* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download the endocrine system - People Server at UNCW
Survey
Document related concepts
Transcript
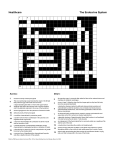
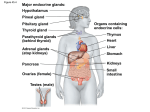
THE ENDOCRINE SYSTEM A. ENDOCRINE GLANDS Compare exocrine with endocrine glands. The body contains two types of glands: Exocrine glands secrete their products into ducts or directly onto epithelial surfaces. Endocrine glands secrete their products called hormones, into the extracellular fluid around the secretory cells. The secretion then diffuses into the blood for distribution throughout the body. Which organs are endocrine only? There are a number of specific organs whose sole function is endocrine: pituitary gland thyroid gland parathyroid glands (4) adrenal glands (2) pineal (epithalamus) thymus gland Name other organs that have some endocrine function. pancreas gonads (2) kidneys stomach small intestine liver heart placenta B. COMPARISON OF NERVOUS AND ENDOCRINE SYSTEMS Together, the nervous and endocrine systems coordinate the functions of all body systems. How does the nervous system achieve this? The nervous system achieves this through the use of nerve impulses and the secretion of neurotransmitter substances that either excite or inhibit the effector. 155 How does the endocrine system achieve this control? The endocrine system, in contrast, regulates body functions by releasing chemical messengers called hormones (“to urge on” or “to set in motion”) into the bloodstream for delivery throughout the body. Compare the types of effectors the two systems utilize to maintain homeostasis. The nervous system causes muscles to contract and glands to secrete. The endocrine system regulates metabolic activities, growth and development, and reproduction. Compare the time frame the two systems need to accomplish their actions. The nervous system tends to act in milliseconds. The endocrine system acts in seconds, minutes, hours, weeks, months, even years, depending upon the hormone. Compare how long the effects of the two systems persist. Nervous effects are brief; endocrine effects are much longer lasting. C. HORMONES 1. HORMONE RECEPTORS What is an endocrine target cell? Although a given hormone travels throughout the body in the blood and is “seen” by all cells of the body, it only affects specific cells called target cells. Like neurotransmitters, hormones influence their target cells by chemically combining to protein receptors on the target cell surface. Only target cells for a particular hormone bear receptors for that hormone, bind to it, and respond to it. Receptors, like other cellular proteins, are constantly synthesized and broken down as part of routine cellular maintenance. What is down-regulation of a target cell’s hormone receptors? Down-regulation occurs when the hormone is present in excess and the cell reduces the number of available receptors for it. This causes a decrease in cellular responsiveness to the hormone. 156 What is up-regulation of a target cell’s hormone receptors? Up-regulation occurs when the hormone is present in less than normal amounts and the cell increases the number of available receptors for it. This causes an increase in cellular responsiveness to the hormone. 2. CIRCULATING AND LOCAL HORMONES Define each of the following: Circulating hormones – Hormones that pass into the blood and act on distant target cells are called circulating hormones or endocrines. Local hormones – Hormones that act on target cells close to their site of release are called local hormones. They are further subdivided into either paracrine or autocrine. Paracrine hormones – Paracrines are local hormones that act on neighboring cells. Autocrine hormones – Autocrines are local hormones that act on the same cell that secreted them. D. MECHANISMS OF HORMONE ACTION Various target cells may respond differently to the same hormone (Ex: insulin in the liver causes glycogen formation, but in adipose cells it causes lipid formation). Give a brief discussion for how this is possible. The response of a target cell to a hormone depends on both the hormone and the target cell. In part, these varied effects of hormones are possible because there are different mechanisms of hormone action. Hormones bind to and activate their specific receptors in different ways. Where are the receptors for lipid-soluble hormones? Lipid-soluble hormones, which can diffuse freely through the cell membrane, use target cell receptors that are found in the cytoplasm or nucleus of target cells. 