* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download PowerPoint Presentation - Infectious Diseases of the Respiratory
African trypanosomiasis wikipedia , lookup
Swine influenza wikipedia , lookup
Hepatitis C wikipedia , lookup
Oesophagostomum wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
West Nile fever wikipedia , lookup
Orthohantavirus wikipedia , lookup
Schistosomiasis wikipedia , lookup
Leptospirosis wikipedia , lookup
Neonatal infection wikipedia , lookup
Herpes simplex virus wikipedia , lookup
Henipavirus wikipedia , lookup
Marburg virus disease wikipedia , lookup
Antiviral drug wikipedia , lookup
Hepatitis B wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Influenza A virus wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
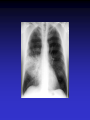
Upper and Lower Respiratory Tract Infections Meral SÖNMEZOĞLU, MD Yeditepe University Hospital Associate Professor of Department of Infectious Diseases and Microbiology Infections of the Respiratory tract • Most common entry point for infections • Upper respiratory tract –nose, nasal cavity, sinuses, mouth, throat • Lower respiratory tract –Trachea, bronchi, bronchioles, and alveoli in the lungs Fig. 21.1a Upper Respiratory Infections • • • • • • Common Cold/ Influenza Pharyngitis, tonsillitis Acute sinusitis Acute laryngitis Acute laryngotracheobronchitis (Croup) Otitis media, otitis externa, mastoitidis 5 Bacterial causes of URIs • Streptococcus pyogenes (group A ßhemolytic) • Group C streptococci • Haemophylus influenza • Moraxella catarrhalis • Staphylococcus aureus • Klebsiella pneumoniae • Haemophylus parainfluenzae • Mycoplasma pneumoniae • Chlamydia pneumoniae Viral causes of URIs • • • • • • • • • • Rhinovirus (100 types and 1 subtype) Coronavirus (>3 types) Parainfluenza virus Respiratory syncytial virus İnfluenza virus Adenovirus (type 3,4,7,14,21) Coxsackievirus A (type 2,4-6,8,10) Epstein Barr virus Cytomegalovirus HIV-1 Clinical characteristics of “common cold” • Incubation period 12-72 hrs • Cardinal symptoms: – Nasal discharges – Nasal obstuctions – Sneezing – Sore and scratchy throat – Cough • Slight fever • Duration 1 week, self limited Diagnosis • Typical and easy • Differential diagnosis; • -hay fever • -vasomotor rhinitis • Major challenge is to distinguish the uncomplicated cold from secondary bacterial sinusitis and otitismedia Treatment • First generation antihistaminics • Nonsteroidal anti-inflammatory drugs • Sore throat reliefs with warm saline gargles and topical anesthetics • Oseltamivir? Prevention • Isolation of the patients for first days • Influenza vaccines Respiratory Syncytial Virus • Enveloped (membrane) RNA virus • Spread by respiratory droplets • Community outbreaks in late fall to spring • Upper respiratory tract infection – epithelial cells • May be fatal in infants Influenza Virus An enveloped RNA virus Structure Influenza Virus New human strains every year • Mutations Pandemic strains Genetic Recombinant Viruses •1957 Asian Flu H2N2 •1968 Hong Kong Flu H3N2 •1977 Russian Flu H1N1 Bird Flu Directly from birds •?? H5N1 ‘H’ and ‘N’ Flu Glycoproteins H – Hemagglutinin • Specific parts bind to host cells of the respiratory mucosa • Different parts are recognized by the host antibodies • Subject to changes N - Neuraminidase • Breaks down protective mucous coating • Assist in viral release Influenza • Epidemics and pandemics, mostly in winter • Upper respiratory tract infection – epithelial cells • Multivalent killed virus vaccine with strains from the previous year (Grown in embryonated eggs) • Bird flu (H5N1) pandemic in birds Pathogenesis of Influenza • Influenza can be transmitted through small or large particle • aerosols or through contact with contaminated surfaces • If not neutralized by mucosal antibodies, virus attacks respiratory tract epithelium • Infection of respiratory epithelial cells leads to cellular dysfunction, viral replication, and release of viral progeny • Release of inflammatory mediators contributes to systemic manifestations of disease Bridges CB et al. Clin Infect Dis. 2003;37:1094-101. Heikkinen T et al. Lancet. 