* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Orthopedic Solutions
Survey
Document related concepts
Transcript
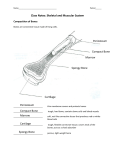
® Cymatherapy Orthopedic Solutions Sound Advice In Sports Medicine Harness the energy of sound to enhance healing in orthopedics and sports medicine ~CYMATHERAPY FOR A KINDER ANSWER~ Copyright 2007 Elizabeth Bauer for Cymatherapy International. All Rights Reserved. Cymatherapy ® Orthopedic Solutions: Sound Advice in Sports Medicine Before Cymatherapy® 15º Extension Contracture After Cymatherapy® 5º Full Extension Images above: right knee extension contracture (of 15 years) resolved in one session using Cymatherapy®. Skin discoloration due to Neurovascular Injury Ankle Swelling Skin discoloration of Neurovascular Injury Resolving Ankle Swelling resolved Images above: right ankle fusion (of 15 years) with neurovascular injury, vascular discoloration, chronic pain and swelling, due to a comminuted fracture, resolving within 3 sessions using Cymatherapy®. 1 What is Cymatherapy®? Cymatherapy® is a non-invasive, sound therapy ( acoustic energy) that helps restore the body to optimal health, balance and function. It uses advanced instruments to transmit frequencies to the body’s organs and tissues that are associated with healthy cells and healthy cell function, supporting the body’s natural healing abilities. How does Cymatherapy® and the Cyma® 1000 work? Today, scientists have shown that the human body is a dynamic energy system and that our cells, organs and tissues have their own vibratory or resonant nature. This natural, or resonant, frequency can become upset or imbalanced, leading to pain, illness or disease. The new Cyma® 1000 is the culmination of over 50 years of research and development. Cymatherapy® International has developed a unique and internationally patented delivery system. The Cyma® 1000 uses a unique applicator to deliver precise combinations of frequencies associated with healthy tissues and organ systems. These sound waves help to normalize and synchronize the cells’ frequency back to its natural healthy state of vibrational resonance. If you have muscular discomfort, for example, the energy of that muscle and the frequency of its field will have been changed by the injury or condition affecting it. Cymatherapy® transmits corrective frequencies into the muscle to rebalance its energy and stimulate the body’s natural healing process. A breakthrough in sound therapy, the Cyma® 1000 is programmed with some 700 “commutations” (harmonious combinations of five frequencies) to treat a variety of imbalances in the body. The Cyma® 1000, via its patent-pending applicator, also contains a static magnet in the diaphragm of its applicator head. This innovation provides a combined magnetic field and a sound wave that oscillate at the same frequency, simultaneously. Many well constructed medical studies in Europe, Asia and the United States have proven that oscillating magnetic fields are effective in alleviating many physical problems. The combination of sound and magnetic therapy―two powerful and natural healing agents in the field of bioresonance and vibrational medicine―further enhance results when combined. How is Cymatherapy® administered? A certified Cymatherapy® practitioner selects the programs for the Cyma® 1000 to deliver the exact combination of frequencies to be used. The applicator of the Cyma® 1000 is placed on the surface of the skin. Cymatherapy® administered by a qualified practitioner is safe, irrespective of the client’s age or level of fitness. Glossary of Terms: Arthrofibrosis- 'Arthro' means joint and 'fibrosis' means scarring. Arthrofibrosis is the internal scarring of the joint, with consequent stiffness, loss of range of motion that results in disability. This condition is generally a sequel to internal joint bleeding or surgery, where rehabilitation has been inadequate or inappropriate. Arthrofibrosis begins with adhesions, and in the early stages these can often be broken with appropriate physiotherapy or manipulation under anesthesia. Later, the adhesions thicken and contract, flexibility is lost leading to extension or flexion contractures. 