157 Where are the receptors for water-soluble hormones? Water-soluble hormones, which cannot cross the cell membrane, use target cell receptors, integral proteins found on the cell surface of target cells. 1. ACTIVATION OF INTRACELLULAR RECEPTORS Name the lipid-soluble hormones and give a brief description of their mechanism of action at the target cell. Steroid hormones and thyroid hormones are lipid-soluble and easily pass through cell membranes. Upon entering a target cell, the hormone binds to and activates an intracellular receptor, located within the nucleus. The activated hormone-receptor complex than alters gene expression by turning specific genes of the nuclear DNA either on or off. This usually involves the synthesis of new enzymes that alter cellular metabolism in the way specific for that hormone, and in that way alters some function. 2. ACTIVATION OF PLASMA MEMBRANE RECEPTORS Name the water-soluble hormone and give a brief description of their mechanism of action at the target cell. Catecholamine, peptide, and protein hormones are water-soluble, cannot diffuse through the cell membrane, and therefore must utilize receptors on the target cell surface. Since the hormone can only bring the physiological message to the cell membrane of the target cell, rather than the nucleus, the hormone is called the first messenger. A second messenger is needed to relay the message from the receptor, through the cell membrane, and into the cytoplasm where the hormone-stimulated response can take place. The best known second messenger is cyclic 3’, 5’-monophosphate (cyclic AMP or camp). 158 The receptor is attached on its inner side to the enzyme adenylate cyclase. The enzyme is stimulated to convert intracellular ATP to cyclic AMP when the hormone binds to the receptor. Increased levels of intracellular cyclic AMP acts as a second messenger within the cell, directing a specific response that is celltype dependent. The increased cyclic AMP within the cell is transient, however, because of the intracellular enzyme phosphodiesterase, which quickly degrades cyclic AMP to 5’-AMP. 5’-AMP has no biological activity (therefore, the hormonal effect on the cell is tightly regulated) within the cell and is used to regenerate ATP. E. CONTROL OF HORMONAL SECRETIONS In general, how are hormone secretions controlled? Most endocrine glands secrete their product(s) in short bursts, with little or no secretion in between stimulations. Regulation of secretion depends on homeostasis and prevents over- or underproduction. Hormone secretion is stimulated and inhibited by signals from the nervous system, chemical changes in the blood, and other hormones. Most often, negative feedback systems maintain homeostasis for hormonal secretions. F. HYPOTHALAMUS AND PITUITARY GLAND (HYPOPHYSIS) What is the role of the hypothalamus in endocrine control? The hypothalamus serves as the master control for many of the hormones secreted by the endocrine system, and serves as the major integrator between the nervous and endocrine systems. In particular, the hypothalamus controls the secretions of the pituitary gland, also known as the hypophysis. 159 What is the anatomical relationship between the pituitary gland and the hypothalamus? The pituitary gland is a pea-sized organ lying within the sella turcica of the sphenoid bone. It is suspended from the base of the hypothalamus by the infundibulum, a stalk-like structure. Describe the pituitary gland by describing its embryologic formation. The pituitary gland has two anatomically and functionally distinct portions due to its embryological formation. The anterior pituitary gland (adenohypophysis) (about 75% of the total gland) is derived from an outpouching of the roof of the developing mouth, called Rathke’s pouch. Rathke’s pouch breaks off from the mouth and migrates as a unit to make contact with the forming posterior pituitary gland associated with the hypothalamus. The posterior pituitary gland (neurohypophysis) forms as an outgrowth of the base of the hypothalamus and remains attached to it via the infundibulum. The posterior pituitary gland contains axons and axon terminals of about 5,000 neurons whose cell bodies are located in nuclei in the hypothalamus. The nerve fibers that terminate in the posterior pituitary gland are associated with neuroglial-like support cells called pituicytes, which are secretory. Regardless of origin, both the anterior and posterior pituitary glands are wholly dependent upon the hypothalamus for regulation of hormonal secretion. Describe the anatomical mechanism by which the hypothalamus controls hormonal secretions from the anterior pituitary gland. The anatomical pituitary gland (adenohypophysis) secretes seven hormones that regulate a wide variety of bodily functions. Release of these hormones is dependent upon chemicals secreted by the hypothalamus called releasing and inhibiting factors (hormones). 