* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download this is blood clotting
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
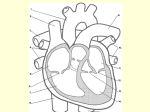
CHAPTERS 11 & 12 BLOOD AND THE HEART FUNCTIONS OF THE BLOOD 1. Transport of dissolved gasses, nutrients, hormones, and metabolic wastes 2. Regulation of pH and electrolyte (ions) composition of fluids in the body 3. Restriction of fluid losses through damaged vessels or other sites of injury 4. Defense against toxins and pathogens 5. Stabilization of body temperature COMPOSITION OF BLOOD Blood consists of a matrix called PLASMA and formed elements PLASMA- contains dissolved proteins; is slightly denser than water FORMED ELEMENTS- blood cells and cell fragments that are suspended in the plasma - Erythrocytes (red blood cells, RBCs), Leukocytes (white blood cells, WBCs), platelets Together plasma and formed elements form WHOLE BLOOD - an adult man has about 5-6 liters of blood - an adult woman has about 4-5 liters Whole blood has the same physical characteristics: - temperature of 38º C (100.4º F) - viscosity 5X greater than water - pH averaging 7.4 CLOSER LOOK AT PLASMA Plasma makes up about 55% of the volume of whole blood PLASMA PROTEINS - the large size of most blood proteins prevents them from crossing capillary walls 3 Primary Classes of Proteins: 1. Albumins- most abundant; major contributors to osmotic pressure of the plasma 2. Globulins- include antibodies and transport proteins - Antibodies attack foreign proteins and pathogens - Transport proteins bind small ions, hormones, or compounds that might otherwise be filtered out of the blood at the kidneys 3. Fibrinogens- function in blood clotting - under certain conditions, these molecules interact and combine to form large strands of FIBRIN, which provide the basic framework for a blood clot The liver synthesizes most of the plasma proteins - liver disorders can alter the composition and functional properties of the blood CLOSER LOOK AT FORMED ELEMENTS HEMOPOIESIS- production of formed elements - embryonic blood cells appear in bloodstream during the 3rd week of development - these cells divide rapidly - the vessels of the yolk sac, an embryonic membrane, are the primary site of blood formation for the first 8 weeks of development - as other organs appear, some of these cells move out of the bloodstream into the liver, spleen, thymus, and bone marrow - these embryonic cells differentiate into STEM CELLS that produce blood cells by their divisions - liver and spleen are the primary sites of hemopoiesis from the 2nd to 5th months of development - as the skeleton enlarges, bone marrow becomes increasingly important, and is the primary site after the 5th month of development - in adults, marrow is the only site of RBC production, and the primary site of WBC production RED BLOOD CELLS (RBCs) - contain the pigment HEMOGLOBIN, which binds, and transports O2 and CO2 - most abundant blood cells, making up 99% of the formed elements HEMATOCRIT- the percentage of whole blood occupied by cellular elements RBCs containing hemoglobin with bound oxygen give blood a bright red color RBCs containing hemoglobin NOT bound to oxygen give blood a dark red, almost burgundy color Carbon Monoxide Poisoning RBCs AND BLOOD TYPES ANTIGENS- substances that can trigger an immune response - cell membranes contain surface antigens, substances that the body’s immune defenses recognize as “normal” A person’s blood type is a classification determined by the presence or absence of specific surface antigens - the characteristics of RBC surface antigen molecules are genetically determined All of the RBCs of any individual have the same pattern of surface antigens - Type A blood has antigen A only - Type B blood has antigen B only - Type AB blood has both A and B - Type O blood has neither A nor B * type O is the most common, followed by A, B, then AB ANTIBODIES AND CROSSREACTIONS Plasma contains antibodies or AGGLUTININS that will attack surface antigens on foreign cells - the plasma of an individual with type A blood contains circulating anti-B antibodies which will attack Type B surface antigens - Type O blood lacks surface antigens A or B, so plasma contains BOTH anti-A and anti-B antibodies - Type AB have no A or B antibodies If an antibody meets an antigen, a CROSSREACTION occurs - the RBCs will clump together, called AGGLUTINATION - then they may break up or hemolyze - these clumps can clog blood vessels The plasma of an Rh-negative individual does not contain anti-Rh antibodies - Rh is another surface antigen - these antibodies are present only if the individual has been sensitized by previous exposure to Rh-positive RBCs * can happen if an Rh-negative mother gives birth to an Rh-positive baby WHITE BLOOD CELLS (WBCs) White blood cells are easily distinguishable from red blood cells because each has a nucleus and lacks hemoglobin - WBCs help defend the body against invasion by pathogens