* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Visual Deficits Following Acquired Brain Injury
Survey
Document related concepts
Photoreceptor cell wikipedia , lookup
Blast-related ocular trauma wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Idiopathic intracranial hypertension wikipedia , lookup
Retinitis pigmentosa wikipedia , lookup
Mitochondrial optic neuropathies wikipedia , lookup
Transcript
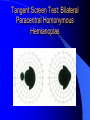
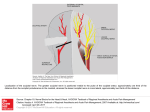
Visual Deficits Following Acquired Brain Injury Bradley K. Farris, M.D. Professor, Ophthalmology Adjunct Professor, Neurology & Neurosurgery University of Oklahoma Dean A. McGee Eye Institute Types of Visual Deficits in ABI Decreased Visual Acuity Decreased Visual Field Diplopia Pain Anatomy of the Visual System Types of Visual Deficits in ABI Decreased Visual Acuity: – Subjective complaints: My vision is blurry My vision is distorted I am blind – I am going blind I lose things in my vision I cannot see well in my right eye My vision comes and goes My eye hurts Types of Visual Deficits in ABI – Causes of Decreased Visual Acuity: Refractive error – Pre-existing or decompensated – Obtaining an accurate visual acuity can be challenging Structural damage to eye – Corneal, lenticular, retinal, optic nerve Traumatic cortical visual loss bilaterally – Anatomical correlation to occipital lobes Papilledema Dry eye syndrome Right Eye Papilledema Optic Atrophy OD Types of Visual Deficits in ABI Decreased Visual Field – Unilateral: Ocular damage to retina, optic nerve – Unilateral, may be altitudinal – Bilateral: Homonymous Hemianopia: – Right vs. Left Bitemporal Hemianopia: – Optic Chiasm contusion (basilar skull fracture) Tunnel Visual Field: – Emotional overlay Anatomy of the Visual System *Diagrams of Visual Field Defects Unilateral defects: – Papilledema, trauma, altitudinal Homonymous Hemianopias: – Right vs. Left – Paracentral Bitemporal Hemianopias: – Basilar skull fractures Quadrantic Defects The “Classic” Homonymous Hemianopia in Occipital Lesions Tangent Screen: Left Inferior Homonymous Quadranopia Tangent Screen Test Right Occipital Tip Infarct Tangent Screen Test: Bilateral Paracentral Homonymous Hemianopias Bilateral Occipital Tip Infarcts: “Watershed” Types of Visual Deficits in ABI Diplopia – Monocular: Not eliminated closing one eye Refractive, cataract, dry eyes – Binocular: Eliminated closing one eye Restrictive: – Orbital or facial fractures (entrapment) Paretic: – Cranial nerve palsies Types of Visual Deficits in ABI Diplopia – Restrictive: Enophthalmous, “restricted” movement – Paretic: Third Cranial Nerve palsy – Dilated pupil, ptosis, vertical + horizontal Fourth Cranial Nerve palsy – Vertical diplopia worse to one side Sixth Cranial Nerve Palsy – Horizontal diplopia worse to one side Goals of surgery -Single vision in primary -Single vision at near -Downgaze more crucial than upgaze -Improve torticollis -Increase field of SBV -Achieve good cosmesis Types of Visual Deficits in ABI Ocular Pain: – Post-traumatic Trigeminal Neuralgia: Throbbing, sharp/shooting, “tooth-ache of the eye” Radiates from behind the eye to ipsilateral ear – Migraine Headache: Post-traumatic Exacerbation of pre-existing condition Muscle contraction overlay Types of Visual Deficits in ABI Emotional Overlay: – The effects of stress, anxiety , and depression on the nervous system and body: Which affects the character and pattern of complaints, Which affects the examination and treatment plan, Which affects the approach to the patient, Which affects the patient expectations, Which affects the rehabilitative success Important Points Traumatic visual loss is not progressive There is a reason for blurred vision You don’t have to live with diplopia Visual field defects may improve Neurological patients require time and patience There is not one patient that cannot be helped – “Seldom heal, comfort always” Treatment Options Glasses for refractive errors/bifocals Diplopia treatment: – – – – Wait 6 months (force fusion) Patch therapy (no need to alternate) Prismatic glasses Strabismus surgery (realistic expectations) Spend time with the patient: – Address physical, emotional, and spiritual needs ML #317185 53 YO WF CC: Visual loss OU HPI: Plane crash 4 mos ago – Depressed skull fx – Multiple reconst surg, R orbit PMH: Otherwise nl EXAM: 2/700 OD, 20/30 OS – – – – Dense bitemp vf defect 3mm enophth OD Complete ext ophth OD ON pallor OU KM #316707 41 YO F CC: Headaches/blurred vision PMH: Negative EXAM: 20/20 OU – + L-N dissociation – + svp’s, vf’s bilat arcuates, OS>OD QUESTIONS? Case Presentations? Complex patient issues? Ethical dilemmas?