160 These hypothalamic hormones reach the anterior pituitary gland through a system of blood vessels that connect the two regions. This system of vessels, called the hypophyseal portal system, consists of several superior hypophyseal arteries that enter the lower hypothalamic region and divide into the primary plexus of capillaries. The primary plexus is recollected into hypophyseal veins that pass down the infundibulum, enter the anterior pituitary gland, then divide into the secondary plexus of capillaries. The secondary plexus is then recollected into the anterior hypophyseal veins that exit the anterior pituitary gland and return the blood to the general circulation. The releasing and inhibiting factors secreted by hypothalamic neurons diffuse into the blood of the primary plexus and are carried by the portal system into the anterior pituitary. The factors diffuse out of the blood of the secondary plexus and into the interstitial fluid of the anterior pituitary, where they interact with their specific target cells. In response, the cells of the anterior pituitary may secrete specific hormones that diffuse into the blood of the secondary plexus and ultimately are distributed throughout the body. 1. ANTERIOR PITUITARY GLAND (ADENOHYPOPHYSIS) Name the seven hormones secreted by the anterior pituitary gland. growth hormone (GH) thyroid-stimulating hormone (TSH) follicle-stimulating hormone (FSH) luteinizing hormone (LH) prolactin (PRL) adrenocorticotropic hormone (ACTH) melanocyte-stimulating hormone (MSH) Tropic hormones (tropins) are those hormones that influence other endocrine glands to secrete their hormone (s). Name them. FSH LH TSH ACTH 161 a. GROWTH HORMONE Growth hormone (somatotropin or GH) stimulates protein synthesis, increased lipolysis, and the decreased use of glucose for ATP production, promoting hyperglycemia (the diabetogenic effect. GH causes cells to increase their rate of amino acid uptake from the blood, especially during childhood and adolescence, thus promoting increased protein anabolism. Control of GH secretion is via GH-Inhibiting Factor and GHReleasing Factor from the hypothalamus and is related to blood glucose concentration. Hypoglycemia inhibits GH-IF secretion, allowing GH-RF secretion and GH blood levels to rise. Hyperglycemia inhibits GH-RF secretion, allowing GH blood levels to fall. this promotes normoglycemia. 162 GROWTH HORMONE increased blood glucose (hyperglycemia) decreased blood glucose (hypoglycemia) (stimulates) (stimulates) increased hypothalamic secretion secretion of GH-IF increased hypothalamic of GH-RF (inhibits) (stimulates) anterior pituitary gland secretion of GH increased anterior pituitary gland secretion of GH (has the following effects) decreased blood glucose anabolism 1. increased protein 2. 3. increased lipolysis increased glycogenolysis (lead to) increased blood glucose normoglycemia (Normoglycemia feeds back to turn off both the hypothalamus and anterior pituitary gland so that both GH-IF and GH-RF secretions are inhibited) 163 b. THYROID-STIMULATING HORMONE HYPOTHALAMIC-PITUITARY-THYROID AXIS decreased basal metabolic rate (stimulates) increased hypothalamic secretion of TSH-RF (stimulates) increased anterior pituitary gland secretion of TSH (stimulates) increased thyroid gland secretion of T3 and T4 (thyroxine) (has the following effects)) 1. 2. 3. increasing carbohydrate catabolism increasing fat catabolism increasing protein anabolism (lead to) increased basal metabolic rate (This feeds back to turn off both the hypothalamus and anterior pituitary gland so that TSH-RF and TSH blood levels decline) 164 c. FOLLICLE-STIMULATING HORMONE HYPOTHALAMIC-PITUITARY-GONADAL AXIS (male – follicle stimulating hormone) decreased blood levels of inhibin (stimulates) increased hypothalamic secretion of gonadotropin-RF (stimulates) increased anterior pituitary gland secretion of FSH (stimulates) 1. 2. increased spermatogenesis increased activity of Sertoli cells (leading to) increased secretion of inhibin by Sertoli cells (Inhibin feeds back to turn off both the hypothalamus and anterior pituitary gland so that Gn-RF and FSH blood levels decline) 165 HYPOTHALAMIC-PITUITARY-GONADAL AXIS (female – follicle stimulating hormone) decreased blood levels of estrogen (stimulates) increased hypothalamic secretion of gonadotropin-RF (stimulates) increased anterior pituitary gland secretion of FSH (stimulates) development of ovarian follicles (has the following effects)) 1. 