and remove toxins, wastes, and abnormal or damaged cells WBCs are divided into 2 groups, based on their appearance after staining: 1. Granulocytes- have many stained granules 2. Agranulocytes- have few if any stained granules - the “granules” are secretory vesicles and lysosomes; agranulocytes also contain lysosomes, they are just more difficult to see Granulocytes: neutrophils, eosinophils, basophils Agranulocytes: monocytes, lymphocytes - most of the WBCs in the body are found in connective tissue proper and in organs of the lymphatic system; very few are circulating General Functions of WBCs Basophils, neutrophils, eosinophils, and monocytes contribute to the body’s nonspecific defenses of the immune system - they do not discriminate between one type of threat and another Lymphocytes are responsible for specific immunity - this is the body’s ability to attack pathogens on a specific, individual basis PLATELETS Platelets in nonmammalian vertebrates are nucleated cells called THROMBOCYTES - because in humans they are cell fragments rather than individual cells, the term platelet is used when referring to our blood Bone marrow contains very large cells with large nuclei called MEGAKARYOCYTES - these continuously shed cytoplasm in small membrane-enclosed packets - these are platelets - platelets initiate the clotting process and help close injured blood vessels - they are continuously replaced HEMOSTASIS HEMOSTASIS- the process that stops bleeding - prevents the loss of blood through the walls of damaged vessels STEP 1: The vascular phase - smooth muscle fibers lining a blood vessel contract, decreasing the diameter of the vessel - lasts about 30 minutes - membranes of cells at the injury site become sticky, and may stick together to block the opening STEP 2: The platelet phase - platelets begin to attach to the sticky cell membranes and exposed collagen fibers within 15 seconds of the injury - as more platelets arrive, they form a PLATELET PLUG, which may also close the opening STEP 3: Coagulation phase - does not start until 30 seconds or more after injury - this is blood clotting - circulating fibrinogen is converted into the insoluble protein fibrin - blood cells and additional platelets become trapped in the protein forming a BLOOD CLOT CLOTTING PROCESS Normal coagulation cannot occur unless plasma contains the necessary CLOTTING FACTORS - these include calcium ions, and 11 different plasma proteins - these proteins are converted to active enzymes that direct essential reactions in the clotting response - most of these are produced by the liver THE HEART AND CIRCULATORY SYSTEM Blood vessels are subdivided into a: PULMONARY CIRCUIT- carries blood to and from exchange surfaces of the lungs SYSTEMIC CIRCUIT- transports blood to and from the rest of the body - each circuit begins at the heart, and blood travels though these circuits in sequence ARTERIES- carry blood away from the heart VEINS- carry blood to the heart CAPILLARIES- small, thin-walled vessels between the smallest arteries and veins - the thin walls of the capillaries permit exchange of nutrients, gases, and waste products between the blood and surrounding tissue STRUCTURE OF THE HEART The heart is a hollow, muscular organ located in the thoracic cavity between the lungs and above the diaphragm - 2/3 of its mass lies to the left of the middle line of the body - size usually corresponds to the size of the person’s clenched fist - the weight of the heart depends on the individual’s size, sex, and age - in embryonic development, the heart has a fixed number of cardiac muscle cells that are present at birth and remain through life- growth of the heart is due to an increase in the size of the cells Pericardial Sac The heart and the base of the heart’s major blood vessels are enclosed in a slippery, loose-fitting sac called the PERICARDIUM 2 Layers: PARIETAL PERICARDIUM- external layer that is attached to the diaphragm, sternum, and blood vessels VISCERAL PERICARDIUM- inner layer that adheres to the heart wall; also called EPICARDIUM Between the 2 layers is a narrow space called the PERICARDIAL CAVITY - this is filled with PERICARDIAL FLUID, a slippery fluid that prevents friction between the membranes A = Visceral pericardium B = Parietal pericardium Heart Wall 3 distinct layers make up the heart wall: EPICARDIUM (visceral pericardium)external layer of wall - usually contains fat MYOCARDIUM- comprises the bulk of the heart - consists of cardiac muscle fibers that are involuntary - this layer is responsible for the contracting action of the heart ENDOCARDIUM- inner layer; thin membrane of endothelial and connectivetissue cells - covers all of inner surface, even the valves Chambers and Valves The heart is divided into right and left halves, and then each side into upper and lower chambers ATRIA- upper chambers - separated by the INTERATRIAL SEPTUM VENTRICLES- lower chambers - separated by INTERVENTRICULAR SEPTUM On the outer