* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Case Study Answer KEY
Survey
Document related concepts
Transcript
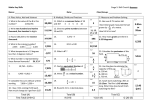
Anatomy and Physiology Fisher Case Study A Sarah, a forty-nine year old Anglo woman, visits her physician complaining of weight loss, sweating, listlessness and flu-like symptoms (fever, headache, scratchy throat, generalized body ache). After checking her history the physician notes that Sarah is married, has four children and no previous history of chronic illness. Her weight has decreased 15 pounds over the past three months and she presents with a temperature of 101o F, a slightly elevated pulse (85 beats per minute), normal blood pressure (112/78 mm Hg) and slightly labored breathing. Sarah has a negative family history of cardiovascular and respiratory disease. All of her family members are living and are free of cardiovascular or respiratory diseases. Sarah does not smoke and is current on all immunizations. She does report that she developed these symptoms a few days after visiting a friend whose son was home with a cold. After a chest X-ray and physical examination of Sarah’s ear, nose and throat, the physician confirms the diagnosis and prescribes bed rest, aspirin and a nasal decongestant. The physician also cautions Sarah from returning to her normal activities until she has been afebrile for a minimum of 24 hours. Sarah’s condition continues to worsen such that a week later she returns to her physician’s office. She has pain on the left side of her chest, is coughing more frequently and her sputum has a yellow color. Her respiratory rate is 32 breaths per minute and her breathing is labored. Her blood pressure is unchanged and does not demonstrate postural changes. Breath sounds indicate inspiratory rates and a chest Xray indicates a dense infiltrate within the lungs. Physical examination reveals lymphadenopathy. The physician suspects pneumonia and orders laboratory tests on Sarah’s blood and sputum. The results of the sputum tests indicate the presence of gram positive diplococci and polymorphonucleocytes that are too numerous to count. What concerns the physician, however, are the results of Sarah’s blood test. Her blood tests indicate leukopenia, anemia, and thrombocytopenia. In addition, the differential leukocyte count indicates that the concentration of helper T cells has decreased. The physician now suspects that Sarah has been infected with the human immunodeficiency virus (HIV) and that she has developed pneumonia as a result of the immune suppression. In reviewing her history, the physician notes that Sarah has been married for the past 30 years and does not admit to any extramarital affairs. She has not received any blood transfusions or blood products and does not use intravenous drugs. She is a selfemployed certified public accountant and has not visited any countries with high incidences of HIV infection. Upon further discussion, Sarah does mention to the physician that she and her husband were separated a few years ago for approximately 6 months as a result of his extramarital affair. The physician asks Sarah if he can run another test to determine whether or not she has contacted HIV and asks Sarah to talk to her husband about being tested for HIV as well. The physician also begins treating Sarah for the pneumonia that has developed and asks her to return the next day for the results of the HIV test. 1 modified 5/7/2017 Anatomy and Physiology Fisher The next day Sarah and her husband return to the physician’s office and the physician confirms that the enzyme-linked immunoadsorbent assay confirms that Sarah is HIV positive. The physician does mention that a second more sensitive test will be conducted to confirm this finding, however, he is doubtful that the result will indicate a false positive in the first test. Her husband admits to having numerous extramarital affairs with both women and men and consents to a blood test to determine his HIV status, which subsequently is positive. The physician then discusses the replicative cycle of HIV, the concept of a retrovirus, and treatment options with both Sarah and her husband. Sarah immediately starts on a regimen of protease inhibitors and nucleoside analogs (azidothymidine, AZT, and ddI). In addition, the physician discusses with Sarah and her husband the necessity of practicing "safe sex" even though both are HIV positive and the importance of not exposing themselves to opportunistic diseases. In addition, he mentions that some of the drugs they will be taking to minimize viral replication may cause nausea. He cautions them to take all medications as scheduled and to return to his office at the first sign of any disorder. He also reiterates that this disease can not be transferred by casual contact, but can be transferred through an exchange of body fluids (blood, semen and vaginal secretions). 1. Define each of the bold terms in the description. Term Definition Afebrile not feverish Anemia an abnormally low number of erythrocytes, concentration of hemoglobin, hematocrit, or any combination of these measures the inability of the immune system to mount a normal response to an antigen or antigens Immunodeficiency Leukopenia abnormally low numbers of leukocytes, usually less than 5000 per cubic mm Lymphadenopathy swollen lymph nodes, often indicating diseased lymph nodes Polymorphonucleocytes a white blood cell with a multilobed nucleus; a granulocyte Protease inhibitors enzymes that inhibit the actions of proteolytic enzymes (proteases) Retrovirus a virus that contains ribonucleic acid as its genetic material and utilizes reverse transcriptase to synthesize a complementary DNA molecule that becomes integrated into a chromosome of the host cell Thrombocytopenia abnormally low numbers of thrombocytes, usually less than 130,000 per cubic mm 2 modified 5/7/2017 Anatomy and Physiology Fisher 2. Why was HIV not initially considered as a possible cause for the symptoms Sarah presented with? Infection with HIV was not initially considered since Sarah did not present with any of the risk factors. She has been in a monogamous relationship for at least 30 years and has not received any blood transfusions or blood products. She does not use intravenous drugs and her travel has not taken her to areas where she would be at risk for HIV infection. 3. Why did Sarah’s symptoms worsen and develop into pneumonia? The initial symptoms worsened due to the inability of her immune system as a result of her positive HIV status, to mount an adequate response to the bacteria which were present in her respiratory tract. Since her immune system was unable to respond, the bacteria were able to become established in the airway. The polymorphonucleocytes increase in concentration in the sputum to respond to the bacteria. These cells, while part of the immune response, are not specifically affected by HIV and would continue to mount a response to a pathogenic organism. These cells were not sufficient to prevent the development of pneumonia. 4. Identify the specific types of leukocytes and the function of each cell. The different types of leukocytes and the functions attributed to each are shown in the following table. Leukocyte Function(s) Basophil Release of heparin and histamine Eosinophil Destruction of antibody-coated pathogens Neutrophil Phagocytosis of antibody-coated pathogens Monocyte Develop into macrophage Macrophage Phagocytosis of pathogens and activation of T cells B lymphocyte Antibody production and differentiation into memory cells T lymphocyte Destruction of virus-infected cells Natural killer cell Attack and lyse virus-infected cells or cancer cells 5. Why does HIV specifically affect one type of leukocyte? A single type of lymphocyte, the CD4+ T lymphocyte or helper T cell, is the only subpopulation of leukocyte infected by HIV. This occurs because the HIV binds specifically to a receptor on the surface of the helper T cells. The virus has a specific glycoprotein known as gp120 which binds to the CD4 molecules on the surface of the helper T cells. This 3 modified 5/7/2017 Anatomy and Physiology Fisher binding allows for the HIV to then fuse with the plasma membrane of the helper T cell and infect the cell. 6. Why can protease inhibitors and nucleoside analogs be used in minimizing the replication of the HIV virus? Protease inhibitors can be used because the genome of HIV encodes for a protease which is required for the formation of viral proteins from larger proteins produced by translation in the cell. Inhibiting this protease by the use of protease inhibitors would block the formation of viral proteins and subsequently viral production. The use of nucleoside analogs will block the production of viral RNA. These nucleoside analogs are added to the growing RNA strand and since they lack a free 2’ hydroxyl group, the synthesis of the RNA molecule ceases. If the cell is unable to synthesize the RNA for the assembly of the virus, then viral replication is minimized. Using these drugs in combination with each other has proven more effective than using each drug alone. 4 modified 5/7/2017