2. increasing blood levels of estrogen maturation of an egg for ovulation (leads to) increased blood estrogen (This feeds back to turn off both the hypothalamus and anterior pituitary gland so that Gn-RF and FSH blood levels decline) 166 d. LUTEINIZING HORMONE HYPOTHALAMIC-PITUITARY-GONADAL AXIS (male – luteinizing hormone) decreased blood levels of testosterone (stimulates) increased hypothalamic secretion of gonadotropin-RF (stimulates) increased anterior pituitary gland secretion of LH (stimulates) increased secretion of testosterone (has the following effects)) support of all male secondary sex characteristics (Testosterone feeds back to turn off both the hypothalamus and anterior pituitary gland so that Gn-RF and FSH blood levels decline.) 167 HYPOTHALAMIC-PITUITARY-GONADAL AXIS (female – luteinizing hormone) increased blood levels of estrogen (stimulates) increased hypothalamic secretion of gonadotropin-RF (stimulates) increased anterior pituitary gland secretion of LHH (stimulates) 1. 2. directly stimulates ovulation, which leads to formation of the corpus luteum (has the following effects)) ovulation (leads to) formation of the corpus luteum (After ovulation, blood estrogen falls below the level necessary ot stimulate the anterior pituitary gland. Therefore, this is not really inhibition of LH secretion. The anterior pituitary gland cannot secrete LH without sufficient blood estrogen.) 168 e. PROLACTIN PROLACTIN (female only) increased estrogen during initiated by last half of menstrual cycle nipple neuroendocrine reflex suckling of postpartum (stimulates) increased hypothalamic secretion of PRL-IF (stimulates) increased hypothalamic secretion of PRL-RF (inhibits) anterior pituitary gland secretion of PRL (stimulates) increased anterior pituitary gland secretion of PRL has the following effects) decreased blood PRL by mammary increased milk synthesis gland cells (not secretion) 169 f. MELANOCYTE-STIMULATING HORMONE MELANOCYTE STIMULATING HORMONE increased hypothalamic secretion ofsecretion of MSH-IF (inhibits) anterior pituitary gland secretion of MSH increased hypothalamic MSH-RF (stimulates) increased anterior pituitary gland secretion of MSH (stimulates) increased skin pigmentation by stimulation of melanocytes gland cells (not secretion) (This hormone is poorly understood.) 170 g. ADRENOCORTICOTROPIC HORMONE HYPOTHALAMIC-PITUITARY-ADRENAL AXIS increased stress or decreased blood levels of glucocorticoids (stimulates) increased hypothalamic secretion of corticotropin-RF (stimulates) increased anterior pituitary gland secretion of ACTH (stimulates) increased adrenal cortex gland secretion of glucocorticoids (cortisol) (has the following effects)) 1. promote normal metabolism and ensure glucose availability by: increasing protein catabolism increasing gluconeogenesis increased lipolysis 2. provide resistance to stress by: increased mental alertness increased energy increased blood pressure 3. increased anti-inflammatory activity by: stabilizing cell membranes depressing phagocytosis decreased capillary permeability (decreased swelling) (lead to) decreased stress (This feeds back to turn off both the hypothalamus and anterior pituitary gland so that CRF and ACTH blood levels decline) 171 2. POSTERIOR PITUITARY GLAND (NEUROHYPOPHYSIS) Describe the posterior pituitary gland and the way it is controlled by the hypothalamus. The posterior pituitary gland (neurohypophysis), in a strict sense, is not an endocrine organ at all since the hormones released from the gland are actually synthesized by neurons in the hypothalamus. In the axon terminals of the neurons that pass down the infundibulum and terminate among the pituicytes are synaptic vesicles filled with one of two hormones: oxytocin and antidiuretic hormone (ADH). An action potential in one of these neurons causes the release of the hormone into the extracellular fluid of the posterior pituitary, where it will diffuse into the blood for distribution throughout the body. These axons passing from the hypothalamus are collected together as the hypothalamo-hypophyseal tract. a. OXYTOCIN What are the functions of oxytocin? Oxytocin stimulates the contraction of uterine smooth muscle during delivery of the baby and placenta. After birth, oxytocin stimulates contraction of the myoepithelial cells of the mammary glands, causing milk ejection (letdown) from the breast. How is oxytocin secretion controlled? Both events are controlled by a neuroendocrine reflex in which stretch of the cervix or tactile stimulation of the nipple initiates sensory impulses that terminate on the appropriate neurons of the hypothalamus. Stimulation of these neurons results in the release of oxytocin into the posterior pituitary gland. What is the role of oxytocin in males and nonpregnant females? In the nonpregnant and postpartum nonnursing female and in the male, the role of oxytocin is unknown. 