2 Cartilage- a type of dense connective tissue. It is composed of cells called chondrocytes which are dispersed in a firm gel-like ground substance, called the matrix. Cartilage is avascular (contains no blood vessels) and nutrients are diffused through the matrix. Cartilage is found in the joints, the rib cage, the ear, the nose, in the throat and between intervertebral disks. The main purpose of cartilage is to provide a framework upon which bone deposition could begin. Another important purpose of cartilage is to provide smooth surfaces for the movement of articulating bones. There are three main types of cartilage: ♦ Hyaline cartilage- the most abundant type of cartilage. The name hyaline is derived from the Greek word hyalos, meaning glass. This refers to the translucent matrix . Hyaline cartilage is found lining bones in joints (articular cartilage.) It is also present inside bones, serving as a center of ossification or bone growth ♦ Elastic cartilage- (yellow cartilage) is found in the pinna of the ear and several tubes, such as the walls of the auditory and eustachian canals and larynx. Cartilage is present to keep the tubes permanently open. Elastic cartilage is similar to hyaline cartilage but contains elastic bundles (elastin) scattered throughout the matrix. This provides a tissue which is stiff yet elastic ♦ Fibrocartilage- (white cartilage) is a specialised type of cartilage found in areas requiring tough support or great tensile strength, such as between intervertebral disks, the pubic and other symphyses, and at sites connecting tendons or ligaments to bones. There is rarely any clear line of demarcation between fibrocartilage and the neighboring hyaline cartilage or connective tissue. The fibrocartilage found in intervertebral disks contains more collagen compared to hyaline. Fibrocartilage lacks a perichondrium Chondromalacia- fraying and damage to the underlying patellar cartilage (the cartilage under the knee cap.) Connective tissue- any type of biological tissue with an extensive extracellular matrix that often serves to support, bind together, and protect organs. Types of connective tissue: Figure: Chondromalacia. ♦ Bone- contains specialized cells called osteocytes embedded in a mineralized extracellular matrix, and functions for general support. Bone is mineralized connective tissue that contains collagen and calcium phosphate, a mineral crystal. Calcium phosphate gives bone its firmness ♦ Blood- is considered to be a type of connective tissue. Even though it has a Figure: blood cells. 3 ♦ ♦ ♦ ♦ ♦ ♦ different function in comparison to other connective tissues, it does have an extracellular matrix. Blood functions in transport. Its extracellular matrix is blood plasma, which transports dissolved nutrients, hormones, and carbon dioxide in the form of bicarbonate. The main cellular component is the red blood cell. The matrix is the plasma and erythrocytes, leukocytes and platelets are suspended in the plasma Cartilage- provides cushioning. The extracellular matrix of cartilage is composed primarily of collagen; a form of fibrous connective tissue that is composed of closely packed collagenous fibers in a rubbery gelatinous substance called chondrin. The skeletons of sharks and human embryos are composed of cartilage. Cartilage also provides flexible support for certain structures in adult humans including the nose, trachea and ears. Connective tissue proper- dense connective tissue or fibrous connective tissue that forms ligaments and tendons. Its densely packed collagen fibers have great tensile strength Loose connective tissue or areolar connective tissue- holds organs in place and attaches epithelial tissue to other underlying tissues, and has a variety of proteinaceous fibers, including collagen and elastin Reticular connective tissue- a network of reticular fibers (fine collagen) that form a soft skeleton to support the lymphoid organs (lymph nodes, bone marrow, and spleen) that joins connective tissues to other tissues. Adipose tissue- contains adipocytes, used for cushioning, thermal insulation, lubrication (primarily in the pericardium) and energy storage Elastic fibers- are made of elastin and are "stretchable" Effusion- excessive joint fluid inside the joint that usually comes on suddenly after an injury or overuse of a joint. An acute effusion may also occur in an arthritic or gouty joint. A joint filled with blood, rather than joint fluid is usually called a haemarthrosis. A chronic effusion is one which is there all the time, although sometimes it may be worse than at other times. Fracture- a bone break. Fractures may be described by the extent to which the bone has been broken: ♦ Incomplete or 'greenstick'- not fully broken through but with a pattern resembling the outer splintering of a green stick when it is bent. Usually found in children ♦ Complete-broken cleanly into two pieces ♦ Multiple- broken into more than two pieces ♦ Comminuted- shattered into several bits 4 ♦ Transverse- oblique or spiral In addition a fracture may be: ♦ Simple or closed - where no fragment has penetrated the skin ♦ Open or compound - where the skin has been pierced by a bone fragment, even if the bone has returned under the skin Frozen shoulder- (adhesive capsulitis) is a disorder characterized by pain and loss of motion or stiffness in the shoulder. It affects about two percent of the general population. It is more common in women between the ages of 40 years to 70 years old. The causes of frozen shoulder are not fully understood. The process involves thickening and contracture of the capsule surrounding the shoulder joint. A doctor can diagnose frozen shoulder based on the history of the patient's symptoms and physical examination. X-rays or MRI (magnetic resonance imaging) studies are sometimes used to rule out other causes of shoulder stiffness and pain. Pain due to frozen shoulder is usually dull or aching. It can be worsened with attempted motion. The pain is usually located over the outer shoulder area and sometimes the upper arm. The hallmark of the disorder is restricted motion or stiffness in the shoulder. The affected individual cannot move the shoulder normally. Motion is also limited when someone else attempts to move the shoulder for the client. Functional ability- physical, mental, or social ability to carry on the normal activities of life. Joint dynamics- dynamic joint control during activity involving complex functional range of motion (flexion/extension, abduction/adduction, and internal/external rotation), synovial fluid viscosity, force distribution, dynamic load bearing and limb inertia. The topic of joint dynamics is very scarce in the literature especially for actively functioning joints involving multiple axes in multiple angles with the subject maintaining various levels of muscle contraction. Ligament- a short band of tough fibrous connective tissue composed mainly of long, stringy collagen fibers. Ligaments connect bones to other bones to form a joint. Ligaments are slightly elastic; when under tension, they gradually lengthen. ♦ Capsular ligaments are part of the articular capsule that surrounds synovial joints. They act as mechanical reinforcements ♦ Extra-capsular ligaments join bones together and provide joint stability The consequence of a torn ligament can be the instability of a joint. The instability of a joint over time may lead to the wear of cartilage and osteoarthritis. The ligaments of the knee: Anterior cruciate ligament (ACL) Lateral collateral ligament (LCL) Posterior cruciate ligament (PCL) Medial collateral ligament (MCL) 5 Muscle atrophy- muscle wasting. The wasting or loss of muscle tissue resulting from disease, injury or lack of use. Muscle hypertrophy- an increase in mass or girth of a muscle. Muscle hypertrophy can be induced by a number of stimuli. The most familiar of these is exercise. The first measurable effect of hypertrophy is an increase in the neural drive through the stimulation of the mechanoreceptors that stimulate a muscle contraction. Neuralgia- a sharp, shooting pain along a nerve pathway. Severe nerve pain caused by nerve compression or the breakdown of the protective myelin sheath surrounding a nerve. Neuritis- Inflammation of a nerve accompanied by pain and sometimes loss of function. The pain or tingling from damaged or inflamed peripheral nerves (nerves not in the brain or spiral cord) may become severe and disabling. Patella- or kneecap is a thick, triangular bone which articulates with the femur and covers and protects the front of the knee joint. It is a sesamoid bone which develops from the tendon of the quadriceps femoris muscle, which contracts to straighten the leg. The patella increases the leverage that the tendon can exert on the femur by increasing the angle at which it acts. The vastus intermedialis muscle is attached to the base of patella. The vastus lateralis and vastus medialis are attached to lateral and medial borders of patella respectively. The patella ossifies around the ages of 3 to 5. Patellofemoral Syndrome- patellofemoral (PF) pain syndrome can be defined as retropatellar or peripatellar pain resulting from physical and biochemical changes in the PF joint characterized by anterior knee pain that typically occurs with activity and often worsens when descending steps or hills. It can also be triggered by prolonged sitting. One or both knees can be affected. The etiology of PF pain syndrome may be multifactoral. Causes include overuse/overload, biomechanical problems and muscular dysfunction. Figure: Dynamic stabilizers (suspension system) of the patella. The most frequent cause of anterior knee pain is retinacular stress associated with PF alignment. Biopsies of the lateral retinaculum have shown that small nerves in the retinaculum can sustain injury causing neuroma (Fulkerson JP, 6 Tenant R, Javin JS, et al: Histological evidence of retinacular nerve injury associated with patellofemoral malalignment. Clin Orthop 1985;197:196-205.) Proprioception- is the sense of the position of parts of the body; relative to other neighboring parts of the body in three dimensional time and space. Proprioception is a sense that provides feedback solely on the status of body position internally. It is the sense that indicates whether your body is moving with required effort, as well as where the various parts of the body are located in relation to each other. Kinesthesia is another term that is often used interchangeably with proprioception. Some users differentiate the kinesthetic sense from proprioception by excluding the sense of equilibrium or balance from kinesthesia. The proprioceptive sense is believed to be composed of information from sensory neurons located in the inner ear (motion and orientation) and in the stretch receptors of joints and muscles. There are specific nerve receptors for this form of perception called mechanoreceptors. Range of motion- joint flexibility is defined as the range of motion (ROM) allowed at a joint. A joint's ROM is usually measured by the number of degrees from the starting position of a segment to its position at the end of its full range of the movement. The most common way this is done is by using a double-armed goniometer. A stationary arm holding a protractor is placed parallel with a stationary body segment and a movable arm moves along a moveable body segment. The pin (axis of goniometer) is placed over the joint. (Measurement of joint motion: a guide to goniometry/Cynthia Claire Norkin, D. Joyce White―2nd ed. ISBN: 0-8036-6579-2) Retinaculum- a band or bandlike structure that holds an organ or a joint in place. Soft tissue- tissues that connect, support, or surround other structures and organs of the body. Soft tissue includes muscles, tendons, fibrous tissues, fat, blood vessels, nerves, and synovial tissues. Sprain- an injury involving the stretching or tearing of a ligament (tissue that connects bone to bone) or a joint capsule, which help provide joint stability. A severely damaged ligament or joint capsule can cause instability in a joint. Symptoms may include pain, inflammation, and in some cases, the inability to move a limb (arm, leg, foot). Sprains occur when a joint is forced beyond its normal range of motion, such as turning or rolling your ankle. Severity of sprain and strains ♦ Grade I- (mild) sprain or strain involves some stretching or minor tearing of a ligament or muscle ♦ Grade II- (moderate) sprain or strain is a ligament or muscle that is partially torn but still intact ♦ Grade III- (severe) sprain or strain means that the ligament or muscle is completely torn, resulting in joint instability 7 Images: severity grading of strain or sprain of the ankle. Strain- injuries that involve the stretching or tearing of a musculo-tendinous (muscle and tendon) structure. An acute (instant or recent) strain of the musculo-tendinous structure occurs at the junction where the muscle is becoming a tendon. These strains take place when a muscle is stretched and suddenly contracts, as with running or jumping. This type of injury is frequently seen in runners who strain their hamstrings. Many times the injury will occur suddenly while the runner is in full stride. Symptoms for an acute muscle strain may include pain, muscle spasm, loss of strength, and limited range of motion. Chronic (long-lasting) strains are injuries that gradually build up from overuse or repetitive stress resulting in tendinitis (inflammation of a tendon). For example, a tennis player may get tendinitis in his or her shoulder as the result of constant stress from repeated serves. Tendonitis- inflammation of the tendon. Tendons may become inflamed by an imbalanced muscle load pulling against the resistance of the tendon causing an irritation. If the normal smooth gliding motion of your tendon is impaired, the tendon will become inflamed and movement will become painful. A tendon is a tough yet flexible band of fibrous tissue that connects the muscles to the bones. When a muscle contracts it pulls on a bone causing movement. The structure that transmits the force or energy of the muscle contraction to the bone is called a tendon. 8