* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Acute Coronary Syndrome
Saturated fat and cardiovascular disease wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Jatene procedure wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Electrocardiography wikipedia , lookup
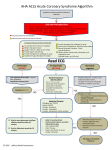
Spencer Toombes FRACP Challenges of assessing patients with chest pain... Terminology & Pathophysiology ECG interpretation Use of Troponin Risk Assessment Inpatient management - how and when to transfer Post-discharge management For each of the following scenarios... What is the most likely diagnosis? What is this patient’s risk of having an Acute Coronary Syndrome? Complaining of intermittent central chest pain. Previous ischaemic heart disease: Coronary angiogram 2 years ago showed 40% LAD and 30% RCA stenosis. Managed medically. Has noticed over the past 2 months that he needs to use his GTN spray whenever he exerts himself. What if he had received a stent 5 months ago? Recent sharp, stabbing pain adjacent to her left sternum. There doesn’t seem to be a clear precipitant. She feels a bit washed out, but otherwise reasonably well. …but she is a Type II diabetic. 10 minutes of central chest heaviness after he finished mowing the lawn Associated with pallor and breathlessness His wife thought he looked ill and talked him into coming up to your practice. Positive family history, heavy smoker. (Includes biliary) Cardiac Oesophageal 28% 14% 60% 37% 10% 100% 100% 49% 35% 23% 5% 18% 12% 33% Back 12% Back 33% Bennett et al. Lancet. 1966 Intensity of Pain - no indication of severity. Nature of Pain - no indication of diagnosis: • 5-19% acute coronary syndromes ‘sharp’ or pleuritic. Physical Signs - no indication of diagnosis: • 15% AMI patients have chest wall tenderness. ‘Atypical’ Presentations: • Up to 25% patients with ACS do not present with “classical” chest pain. Acute Coronary Syndrome (ACS) Stable angina Unstable angina Myocardial ischaemia Q wave infarction Non-Q wave infarction STEMI... STEACS Non-STEMI... Non-STEACS little cholesterol content thick fibrous cap low risk of rupture The proportion of the lumen occluded determines the degree of exercise related ischaemia, and the severity of symptoms. Lots of Low Density Lipoprotein Cholesterol Thin fibrous cap Lots of inflammation: Activated T cells, Macrophages, Foam Cells Mediators: Cytokines and C reactive protein HIGH RISK OF RUPTURE Dynamic Partial Occlusion: No damage Worsened Angina pain, possible ECG change No cardiac enzyme rise Dynamic Partial Occlusion: Some damage Worsened Angina pain, probable ECG change Rise in cardiac troponin, +/- creatinine kinase Complete Occlusion: Full thickness myocardial infarction ST segment elevation, Q wave formation if not treated Acute Coronary Syndrome : Terminology Low-risk UAP High-risk UAP “minor myocardial damage” Non-ST Elevation MI ST Elevation MI Troponin CK Serum markers No detectable troponin Normal CK Detectable troponin Normal CK ECG at evaluation Normal ECG ST depression or transient ST elevation ECG at discharge Normal ECG no Q wave Detectable troponin and elevated CK ST elevation Q or no Q wave Rapid assessment. Observed environment. Aspirin 300mg. ECG within 10 minutes of presentation. STEMI: requires immediate reperfusion Everything else: still requires risk assessment. Tnl TnC TnT Ca++ Tropomyosin Actin Exquisitely sensitive marker of myocardial distress... not necessarily muscle necrosis Onset 4-6, peak 24-36 hours, offset 7 days Normal initial troponin is NOT reassuring Normal 12 hour troponin is quite reassuring Lindahl NEJM 2000 343:16;1139-47 Don’t necessarily mean ACS... Pulmonary embolus Left ventricular failure