172 OXYTOCIN (female only) increased stretch of the postpartum pregnant cervix tactile stimulation of areola and nipple (stimulates) (stimulates) increased activity of hypothalamic neurons increased activity of hypothalamic neurons (stimulates) (stimulates) posterior pituitary gland neurosecretion of oxytocin posterior pituitary gland neurosecretion of oxytocin (stimulates) (stimulates) contraction of uterine smooth muscle during labor and delivery contraction of mammary gland myoepithelial cells, resulting I milk letdown (This system requires the hormones of pregnancy to properly prime the uterus and mammary gland cells so that they are responsive to oxytocin.) b. ANTIDIURETIC HORMONE What is an antidiuretic? An antidiuretic is any chemical substance that prevents excessive urine formation. What are the functions of ADH? The principal effect of ADH is to cause the kidneys to remove water from the forming urine and return it to the blood, thus conserving it. ADH also causes decreased perspiration and vasoconstriction of blood vessels. All efforts of ADH are related to maintaining normal blood pressure. 173 How is ADH secretion controlled? The neurons of the hypothalamus that secrete ADH are osmoreceptors and detect high osmotic pressure in the extracellular fluid. Increased osmolarity stimulates the neurons to create an action potential that results in the release of ADH. Decreased osmolarity inhibits ADH secretion. What is diabetes insipidus? Diabetes insipidus results when there is too little ADH secretion. As a result, the kidneys conserve much less water than usual and daily urine output may be as much as 10-fold normal. ANTIDIURETIC HORMONE (VASOPRESSIN) increased extracellular fluid osmolarity (stimulates) hypothalamic neurosecretory osmoreceptors (leading to) posterior pituitary gland secretion of ADH (has the following effects) 1. 2. increased water reabsorption by kidney tubule cells increased thirst (leading to) increased extracellular fluid volume and therefore decreased body osmolarity (Decreased extracellular fluid osmolarity feeds back to turn off the hypothalamic osmoreceptors and blood levels of ADH decline.) 174 G. THYROID GLAND Describe the thyroid gland. The thyroid gland is located just below the larynx in the anterior neck, consisting of a right and left lateral lobe, and a central portion called the isthmus. The gland itself consists of microscopic spherical sacs or follicles formed by the follicular cells. Name the hormones secreted by the follicular cells. Follicular cells secrete two hormones that are closely related: 1. triiodothyronine (T3), with three iodine atoms, and 2. tetraiodothyronine (T4 or thyroxine), with four iodine atoms What are parafollicular cells? Between the follicles, lying in small nests, are the parafollicular (C-) cells that secrete the hormone calcitonin. 1. FORMATION, STORAGE, AND RELEASE OF THYROID HORMONES Describe the synthesis pathway for thyroxine. The thyroid gland is the only endocrine gland that stores its secretory product in large quantity, normally about a 10-day supply. In essence, the thyroid gland captures iodide ions, which are then stored in the cytoplasm of the follicular cells until needed. The follicular cells synthesize a glycoproteins called thyroglobulin, which has tyrosine molecules along its length, and secrete it into the center of the follicle. The iodide ions are moved out of the cells and into the center of the follicle to iodinate the tyrosine residues, forming colloid, the storage form of T3 and T4. When stimulated by TSH from the anterior pituitary gland, the follicular cells remove colloid from the follicle center and enzymatically remove the T3 and T4 molecules from the thyroglobulin. The follicular cells then secrete the T3 (triiodothyronine) and T4 (tetraiodothyronine or thyroxine) molecules, into the extracellular space around the follicle so they can diffuse into the blood. 175 2. 