* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Chapter 23
Survey
Document related concepts
Biochemistry wikipedia , lookup
Photosynthesis wikipedia , lookup
Homeostasis wikipedia , lookup
Human genetic resistance to malaria wikipedia , lookup
Evolution of metal ions in biological systems wikipedia , lookup
Gaseous signaling molecules wikipedia , lookup
Transcript
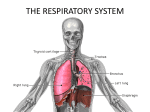
Chapter 23 Respiratory System Respiration • Ventilation: Movement of air into and out of lungs • External respiration: Gas exchange between air in lungs and blood • Transport of oxygen and carbon dioxide in the blood • Internal respiration: Gas exchange between the blood and tissues The primary function of respiration is to deliver oxygen to the tissues and bring back the a metabolic product, carbon dioxide, to the lungs for exchange with oxygen. The ratio, CO2/O2, depends upon what kinds of foods are consumed as the energy source, and is called the respiratory quotient (RQ). On a mixed diet the RQ is about 0.8. For carbohydrate 1.0, for fat 0.7 and for protein 0.8. Respiratory System Functions • Gas exchange: Oxygen enters blood and carbon dioxide leaves • Regulation of blood pH: Altered by changing blood carbon dioxide levels • Voice production: Movement of air past vocal folds makes sound and speech • Olfaction: Smell occurs when airborne molecules drawn into nasal cavity • Protection: Against microorganisms by preventing entry and removing them 1. Pulmonary ventilation The purpose of pulmonary ventilation is to exchange gases in the alveoli. One single respiratory cycle consists of inspiration and expiration. Fig 23-16 Pressure change during respiration a. Pressure and airflow to the lungs Size of the thoracic cavities, where the lungs are held, is determined by the position of the ribs and abdominal diaphragm. The outer membrane of the lungs, visceral pleura, adheres to parietal pleura with pleural fluid. These membranes are kept in contact with the fluid while the lungs expand and shrink. (Fig. 23-16). The flows of air into the lungs and out from the lungs are determined by changing the volume of thoracic cavity, thus creating negative and positive pressures in the lungs relative to the outside pressure. In order to keep the lungs in contact with the thoracic wall, the fluid in the pleural cavity must be maintain closed. a. Modes of breathing Inhalation, while quiet breathing, involves contractions of the diaphragm and the external intercostals. Exhalation is passive. In forced breathing both inhalation and exhalation are active. a. Respiration volumes and rates The tidal volume is the amount of air moved into or out of the lungs during on respiratory cycle. During quiet breathing only a small fraction of the air in the lungs is exchanged. - about 500 ml. The total lung capacity may be divided into 4 major fractions. Fig. 23-18. Fig 23-18 Respiratory volumes and capacities 1. The tidal volume. Volume of air inspired or expired during a normal inspiration or expiration - about 500 ml. 2. Inspiratory reserve volume (IRV). The amount of air that can be taken in over and above the tidal volume - males 3,300 ml and females 1,900 ml. 3. Expiratory reserve volume (ERV). The amount of air that could be voluntarily expelled at the end of a tidal cycle - about 1,100 ml. 4. ml. Residual volume - After the expiratory volume - about 1,200 By combining more than two of these volumes, pulmonary capacities are formed. 1. Gas exchange at the respiratory membrane Diffusive exchange of gases takes place through respiratory membranes. a. Alveolar ducts and alveoli Study Fig. 23-10 for alveolar ducts, alveolar sacs, and alveoli. The surface area of alveolar and alveoli, where gas exchanges takes, is large and amounts up to 140 sq ft. The alveolar epithelium consists of thin squamous cells. Fig. 2312. Alveolar macrophages move around on the surface of the epithelium to combat diseases. Surfactant is released from the surfactant cells, which are imbedded with the epithelium. Surfactant reduces the surface tension of the epithelial cells and keep alveoli inflated. Without the surfactant the alveoli will collapse. Furthermore, without surfactant, a smaller alveoli joined to a larger alveoli will collapse and join the larger alveoli. Fig 23-12 Alveolar organization a. The respiratory membrane Exchange of gases is done from the side of higher content to that of the lower content of each gas through the respiratory membranes, which consist of three layers. (Fig. 23-12b,c). 