2003;361:51-9. Clinical Features of Influenza • Sudden onset of symptoms, persist for 7+ days • Incubation period: 1-4 days, average 2 days • Infectious period of wild type virus: – Adults shed virus typically from 1 day before through 5 days after onset of symptoms – Children shed higher titers for a longer duration than adults ACIP. MMWR. 2004,53(RR06)1-40. Kavet J. Am J Public Health. 1977;67:1063-70. Frank AL et al. J Infect Dis. 1981;144:433-441. Hayden FG et al. JAMA. 1999;282:1240-6. Influenza Manifestations & Complications Frequent Rare Exacerbations of underlying disease Children Adults Sinusitis, bronchitis, bronchiolitis, pneumonia, croup, acute otitis media Encephalopathy, myositis, rhabdomyolysis, myocarditis, pericarditis, Reye syndrome, sepsis-like syndrome Cardiovascular, diabetes, asthma, cystic fibrosis Primary viral pneumonia, secondary bacterial pneumonia, sinusitis, bronchitis Myositis, rhabdomyolysis, myocarditis, pericarditis Cardiovascular, diabetes, asthma, COPD Loughlin J et al. Pharmocoeconomics. 2003;21:273-283. Treanor JJ. Influenza virus. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 5th ed. Philadelphia, PA: Churchill Livingstone; 2000:1823-1849. ACIP. MMWR 2004;53 (RR06):1-40. Patient Groups at Risk for Complications • Increased risk of influenza complications among: – Children <2 years – Children and adolescents receiving long-term aspirin therapy – Children and adults with chronic conditions • Chronic pulmonary, metabolic, or CV disorders • Renal dysfunction • Hemoglobinopathies • Immunosuppression, including HIV infection – Pregnant women – Residents of chronic care facilities – Persons 65 years old ACIP. MMWR. 2004;53(RR06):1-40. Complications Pulmonary: Non-Pulmonary: Primary influenza viral pneumonia Secondary bacterial pneumonia Croup Asthma, COPD,* bronchitis, cystic fibrosis exacerbation Increased severity of influenza in HIV patients * Chronic obstructive pulmonary disease Myositis Cardiac complications Toxic shock syndrome Guillain-Barré syndrome Transverse myelitis Encephalitis Reye syndrome Influenza Diagnostic Testing • Rapid Antigen (EIA) – NP aspirates and swabs only – Detects Influenza A/B nucleoproteins – 1 hour TAT, batched on the hour – Upper and lower respiratory specimens – Detects Influenza A/B, Parainfluenza 1/2/3, Adenovirus and RSV – 24-72 hour TAT • Real-time RT-PCR – – – – Upper and lower respiratory specimens Detects Influenza A matrix gene Influenza B validation in progress 24 hour TAT Increase in Sensitivity • Viral Culture (Shell Vial) Treatment • Rest, liquids, anti-febrile agents (no aspirin for ages 6mths-18yrs) • Be aware of complications and treat appropriately • Oseltamivir for patients at risk Sinusitis — facts and figures Definition: – infection of frontal, ethmoidal or maxillary sinuses Symptoms: – facial pain, headache, nasal discharge, fever Prevalence: – 31.2 million cases per year in the USA – 16 million outpatient visits Complications: – permanent mucosal damage and chronic sinusitis – rarely, optic neuritis, subdural abscess and meningitis Schwartz. Nurse Pract 1994;19:58–63 Etiology of acute sinusitis