3. ACTIONS OF THYROID HORMONES CONTROL OF THYROID HORMONE SECRETION Describe the functions of thyroxine and the control of its secretion. The major action of thyroxine is to regulate all metabolic processes of the body cells by stimulating the following: 1. increased carbohydrate catabolism 2. increased fat catabolism 3. increased protein anabolism The net result is an increase in catabolism, thereby increasing the basal metabolic rate (BMR) and raising body temperature (the calorigenic effect). In addition, thyroxine is required for normal growth and development of children, particularly of the nervous system (cretinism results from too little thyroxine during development). Thyroxine secretion is controlled by TSH secretion from the anterior pituitary, which is itself controlled by TSH-RF from the hypothalamus, which is controlled by the BMR, the blood glucose level, and the T4 concentration. 176 HYPOTHALAMIC-PITUITARY-THYROID AXIS decreased basal metabolic rate (stimulates) increased hypothalamic secretion of TSH-RF (stimulates) increased anterior pituitary gland secretion of TSH (stimulates) increased thyroid gland secretion of T3 and T4 (thyroxine) (has the following effects)) 1. 2. 3. increasing carbohydrate catabolism increasing fat catabolism increasing protein anabolism (lead to) increased basal metabolic rate (This feeds back to turn off both the hypothalamus and anterior pituitary gland so that TSH-RF and TSH blood levels decline) 4. CALCITONIN Describe the role of calcitonin in calcium homeostasis. The second major cell population of the thyroid gland is the parafollicular (C-) cell. These cells are located between the thyroid follicles. They secrete the hormone calcitonin. Calcitonin works antagonistically with parathyroid hormone (PTH) to maintain blood calcium levels between 9.5 – 10.5 mg%. 177 The C-cells have receptors that monitor extracellular fluid calcium concentration. They are stimulated to secrete calcitonin when blood calcium levels exceed 10.5 mg% (hyperglycemia). Calcitonin works to decrease serum calcium by: 1. inhibiting osteoclasts 2. stimulating osteogenesis 3. decreasing calcium reabsorption by the kidneys When blood calcium levels drop back below 10.5 mg%, the C-cells are inhibited and no longer secrete calcitonin. CALCITONIN blood calcium > [10.5 mg%] (hypercalcemia) (stimulates) parafollicular cells of the thyroid gland (leading to) increased secretion of calcitonin (has the following effects) 1. 2. 3. decreased bone resorption increased bone formation decreased calcium reabsorption by kidneys (leading to) decreased blood calcium concentration (normocalcemia) (Blood calcium < [10.5 mg%] feeds back to turn off calcitonin secretion.) 178 H. PARATHYROID GLANDS AND PARATHYROID HORMONE Describe the parathyroid glands and the role of parathyroid hormone (PTH) in calcium homeostasis. There are four parathyroid glands embedded into the posterior surface of the thyroid gland. The glands consist of two cell types: 1. chief cells that secrete parathyroid hormone (PTH) 2. oxyphil cells – function unknown PTH works antagonistically with calcitonin to regulate the blood concentration of calcium and is secreted by chief cells under conditions of PTH works antagonistically with calcitonin to regulate the blood concentration of calcium and is secreted by chief cells under conditions of hypocalcemia (<9.5 mg%). PTH works to increase blood calcium levels by: 1. activating osteoclasts 2. increasing calcium reabsorption by the kidneys 3. increasing calcium absorption by the gut 4. stimulating secretion of vitamin D (similar effects as PTH) When blood calcium levels rise above 9.5 mg%, the chief cells are inhibited and no longer secrete PTH. 179 PARATHYROID HORMONE blood calcium < [9.5 mg%] (hypocalcemia) (stimulates) chief cells of the parathyroid glands (leading to) increased secretion of PTH (has the following effects) 1. 2. 3. increased bone resorption decreased bone formation increased calcium reabsorption by kidneys (leading to) increased blood calcium concentration (normocalcemia) (Blood calcium > [9.5 mg%] feeds back to turn off PTH secretion.) I. ADRENAL (SUPRARENAL) GLANDS Describe the adrenal glands. The paired adrenal (suprarenal) glands, each lying just superior to each kidney, are structurally and functionally divided into two separate glands: the adrenal cortex and the adrenal medulla. What are steroids? All hormones secreted by the adrenal cortex are called steroid hormones, lipid molecules whose chemical structure is derived from cholesterol. 180 1. ADRENAL MEDULLA, EPINEPHRINE, AND NOREPINEPHRINE Describe the adrenal medulla and its hormones. The adrenal medulla, the inner portion of the gland, consists of chromaffin cells that secrete the catecholamines epinephrine and norepinephrine. These cells receive direct innervation from sympathetic preganglionic neurons. In response, they secrete these catecholamines and add to the fight-or-flight response. 