Renal failure Sepsis True false positives related to assay Immune cross reactivity GENERALLY DO NOT ORDER IN GENERAL PRACTICE Presentation of ACS (clinical presentation, initial ECG) Working diagnosis NSTEACS STEMI Time Evolution of ECG and biomarkers Myonecrosis confirmed Final diagnosis STEMI NSTEMI Myonecrosis not confirmed Unstable angina ACS = acute coronary syndromes; ECG = electrocardiogram; STEMI = ST-segment-elevation myocardial infarction; NSTEACS = non-ST-segment elevation acute coronary syndromes; NSTEMI = non-ST-segment elevation myocardial infarction Acute Coronary Syndrome Guidelines Working Group. Med J Aust 2006;184(8 Suppl):S9-29. Complaining of intermittent central chest pain. Previous ischaemic heart disease: Coronary angiogram 2 years ago showed 40% LAD and 30% RCA stenosis. Managed medically. Has noticed over the past 2 months that he needs to use his GTN spray whenever he exerts himself. Recent sharp, stabbing pain adjacent to her left sternum. There doesn’t seem to be a clear precipitant. She feels a bit washed out, but otherwise reasonably well. …but she is a Type II diabetic. 10 minutes of central chest heaviness after he finished mowing the lawn Associated with pallor and breathlessness His wife thought he looked ill and talked him into coming up to your practice. Positive family history, heavy smoker. What is their risk of having an Acute Coronary Syndrome? These patients can be managed with upgrade to their anti-anginal medications and outpatient referral for cardiac investigation. These patients generally require emergency admission to a monitored environment, and aggressive drug therapy including parenteral anticoagulants. These patients generally require a period of observation with serial ECG and biomarker assessment, enabling them to be re-classified as high or low risk... Ambulance Monitoring Oxygen ? Nitrates ? Aspirin ? Pain relief ? Intermediate risk: reclassify after 6-12 hours Low risk: Upgrade therapy? Provocative investigation: EST or MPS High risk... Aspirin 300mg. stat. then 75 -100mg. daily. Clopidogrel: 300mg. load then 75mg. daily Gp IIbIIIa receptor antagonists: Tirofiban (Aggrastat) Abciximab (Reopro) Eptifibatide (Integrilin) CLOPIDOGREL C ADP ADP GPllb/llla Activation (Fibrinogen receptor) Collagen thrombin 2 TXA COX ASA TXA2 COX, cyclooxygenase; ADP, adenosine diphosphate; TxA2, thromboxane A2 Schafer AI Am J Med 1996;101:199–209 Pathways of Blood Coagulation during Hemostasis and Thrombosis Furie B and Furie B. N Engl J Med 2008;359:938-949 IV unfractionated heparin infusion s/c low molecular weight heparin (eg. Clexane 1mg./kg. bd.) s/c Fondaparinux (Erixtra) Beta blockers, IV and/or oral. Insulin + dextrose infusion for high BSL. High dose Statins: ACE inhibitors Oxygen Morphine & Nitrates for symptom control eg. 80mg. Atorvastatin Evidence supports prompt routine angiography with a view to angioplasty of the culprit lesion. ▪ TACTICS TIMI18, FRISC II, RITA 3 ▪ ICTUS ??? Short term death 7% vs. 9% STD excld. SHOCK 5% vs. 7% Reinfarct rates 3% vs. 7% CVA 1% vs. 2% Combined endpoint 8% vs. 14% Cardiologists drive SAABs: S tatin (high dose atorvastatin) A nti platelet agents: Aspirin + Clopidogrel A ce inhibitor B eta-blocker Sexual Relations: 6-7 METS: Stage II Bruce, 2 flights stairs Driving: (private license) Angioplasty: 2 days, assuming no MI, no symptoms and normal ecg. Myocardial Infarct: 2 weeks, assuming uncomplicated Cardiac Arrest: 6 months, unless assoc. MI Assessing chest pain is notoriously difficult Early aspirin, Early ECG If in doubt, manage as an inpatient Risk stratification, with serial data Aggressive drug combinations for high risk patients... Anticoagulants, and Antiplatelets.