Streptococci S. aureus 8% Staphylococci 6% M. catarrhalis 7% 1% Anaerobes 7% S. pneumoniae 34% Other bacteria 5% H. influenzae 35% Total percentages greater than 100% because of multiple organisms Willett et al. J Gen Intern Med 1994;9:38–45 Sinusitis • Acute sinusitis ; – into three main syndromes: • acute, • subacute • chronic – In young adults, acute sinusitis is responsible for 4.6% of physician consultations RV in Acute Sinusitis • Sinusitis is an extremely common part of the common cold syndrome • RV has been detected in 50% of adult patients with sinusitis by RT-PCR of maxillary sinus brushings or nasal swabs1 • Frequency of association of RV infection with sinusitis suggests the common cold could be considered a rhinosinusitis2 1. Pitkäranta A et al. J Clin Microbial. 1997;35:1791. 2. Gwaltney JM Jr. Clin Infect Dis. 1996;23:1209. Acute pharyngitis/tonsillitis — facts and figures Definition: – inflammation of the pharynx or tonsils Symptoms: – pharyngeal pain, dysphagia and fever Epidemiology: – 1% physician visits/year – most common childhood bacterial infectiona Complications: – acute rheumatic fever and glomerulonephritisa aStreptococcal pharyngitis Gwaltney. In: Principles and Practices of Infectious Disease 1990;43:493–8 Acute streptococcal pharyngitis /tonsillitis Etiology of pharyngitis Coronavirus (5%) Adenovirus (5%) Rhinovirus (20%) Other bacteria/viruses (7%) S. pyogenes (15–30%) Unknown (40%) Gwaltney. In: Principles and Practices of Infectious Disease 1990;43:493–8 Acute otitis media — facts and figures Definition: – infection of the middle ear leading to accumulation of fluid and inflammation of the tympanic membrane Symptoms: – cough, fever, irritability, earache Epidemiology: – 24.5 million physician visits per year – majority of cases occur in children <2 years – most frequent indication for antimicrobial treatment in children in the USA Complications: – loss of hearing Garau et al. Clin Microbiol Infect 1998;4:51–8 Klein. Clin Infect Dis 1994;19:823–33 Infected Middle Ear (otitis media) Acute otitis media — etiology M. catarrhalis 14% H. influenzae 23% S. pneumoniae 35% Unknown 16% Others 32% S. pyogenes 3% S. aureus 1% 2807 effusions from patients in the USA 1980–1989 Total percentages greater than 100% because of multiple organisms Bluestone et al. Paediatr Infect Dis J 1992;11:7–11 Acute Bronchitis Inflammation of the bronchial respiratory mucosa leading to productive cough. Acute Bronchitis • Etiology: A)Viral B) Bacterial (Bordetella pertussis, Mycoplasma pneumoniae, and Chlamydia pneumoniae) • Diagnosis: Clinical • S/S: Productive cough, rarely fever or tachypnea. Treatment A) Symptomatic B) If cough persists for more than 10 days: Azithro x 5 days OR Clarithro x 7 days PNÖMONİ Pneumonia Bacterial, viral or fungal infection can cause Inflammation of the lung with fluid filled alveoli Aetiology Frequency of causative organisms of community-acquired pneumonia (CAP) in Europe. Welte T et al. Thorax 2012;67:71-79 Treatment setting Frequency of Isolation of Causative Organisms of CAP in Europe by Country Percentage Means of Frequency of Isolation in Each Country Franc e Italy Spain Turkey UK German y S pneumoniae 37.2 11.9 33.7 25.5 42.1 40 Haemophilus influenzae 10.3 5.1 5.3 44.9 12.3 8 Legionella spp. 2.0 4.9 12.9 0 9.1 3.1 Staphylococcus spp. 11.7 6.5 3.2 1.0 2.6 5 Moraxella catarrhalis 3.3 1.0 2.7 12.2 0.8 0 Gram-negative bacilli 16.8 24.3 7.9 4.1 2.6 7 Mycoplasma pneumoniae 0.7 7.0 8.4 0 5.3 5.6 1 2.4 7.2 0 5.9 1.3 Coxiella burnetii 0.2 0.4 6.2 0 0.3 0 Viruses 1.7 11.6 5.9 0 18.6 9 No pathogen identified 35.6 67.3 56.8 40.6 38.4 NR Chlamydophila