surface of each atrium is an external flap called an AURICLE - can be seen when atrium is not filled with blood On the surface of the interatrial septum is an oval depression called the FOSSA OVALIS - this is a remnant of an oval hole called the FORAMEN OVALE through which blood passes in the fetal heart - in the fetus the blood passes directly from the right side to the left side without passing through the lungs to become oxygenated - Lungs only begin to function as an oxygen source after birth- the hole closes - RIGHT- only gets DEOXYGENATED blood - LEFT- only gets OXYGENATED blood from lungs APEX- inferior tip of heart 2 types of valves 1. ATRIOVENTRICULAR VALVES - Tricuspid - Bicuspid (Mitral) 2. SEMILUNAR VALVES - Pulmonary Semilunar Valve - Aortic Semilunar Valve TRICUSPID- located between the right atrium and right ventricle - consists of 3 irregularly shaped flaps or cusps formed by fibrous tissue - pointed ends point in toward ventricle - attached by cords called CHORDAE TENDINEAE to small muscular projections called the PAPILLARY MUSCLES The PAPILLARY MUSCLES are found along the inner surface of the ventricles The left atrioventricular opening is guarded by the BICUSPID or MITRAL VALVE - consists of 2 flaps or cusps - heavier and stronger than the tricuspid valve because the left ventricle exerts greater force in its contraction - its cusps are also attached to chordae tendineae and papillary muscles The second type of valve is found where the 2 major arteries (pulmonary and aorta) leave the ventricles - they are crescent moon shaped and have 3 flaps PULMONARY SEMILUNAR VALVEprevents blood in the pulmonary artery from reentering the right ventricle AORTIC SEMILUNAR VALVE- prevents blood from reentering the left ventricle as it enters the aorta DIFFERENCES BETWEEN LEFT AND RIGHT VENTRICLES The demands on the right and left atria are very similar, so they look almost identical Demands on the right and left ventricles are very different - the lungs are close to the heart, and the pulmonary arteries and veins are short and wide - the right ventricle does not need to push very hard to pump blood through the pulmonary circuit - the wall of the right ventricle is thin Pushing blood through the systemic circuit takes 6-7 times more force than around the pulmonary circuit - the left ventricle has a very thick muscular wall - as the left ventricle contracts, it bulges into the right ventricular cavity and helps force blood out of the right ventricle BLOOD SUPPLY TO THE HEART The heart has its own extensive blood supply - the CORONARY ARTERIES supply the myocardium with blood - the left coronary artery and the right coronary artery are the first branches of the aorta - from the arteries, blood empties into the coronary veins, then the coronary sinus which empties into the right atrium HEARTBEAT How can the heart contract without direct control by the brain or spinal cord? - a specialized conducting system is found within the heart- a network of specialized cardiac muscle cells that initiate and distribute electrical impulses The network is made up of 2 types of cardiac muscle cells that do not contract: 1. Nodal cells 2. Conducting cells Nodal Cells - responsible for establishing the rate of cardiac contraction Nodal cells are electrically coupled to one another, to conducting cells, and to normal cardiac muscle cells - when action potential appears in a nodal cell, it sweeps though the conducting system, reaching all of the cardiac muscle tissue and causing a contraction - so nodal cells determine heart rate Normal rate of contraction is established by PACEMAKER CELLS, nodal cells that reach threshold first - these are located in the SINOATRIAL NODE (SA node) or cardiac pacemaker, a tissue mass embedded in the posterior wall of the right atrium near the entrance of the superior vena cava - pacemaker cells depolarize rapidly, resulting in a heart rate of 70-80 beats per minute Conducting Cells The cells of the SA node are electrically connected to those of a larger ATRIOVENTRICULAR NODE (AV node) by conducting cells in the atrial walls The Conducting System Consists of 3 structures: 1. Sinoatrial Node (SA Node)- mass of specialized myocardial cells embedded in the wall of the right atrium, near where the superior vena cava enters the heart - this structure initiates each heart beat and sets the pace for the heart- called PACEMAKER Electrical activity of the SA node occurs on average of 70 to 72 times per minute and excites both atria at about the same time 2. ATRIOVENTRICULAR NODE (AV NODE)- after each atrial contraction, an impulse reaches the AV node - located at the base of the right atrium near the interatrial septum - a delay occurs for about 0.1 second which allows the atria to contract and empty their contents into the ventricles - the impulse then travels over the connecting link, the AV bundle 3. ATRIOVENTRICULAR BUNDLE (AV BUNDLE)- consists of a group of specialized cardiac