1. The squamous epithelial cells 2. The endothelial cells of capillaries 3. The fused basement membranes between them. The total thickness is about 0.1 um. Thus, lipid soluble oxygen and carbon dioxide pass through the membrane quickly. Although the passage of blood going through alveolus capillaries is fast, it is assumed that the gases in the blood coming out from the alveolus capillaries are in equilibrium with those in the alveoli. Pneumonia by Pneumocystis carinii commonly found in alveoli. a. Mixed gases and partial pressures Composition of normal air is: 20.8% 78.6% 0.5% 0.04% Trace Oxygen Nitrogen Water (This could change) Carbon dioxide Helium, hydrogen, etc. The total pressure at sea level is 760 mmHg. The gravitational pull of all the gases in the atmosphere down at the sea level amounts this much. Since 20.8% of the air is oxygen, the contribution by oxygen as its partial pressure is, 20.8 X 760 = 158.08 mmHg (or torr) Thus, the partial pressure of oxygen, PO2, is 158.08 mmHg. The partial pressures for other gasses may be calculated in a similar manner. Also, the sum of all partial pressures will be 760 mmHg. If there is moisture in the air, the percentage of other gases will be decreased by the amount of pressure by water vapor, but the total pressure will not change. Thus, if the partial pressure of water is 40 torr, the total pressure of the rest of gases will have pressure of only 720 torr (760 - 40 = 40). a. Alveolar versus atmospheric air As the air gets into the respiratory system, the composition of gases will change. The air will get warmer and moist. More carbon dioxide content will increase. See Fig. 23-20 for the level of gases in different parts of the respiratory system. Fig. 23-20 Gas exchange Partial pressures within the circulatory system Study Fig. 23-20 for the partial pressures of oxygen and carbon dioxide in the circulatory system of a resting human. Gas pick up and delivery Solubility of both oxygen and carbon dioxide are relatively small in plasma. However, the total contents of these two gases in plasma are significantly increased physiologically. Changes in Partial Pressures PARTIAL PRESSURE OF GASES Gas Air Alveolar N2 597 569 O2 159 104 H2O 3.7 47 CO2 0.3 40 Tissue, Art. 95 47 40 Tissue, Vein 40 47 45 1. Oxygen transport 98.5% of oxygen in arterial blood are bound to hemoglobin and only 1.5% are in the form of dissolved oxygen. Hemoglobin binds oxygen reversibly up to 4 molecules of oxygen. Hb + 4O2 = Hb(O2)4 Oxygen-RBC Dissociation Curve at Rest Oxygen-RBC Dissociation Curve during Exercise Shifting the Curve Since the partial pressure of oxygen in interstitial fluid is about 40 torr, at this pressure, the red blood cells are about 75% oxygen saturated - thus 25% of oxygen in the red blood cells are unloaded. The amounts of unloaded oxygen may increase in response to the increased tissue oxygen demand - i. e. more carbon dioxide. At rest, about 5 ml of oxygen is transported to the tissues in each 100 ml of blood at cardiac output of 5000 ml/min, thus 250 ml of oxygen per minute. Under exercise, this may be increased up to 15 times. Hemoglobin and RBC What makes the difference in oxygen affinity between hemoglobin in solution and in red blood cells? The oxygen dissociation curves of hemoglobin in solution and that in cells are compared below. 100% Hb DPG RBC Saturation 0% 40 mmHg 100 mmHg The oxygen dissociation curve of purified hemoglobin is shifted towards left of that of red blood cells. Since Hb in solution saturates with oxygen at the lower partial pressure of oxygen than that of red blood cells, Hb has a higher affinity to oxygen than RBC. The difference comes from the presence of 2,3 diphosphoglycerate, that interacts with Hb, in red blood cells. In fact, the level of 2,3-DPG regulates the oxygen affinity of red blood cells. In the higher altitude, its level goes up so that red blood cells can pick up oxygen more. 1. Carbon dioxide transport Carbon dioxide is a waste product of aerobic metabolism. It may exist in blood in three forms. 1. As freely dissolved gas in plasma. 7% 2. Bound to the amino group of hemoglobin and forms carbamino hemoglobin. It does not bind to the heme where oxygen binds. 23% The oxygen affinity of hemoglobin is slightly reduced, thus CO2 bound hemoglobin releases more oxygen. Other proteins can form carboamino-proteins, but the amount is small. 3. CO2 enters RBC where carbonic anhydrase (CA) facilitates reaction of CO2 with water to form carbonic acid. Carbonic acid dissociates further to bicarbonate and proton. 70% CA CO2 + H2O === H2CO3 ===== H+ + HCO3- The released proton is likely to be picked up by hemoglobin and the molecule reduces its oxygen affinity further, thus releases more oxygen. Bicarbonate ions made in RBC will leave the cell in exchange with chloride ion (chloride shift). The reverse reactions of 2 and 3 take place in the alveolar capillaries to restore oxygen. Study Fig. 23-24 for pick up and release of carbon dioxide by RBC. Outside RBC, CO2 may undergo similar reaction with CA on the surface of capillary cell walls. In this case, the released proton remains in blood plasma, thus blood pH goes down. Without much ventilation (hyhpoventilation) blood pH goes down. While by hyperventilation, blood pH goes up. Fig. 23-25 Summary of gas transport 1. Control of respiration a. The respiratory centers of the brain The respiratory center has three pairs of nuclei in the reticular formation of the pons and medulla oblongata. They regulate the respiratory muscles and control the respiratory rate and the depth of breathing. (Fig. 23.27) The respiratory rhythmicity center determines the basic pace. Fig. 23-27 Respiratory centers and reflex Modification of Ventilation • Chemical control • Cerebral and limbic system – Respiration can be voluntarily controlled and modified by emotions – Carbon dioxide is major regulator • Increase or decrease in pH can stimulate chemosensitive area, causing a greater rate and depth of respiration – Oxygen levels in blood affect respiration when a 50% or greater decrease from normal levels exists Modifying Respiration