spp. Protective Mechanisms Normal flora: Commensal organisms • Limited to the upper tract • Mostly Gram positive or anaeorbic • Microbial antagonist (competition) Defense Mechanisms • 80% of cells lining central airways are ciliated, pseudostratified, columnar epithelial cells • Each ciliated cell contains about 200 cilia that beat in coordinated waves about 1000x/minute • So the lower respiratory tract is normally sterile Protective Mechanisms Clearance of particles and organisms from the respiratory tract Cilia and microvilli move particles up to the throat where they are swallowed. Alveolar macrophages migrate and engulf particles and bacteria in the alveoli deep in the lungs. Other Protective Mechanisms • • • • • Nasal hair, nasal turbinates Mucus Involuntary responses (coughing) Secretory IgA Immune cells First cause of death in the United States from infectious disease is: A. Meningitis B. Pneumonia C. Gastroenteritis D. Urinary Tract Infections E. Toe fungus First cause of death in the United States from infectious disease is: A. Meningitis B. Pneumonia C. Gastroenteritis D. Urinary Tract Infections E. Toe fungus Mortality due to infections DM Morens et al. Nature 463, 122-122 (2010) doi:10.1038/nature08554 Pneumonia • Most deadly infectious disease in the U.S. • 6th leading cause of death • Average mortality 14% • $20 billion/year in U.S.1 • Community acquired pneumonia affects ~4 million patients and results in 10 million physician visits, • 1 million hospitalizations, and >50,000 deaths annually File Chest 2004; 125:1888-1901 Pneumonia Pathophysiology • Microbial pathogens enter the lung by: • Aspiration of organisms from oropharynx – More common in patients with impaired level of consciousness: alcoholics, IVDA, seizures, stroke, anesthesia, swallowing disorders, NG tubes, ETT – Gram positive and anaerobes: Strep pneumo, H flu, Mycoplasma, Moraxella, Actinomyces – Gram negatives: • more likely with hospitalization, debility, alcoholism, DM, and advanced age • Source may be stomach which can become colonized with these organisms with use of H2blockers • Inhalation of Infectious Aerosols – Influenza, Legionella, Psittacosis, Histoplasmosis, TB • Hematogenous Dissemination – Staph aureus – Fusobacterium infections of the retropharyngeal tissues: Lemierre’s syndrome • Direct inoculation and Contiguous Spread – Tracheal intubation, stab wounds At the left the alveoli are filled with a neutrophilic exudate that corresponds to the areas of consolidation seen grossly with the bronchopneumonia. This contrasts with the aerated lung on the right of this photomicrograph. Clinical presentation • Pneumonia should be considered in any patient who has newly acquired respiratory symptoms: cough, sputum production, dyspnea, especially if accompanied by fever and abnormal breath sounds and crackles • In elderly or immunocompromised, pneumonia may present with confusion, failure to thrive, worsening of underlying chronic illness, falling Pneumonia Symptoms • “Typical” pneumonia: sudden onset of fever, cough productive of purulent sputum, pleuritic chest pain • “Atypical”: gradual onset, dry cough, prominence of extrapulmonary symptoms: headache, myalgias, fatigue, sore throat, nausea, vomiting • Includes diverse entities and has limited clinical value Pneumonia Diagnosis • Radiography: CXR – confirm the presence and location of the pulmonary infiltrate – assess the extent of the infection – detect pleural involvement, pulmonary cavitation, or lymphadenopathy • May be normal when the patient is unable to mount an inflammatory response (immunocompromised) or • is in the early stage of an