor Heart Attack Study report 63% experience chest pain. Above 75 years women only 50% 22% experience only dyspnea 32% experience dizziness, arm numbness, head ache, syncope, sweating, palpitation, weakness and confusion, due to diminished autonomic response, age related diastolic dysfunction, lung diseases, and associated pulmonary diseases. Acute chest pain-Vascular Aortic dissection-Excruciating, ripping pain on sudden onset in anterior chest. Causes: HTN, connective tissue disorders ECG- no significant Cardiac Enzyme: no elevation except CRP. Acute chest pain-Vascular Pulmonary Embolism: Sudden onset of dyspnea and pain, pleuritic with pulmonary infarction. Causes: DVT,CTD,CAD,etc ECG: RBBB, ST,ST-T changes, Q in III and S1 Enzyme: no elevation Acute chest pain-Vascular Pulmonary HTN: Substernal chest pressure and exacerbated by excertion Pain associated with dyspnea and evidence of PHT ECG-no significant ST elevation or depression Enzyme: d-dimer in case of PTE Acute chest painPulmonary cause Pleuritis/Pneumonia: brief over involved area, lateral to mid line pain with dyspnea. Tracheobronchitis / Spontaneous Pneumothorax: burning in midline associated with cough and pain ECG: no significant Enzyme: no Acute chest painGastrointestinal cause Esophageal reflux: burning epigastric,1060min, aggravated by large meal, relieved by antacid. Peptic ulcer: Prolonged epigastric or Substernal burning, relieved by antacid of food. Gallbladder disease: prolonged epigastric, right upper quadrant pain, unprovoked Pancreatitis: Prolonged, intense epigastric and Substernal pain, RF include alcohol, medications and hypertryglyceridemia. Acute chest painMusculoskeletal Cause Costochondritis: Sudden onset of intense fleeting type pain, by affected joints, occasional swelling and inflammation. Cervical disc Diseases: Sudden onset of Fleeing pain, may be reproduced with movement of neck. Acute chest pain- other causes Infections: herpes zoster, prolonged burning pain in dermatomal distribution. Vesicular rash. Psychological: Panic pain, chest tightness or aching often accompanied by dyspnea and lasting 30 min, may have with emotional disorders. What is mean ACS? Chest pain: Precipitation by stress, emotion, cold, 2-20 min, MI->30 min. ECG Classification: ST-T changes, Q waves, LBBB, and RBBB with ST elevation ECG: 75% STEMI develops into QWMI. 25% persists STEMI with absence of R wave. Pathology- cell death Imaging studies: loss of perfusion and RWMA Biomarkers: C-Troponin-necrosis, CRP-inflammation, BNP- LV overload. Atypical Presentation of ACS Patient older than 75 years, ECG in evolution, non specific ST-T changes. Diabetic patients. Previous MI Stuttering chest pain IL1,TNF,IL6,I L18,MCP1 MMPS,IL18 ICAM,VCAM, ,MPO.MRP, S selectin CD40L,tPA,PAI1,Ddimer,VWF, MPO,MRP Evolution of ECG in Acute Diagnostic markers ACS Non–ST-segment elevation ACSe Stable angina ST-segment elevation AMI Unstable angina Non–Q-wave AMI Q-wave AMI CK-MB Troponin T or I C-Reactive Protein Antman EM. In: Braunwald E, ed. Heart Disease: A Textbook in Cardiovascular Medicine, 5th ed. Philadelphia, Pa: WB Saunders; 1997. ECG-Enzyme changes in ACS Stable angina Creatine kinase evidence of necrosis ECG early ECG late Unstable Non–Q-wave Q-wave angina AMI AMI None Positive Positive ST-segment ST-segment ST-segment depression depression elevation and/or and/or T-wave inversionT-wave inversion No Q No Q Q develops Antman EM. In: Braunwald E, ed. Heart Disease: A Textbook in Cardiovascular Medicine, 5th ed. Philadelphia, Pa: WB Saunders; 1997. Biomarkers and mortality CRP and