2. ADRENAL CORTEX Name the three zones of the adrenal cortex. The adrenal cortex is subdivided into three zones, each of which has a different cellular arrangement and secretes a different class of steroids. a. MINERALOCORTICOIDS What are the mineralocorticoids? The mineralocorticoids are the class of steroids produced by the outermost zone of the adrenal cortex, the zona glomerulosa. Aldosterone is the primary mineralocorticoid and, like all the steroids of this class, work to control water and electrolyte balance, particularly by controlling sodium and potassium concentrations. Under normal conditions, aldosterone secretion is in response to high potassium ion concentration in the extracellular fluid. Aldosterone stimulates kidney cells to lose potassium ions into the forming urine, while at the same time conserving sodium ions and, by osmosis, water. Describe control of aldosterone secretion by the renin-angiotensin system and its role in homeostasis. During times of dehydration, hemorrhage, or sodium deficiency, aldosterone secretion may be stimulated via the 181 renin-angiotensin system. This is related to blood pressure control. Decreased blood volume causes decreased blood pressure, which in turn causes the kidneys to secrete renin. Renin converts the inactive plasma protein angiotensinogen to angiotensin I. As angiotensin I passes through the lungs in the blood it is converted to angiotensin II. Angiotensin II stimulates aldosterone secretion, which causes increased sodium reabsorption and therefore water reabsorption. As a result, blood volume increases and therefore blood pressure rises. This is an important long-term compensatory mechanism for blood pressure control. It will be discussed in greater detail with the kidneys 182 MINERALOCORTICOIDS (RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM) dehydration sodium deficiency hemorrhage Above the dashed line represents compensatory changes in response to decreased blood pressure. (leading to) Below the dashed line shows the normal physiologic control mechanism for aldosterone secretion decreased blood volume (leading to) increased blood pressure decreased blood pressure (leading to) increased renin secretion from kidney (converts) angiotensinogen angiotensin I (converted in lungs to) increased blood volume angiotensin II (effects) increased water retention by kidneys 1. 2. 3. systemic vasoconstriction increased thirst increased ADH secretion increased sodium reabsorption 4. increased aldosterone by kidneys secretion --------------------------------------------------------------------------------------------------------------------decreased K+ (stimulates) reabsorption by kidneys (inhibits) increased K+ in blood (leads to) loss of potassium into urine decreased K+ in blood 183 b. GLUCOCORTICOIDS What are glucocorticoids? The glucocorticoids are the class of steroids produced by the middle zone of the adrenal cortex, the zona fasciculate. The predominant glucocorticoids are hydrocortisone, cortisone, and corticosterone. What controls their secretion? Glucocorticoids are secreted in response to ACTH from the anterior pituitary, which is controlled by corticotropic-RF from the hypothalamus. C-RF secretion is in response to stress. Reduction in stress inhibits C-RF and therefore ACTH and the glucocorticoids. What are their principal effects? Glucocorticoids have the following effects: 1. increased gluconeogenesis, thus increasing available glucose for body cells for normal metabolism and to combat stress 2. inhibition of the inflammatory response 184 HYPOTHALAMIC-PITUITARY-ADRENAL AXIS increased stress or decreased blood levels of glucocorticoids (stimulates) increased hypothalamic secretion of corticotropin-RF (stimulates) increased anterior pituitary gland secretion of ACTH (stimulates) increased adrenal cortex gland secretion of glucocorticoids (cortisol) (has the following effects)) 1. promote normal metabolism and ensure glucose availability by: increasing protein catabolism increasing gluconeogenesis increased lipolysis 2. provide resistance to stress by: increased mental alertness increased energy increased blood pressure 3. increased anti-inflammatory activity by: stabilizing cell membranes depressing phagocytosis decreased capillary permeability (decreased swelling) (lead to) decreased stress (This feeds back to turn off both the hypothalamus and anterior pituitary gland so that CRF and ACTH blood levels decline) 185 c. GONADOCORTICOIDS Briefly describe the gonadocorticoids. The gonadocorticoids are the class of steroids produced by the innermost zone of the adrenal