infiltrative process (hematogenous S. aureus pneumonia) Pneumonia Diagnosis • Sputum gram stain and culture: • Controversial: no rapid, easily done, accurate, cost-effective method to allow immediate results • Expectorated sputum is frequently contaminated by oropharyngeal flora – Low power magnification to assess squamous epithelial cells – Culture and sensitivity are only accurate if there are <10 epi’s per low power field – Best results if the specimen contains >25 WBCs per LPF • If patient has a productive cough, send sputum for gram stain and culture: could be of use in directing treatment if patient fails to respond to empiric therapy Pneumonia Diagnosis • Blood cultures are positive in 11% of patients with CAP, more commonly in patients with severe illness • Urine antigen assays for L pneumophila serogroup 1 can be done easily and rapidly. Sensitivity 70% Specificity >90% • Assay for pneumococcal urinary antigen : sensitivity 50-80% and specificity 90% • Responsible pathogen is not defined in as many as 50% of patients Pneumonia Diagnosis • Routine laboratory tests: • (CBC, electrolytes, hepatic enzymes) are of little value in determining the etiology of pneumonia, but may have prognostic significance and influence the decision to hospitalization. • Should be considered in patients who may need hospitalization, >65 yr, or with coexisting illness. • All admitted patients should have oxygen saturation assessed by oximetry Pneumonia Diagnosis • Invasive testing: percutaneous transthoracic needle aspiration or bronchoscopy are not routinely recommended. – May be helpful in: • immunocompromised hosts • suspected tuberculosis in the absence of productive cough • non-resolving pneumonia • pneumonia associated with suspected neoplasm or foreign body • suspected Pneumocystis jirovecii (carinii) • Pneumonia • Severity • Index Pneumonia Severity Index PORT Score • • • • • • Age 55-10=45 CHF +10 RR +20 HR 124 +10 BUN +20 pO2 +10 115 Class IV Mortality 9% Site of Treatment • Class I or II: Outpatient treatment • Class III: Potential outpatient or brief inpatient observation • Class IV and V: Inpatient • Physician decision making: medical and psychosocial comorbidities, ability to take po, substance abuse, ability to do ADLs CURB 65 • • • • • Confusion Urea level (>19) Respiratory rate (>30) Blood Pressure SBP< 90 or DBP <60 Age • Excellent indicator for mortality ICU Admission • Minor Criteria – – – – – RR>30/min PaO2/FiO2 <250 Multilobar pneumonia Systolic BP <90 Diastolic BP <60 • Major Criteria – Need for mechanical ventilation – Increase in the size of infiltrates by >50% within 48hrs – Septic shock – Acute renal failure (uop <80ml in 4 h or serum Cr>2.0) Modifying Factors that Increase the Risk of infection with Specific Pathogens • Penicillin-resistant pneumococci – – – – – Age >65 B-lactam therapy within the past 3 months Alcoholism Immune suppressive illness (including tx with corticosteroids) Multiple medical comorbidities: DM, CRI, CHF, CAD, malignancy, chronic liver disease – Exposure to a child in a day care center • Enteric gram negatives – – – – Residence in a nursing home Underlying cardiopulmonary disease Multiple medical comorbidities Recent antibiotic therapy • Pseudomonas aeruginosa – – – – Structural lung disease (bronchiectasis) Corticosteroid therapy (>10mg prednisone/day) Broad spectrum antibiotic therapy for > 7 days in past month Malnutrition Group I: Outpatients No cardiopulmonary disease No modifying factors Organism: Streptococcus pneumonia Mycoplasma pneumonia Chlamydia pneumonia Hemophilus influenzae Miscellaneous Legionella Mycobacterium Fungi Treatment: Advanced generation macrolide(azithromycin or clarithromycin) OR doxycycline Group II: Outpatient, with cardiopulmonary disease, and/or other modifying factors • • • • • • • • • • Organism: Strep pneumonia Mycoplasma Chlamydia Mixed infection Hemophilus influenzae Enteric gram-negatives Viruses Miscellaneous Moraxella, Legionella, anaerobes, TB, fungi • Therapy: B -lactam (oral cefpodoxime, cefuroxime, high-dose amoxicillin, amoxicillin/clavulanate or parenteral ceftriaxone PLUS • Macrolide or doxycycline OR • Antipneumococcal fluoroquinolone Group III: Inpatients • • • • • • • • • • Organism Strep pneumonia Hemophilus influenzae Mycoplasma Chlamydia Mixed infection Enteric gram-negatives Aspiration Virus Miscellaneous • • • • • Therapy: 1. Intravenous B lactam: cefotaxime, ceftriaxone, ampicillin/sulbactam, high-dose amipicillin PLUS Intravenous or oral macrolide or doxycycline OR 2. Antipneumococcal fluoroquinolone ICU Patients • • • • • • • • • Organisms: Strep pneumonia Legionella Hemophilus influenzae Enteric gram-negative bacilli Staphylococcus aureus Mycoplasma Respiratory Viruses Miscellaneous • Therapy: • 1. Intravenous B lactam: cefotaxime, ceftriaxone, ampicillin/sulbactam, high-dose amipicillin • PLUS either • Intravenous or oral macrolide or doxycycline • or • Antipneumococcal fluoroquinolone ICU Patients with Risks for Pseudomonas aeruginosa • 1. Selected iv antipseudomonal B -lactam (cefepime, imipenem, meropenem, piperacillin/tazobactam) • PLUS iv antipseudomonal quinolone • OR • 2. Selected iv antipseudomonal B -lactam PLUS iv aminoglycoside PLUS either iv macrolide or iv nonpseudomonal fluoroquinolone Hospital-Acquired Pneumonia • Enteric aerobic gram negative bacilli • Pseudomonas aeruginosa • Staphylococcus aureus • Oral anaerobes • Antipseudomonal cephalosporin (cefepime, ceftazidime) OR Antipseudomonal carbepenem OR B lactam/B -lactamase inhibitor • PLUS • Antipseudomonal fluoroquinolone OR aminoglycoside • PLUS Vancomycin or Linezolid TUS 2012 • Üç hafta-4 yaş arasındaki çocuklarda, toplum kaynaklı pnömoninin en sık bakteriyal etkeni aşağıdakilerden hangisidir? • A) Mycoplasma pneumoniae • B) Haemophilus influenzae • C) Staphylococcus aureus • D) Streptococcus pneumoniae • E) Chlamydia trachomatis TUS 2012 • Üç hafta-4 yaş arasındaki çocuklarda, toplum kaynaklı pnömoninin en sık bakteriyal etkeni aşağıdakilerden hangisidir? • A) Mycoplasma pneumoniae • B) Haemophilus influenzae • C) Staphylococcus aureus • D) Streptococcus pneumoniae • E) Chlamydia trachomatis TUS 2012 • Okul çağındaki çocuklarda trakeobronşite ve pnömoniye en sık neden olan mikroorganizma aşağıdakilerden hangisidir? • A) Chlamydia pneumoniae B) Bordetella pertussis C) Mycoplasma pneumoniae D) Legionella pneumophila E) Haemophilus influenzae TUS 2012 • Okul çağındaki çocuklarda trakeobronşite ve pnömoniye en sık neden olan mikroorganizma aşağıdakilerden hangisidir? • A) Chlamydia pneumoniae B) Bordetella pertussis C) Mycoplasma pneumoniae D) Legionella pneumophila E) Haemophilus influenzae TUS 2010 • Aşağıdakilerden hangisi akut bronşiyolit tedavisinin ilkelerinden biri değildir? • • • • A) Bronşiyal obstrüksiyonun kaldırılması B) Asiklovir tedavisi C) Hipoksemi ve asidozun düzeltilmesi D) Potansiyel kardiyak komplikasyonların önlenmesi • E) İkincil bakteriyal enfeksiyonların tedavisi TUS 2010 • Aşağıdakilerden hangisi akut bronşiyolit tedavisinin ilkelerinden biri değildir? • • • • A) Bronşiyal obstrüksiyonun kaldırılması B) Asiklovir tedavisi C) Hipoksemi ve asidozun düzeltilmesi D) Potansiyel kardiyak komplikasyonların önlenmesi • E) İkincil bakteriyal enfeksiyonların tedavisi QUESTIONS