muscle fibers adapted for conduction - the bundle divides and passes down each side of the interventricular septum to form the PERKINJE NETWORK- the conducting system within the walls of the ventricles - contraction proceeds from the inferior portions of the ventricles upward, ensuring that the blood leaves the ventricles through the arteries The Cardiac Cycle CARDIAC CYCLE- sequence of heart action 3 stages: 1. Blood enters the atria through the pulmonary veins and the superior and inferior venae cavae 2. The pulmonary circuit brings blood from the lungs while the systemic circuit returns blood from the head, neck, arms, thorax, trunk, and legs 3. The right atrium receives blood from the heart wall itself through the coronary sinus Diastolic and Systolic Phases DIASTOLE- the process of filling the atria and ventricles - this is a period of relaxation in which the chambers become distended - followed by a period of active contraction called SYSTOLE, which is marked by a shortening of the muscle bundles - the total time for a complete cycle is about 0.8 seconds CONTROL OF THE HEART Heart is affected by a number of influences: - Heart rate is affected by the secretions of endocrine - Hormones secreted by the thyroid and adrenal glands increase heart rate- fright or stress CHEMICAL INFLUENCE Many chemical compounds affect the heart - ATROPINE- active substance that comes from the deadly plant nightshade Greatly accelerates heartbeat - MUSCARINE- poisonous substance found in some mushrooms Inhibits heart action to the point where the heart stops beating completely - NICOTINE Blood pressure is raised Pulse rate is increased and there is a constriction of the coronary arteries Body temperature in extremities is decreased due to the constriction of blood vessels RATE OF HEART BEAT Heart rate is affected by several factors: - age - sex - position of body - amount of physical activity - temperature of surroundings - thought processes - heart rate is faster before birth and steadily declines after birth until a constant average is reached - females usually have a faster heartbeat than males EKG As with all muscles, the heart develops an electric current when it contracts - this is a result of the movement of ions across cell membranes > ACTION CURRENT ELECTROCARDIOGRAPH- instrument that measures and records the electric current ELECTROCARDIOGRAM (EKG)- resulting record Heart Sounds STETHOSCOPE- instrument to measure the sound of the heart WHY DO DOCTORS LISTEN TO THE HEART? - by noting the beginning and ending of the ventricular systole (contraction), one can time other events in the cardiac cycle - indicate the condition of the atrioventricular and semilunar valves 2 heart sounds: 1. Result of the closing of the atrioventricular valves and the contraction of the muscles in the walls of the ventricles - the instant at which the atrioventricular valves close - sounds like a lub - best heard right over the heart, between the 5th and 6th ribs 2. Represents the sudden closing of the semilunar valves - sounds like dub and is shorter in duration than the first sound - best heard between the 2nd and 3rd ribs, near the sternum HEART DISORDERS Every heart has the ability to perform work - if a heart is abnormal at birth, or if an individual develops certain risk factors, the life span of the heart may be shortened Risk Factors: High cholesterol, high blood pressure, cigarette smoking, obesity, lack of exercise, sugar diabetes ISCHEMIA- lack of blood supply to a restricted area INFARCTION- if this restriction results in destroying tissues of the heart - one of the many causes of heart attack FIBRILATION- most common of all serious heart irregularities - atria are never completely emptied of blood and their walls quiver instead of contracting - beat may be very rapid, irregular, and disorganized - AV node is activated at irregular intervals, resulting in a ventricular irregularity TACHYCARDIA- rapid heartbeat - if fibrillation occurs in the ventricles, little or no blood is pumped out of the heart through the pulmonary artery or aorta, and circulation of blood stops> FATAL HEART MURMURS AND VALVE DEFECTS Defective or diseased valves cause most murmurs STENOSIS- valve becomes narrow and blood that forces through becomes turbulent - produces a sound If a valve does not close properly, blood leaks through it in the wrong direction, again producing a sound ATRIAL SEPTAL DEFECT- occurs when the fetal foramen ovale fails to close completely after birth - pressure is lower in right atrium than in left and blood moves from the left to the right atrium - this causes added strain to pulmonary circulation, resulting in fatigue VENTRICULAR SEPTAL DEFECT- if the interventricular septum is defective, deoxygenated blood may mix with oxygenated blood in the left ventricle - affected individual’s blood is not bright red, and skin, fingernails, and lips appear blue> CYANOTIC - can usually be repaired through open heart surgery