cortex, the zona reticularis. these steroids are the male androgens and the female estrogens. During reproductive left, the concentration of these hormones from the adrenal cortex is of little importance because of gonadal secretion. their secretion during development, childhood, and after menopause does contribute to normal metabolism. J. PANCREAS Describe the pancreas. The pancreas is both an exocrine organ related to digestion and an endocrine gland. It is a flattened organ located posterior and just inferior to the stomach. Scattered throughout the exocrine portion of the gland are small islands of cells called the islets of Langerhans. Describe the cell types of the islets of Langerhans? Islets are composed of four cell types: 1. alpha cells that secrete glucagon 2. beta cells that secrete insulin 3. delta cells that secrete somatomedin (GH-IF) 4. F-cells that are related to digestion 1. GLUCAGON Describe the role of glucagon in maintaining glucose homeostasis. Glucagon works antagonistically with insulin to maintain blood glucose levels within homeostatic range (90 – 110 mg%). The alpha cells of the islets of Langerhans bear receptors for glucose that monitor the extracellular fluid for glucose concentration. Under conditions of hypoglycemia (<90 mg%), the alpha cells are stimulated to secrete glucagon. 186 Glucagon works to raise blood glucose by: 1. increasing glycogenolysis (glycogen breakdown) 2. increasing gluconeogenesis (formation of glucose from other sources, such as amino acids). When blood glucose concentration rises above 90 mg%, the alpha cells are inhibited and glucagon secretion stops. GLUCAGON blood glucose < [90 mg%] (hypoglycemia) (stimulates) alpha cells of the islets of Langerhans in the pancreas (leading to) increased secretion of glucagon (has the following effects) 1. 2. increased glycogenolysis increased gluconeogenesis (leading to) increased blood glucose concentration (normoglycemia) (Blood glucose > [90 mg%] feeds back to turn off glucagon secretion.) 2. INSULIN Describe the role of insulin in maintaining glucose homeostasis. Insulin works antagonistically with glucagon to maintain blood glucose levels within homeostatic range (90 – 110 mg%) or normoglycemia. Beta cells of the islets of Langerhans bear receptors for glucose that monitor the extracellular concentration for conditions of hyperglycemia (>110 mg%). 187 When blood glucose levels exceed 110 mg%, the beta cells are stimulated to secrete insulin. Insulin decreases blood glucose by: 1. increasing cell uptake of glucose 2. increasing glycogenesis 3. decreasing glycogenolysis 4. decreasing gluconeogenesis 5. increasing lipogenesis When blood glucose levels fall back into the normoglycemic range (<110 mg%), the beta cells are inhibited and insulin secretion is stopped. INSULIN blood glucose > [110 mg%] (hyperglycemia) (stimulates) beta cells of the islets of Langerhans in the pancreas (leading to) increased secretion of insulin (has the following effects) 1. 2. 3. 4. increased cellular uptake of glucose from the blood (particularly liver, skeletal muscle, and adipose cells) increased glycogenesis increased lipogenesis increased protein anabolism (leading to) decreased blood glucose concentration (normoglycemia) (Blood glucose < [110 mg%] feeds back to turn off insulin secretion.) 188 K. THE GENERAL ADAPTATION SYNDROME Review the stages and events of the general adaptation syndrome. Three phases: 1. Alarm phase – immediate short-term responses to stressors, causing fight-or flight, which might lead to the 2. Resistance phase – long-term metabolic adjustments to provide resistance to the stressors, which might lead to 3. Exhaustion phase – collapse of vital systems as resistance efforts fail to counteract stressors. In the alarm phase, stress stimulates the hypothalamus, leading to general sympathetic action and activation of the adrenal medulla. This leads to secretion of norepinephrine and epinephrine, causing fight-or-fight. During the resistance phase, a number of hormones cause the following effects: 1. mobilization of remaining energy reserves from lipid and muscle 2. conservation of glucose 3. elevation of blood glucose level 4. decreased inflammatory response 5. conservation of sodium and water 6. increased blood pressure Continued use of resistance phase to counter the effects of stress eventually leads one into the exhaustion phase. Causes of multisystem collapse may be due to: 1. exhaustion of lipid (energy) reserves 2. depressed immune response 3. failure of electrolyte balance 4. cardiac and/or renal failure The net result of the exhaustion phase is death. 189