cardiac Troponin -T and I have direct proportion to mortality. CD40L had 5 times higher mortality in ACS. Management of ACSSTEMI Dose STK 1.5m Altep100mg Retep20mg TNK-tPA50mg TIMI-3 32% 54% 60% 63% 90min patency 50% 75% 75% 75% 1 month mortality in STEMI 14.7% in who did not receive reperfusion 9% In hospital 7-9% in Primary PCI 2-3% in Pre hospital fibrinolysis ECG changes and 1 year mortality in ACS No ST elevation 5% T wave inversion 13% ST elevation 17% ST depression 19% ST dep and ST ele 26% Improvement in 30 days mortality Pre ICCU era 30% ICCU era 15% PTCA 5% Identifying Patients for Reperfusion ECG indications: ST elevation, LBBB, RBBB with ST elevation Biomarker Indication: elevated CK-MB, cTnT and I, CD40L, The best way to treat ACS Thrombolysis with in 30 min. If possible shift the patient immediately to PCI within 90 min. Measure all biomarkers to assess the prognosis and outcome, include BNP, CRP, Troponin I or T, CD40L, MPO Ensure the administration of all important drugs. Medical management Anti Platelets: Aspirin, Clopidogrel Anticoagulants: UFH, LMWH, DTI Fibrinolytics: STK, UK, ALTE,RETE, TNK. Statins, ACEIS, BBS, Flavinoids, Adenosine, and antioxidants. Glycoprotein Receptor Blockers: Abciximab, Eptifibatide, Tirofiben. Invasive management Primary PTCA and Stenting. Administration of GP2b3aRBs, which reduces CRP-32%, IL6-76%, TNF alpha-100%. Intra coronary infusion of adenosine for no flow or sluggish flow after PTCA. Primary PTCA in AMI 55 yrs male H/O smoker, No DM, no HTN, No lipid abnormalities. ECG- ST elevation in V2-V6 Elevated CK-MB, Troponin Positive, CRP positive Echo- severe LV dysfunction CAG- mid LAD total occlusion. Normal coronary arteries Left coronary artery Right coronary artery Acute AWMI- LAD mid 100% occlusion Echocardiogram of AWMI-LAD region After Primary Stenting to LAD mid Time dependence in occlusion Cross-sections of left ventricle after experimental coronary artery occlusion xx x xx xx x x x x xxx x x x xx x Duration of occlusion Necrosis 40 min XXX X Ischemic but viable Reimer KA, et al. Circulation. 1977;56:786-794. x x x x x xx x x x x 3h Nonischemic 24 h Area supplied by occluded artery ACS-RCA ostial tight lesion 58 male. Smoker, alcoholic, no DM, no HT, no CVA, no BA, No APD, no H/O previous surgical history. complaints: DOE Class-2, EA-class 2 ECG: ST depression in inferolateral leads, more than 3mm. Echo-Severe LV dysfunction. EF-30%. CAG: ostial RCA 99% tight lesion. RCA ostial tight lesion 99% Dilating the lesion with Balloon 3mm/12mm After stent deployment Asymptomatic Male 50 years male. Known DM, HTN, no smoker, no alcoholic, no CVA, no BA, no APD. No chest pain, only SOB Underwent routine cardiac check up. TMT positive. ECG: NSR, No ST-T changes Echo: normal LV fxn, no RWMA. CAG: LAD severe disease, RCA-distal 90%, LCX-mid 60% lesion. LAD in DM asymptomatic LAD 65 years old female. Cardiogenic shock Known HTN, DM, DNP, smoker. Admitted with cardiogenic shock. BP50/60mmhg, HR-120/min, O2-92% ra, ECG- Wide QRS in all leads, ST elevation in all leads Echo- global hypokinesia, EF-25% CAG- LM-100%, RCA-normal non dominant. Left main -100% occlusion Emergency management Dopamin, Dobutamin, noradrenalin, IV integrillin, Enclex, Clopivas-AP. IABP support Post PTCA and Stenting of LM Home taking Points Multi biomarkers approach will reduce the mortality. New Biomarkers: PDGF, PF-4, CD152, CD40L, PMN chemokines, Thrombospondin, TGF-B and Nitric oxide. Door to needle time less than 30 min, Door to Balloon time less than 90 min. Ensure all the essential drugs before discharge.