* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download chapter 2 - Eastbourne, Hailsham and Seaford CCG
Survey
Document related concepts
Polysubstance dependence wikipedia , lookup
Orphan drug wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Pharmacognosy wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Neuropharmacology wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Psychopharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
National Institute for Health and Care Excellence wikipedia , lookup
Transcript
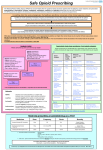
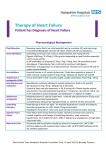
CHAPTER 2 First line drugs – drugs recommended in both primary and secondary care CARDIOVASCULAR SYSTEM Second line drugs – alternatives (often in specific conditions) in both primary and secondary care Specialist drugs – Drugs where a specialist input is needed (see introduction for definition) Specialist only drugs – prescribing within specialist service only Page 2.1 Positive inotropic drugs 2 2.2 Diuretics 2 2.3 Anti-arrhythmic drugs 4 2.4 Beta-adrenoceptor blocking drugs 6 2.5 Drugs affecting the renin-angiotensin system and some other antihypertensive drug 7 2.6 Nitrates, calcium-channel blockers, and potassium channel activators 9 2.7 Sympathomimetics 11 2.8 Anticoagulants and reversal agents 11 2.9 Antiplatelet drugs 15 2.10 Myocardial infarction and fibrinolysis 16 2.11 Antifibrinolytic drugs and haemostatics 16 2.12 Lipid-lowering drugs 17 Date of revision 01/13 03/13 03/13 10/13 01/14 03/14 06/14 07/14 11/14 01/15 04/15 07/15 09/15 11/15 01/16 07/16 08/16 09/16 10/16 12/16 01/17 03/17 First line drugs Revisions 1.3.5 (Updated MHRA Drug Safety), 2.8.2 (Updated guidance), 2.8.1 (Direct Healthcare Professional Communication) 2.6.3 (NICE guidance) 2.8 (NICE guidance) 2.8.2 (MHRA safety update) 2.8.2 (MHRA safety update) 2.4, 2.5, 2.9, 2.12 (NICE guidance) 2.9 (Minor amendment) 2.8.2 (Minor amendment) 2.9 (NICE guidance) 2.4 (NICE guidance), 2.8 (minor amendment) 2.11 (NICE guidance) 2.8 (NICE guidance) 2.8 (NICE guidance) 2.8 (NICE guidance) 2.8 (NICE guidance) 2.8 (NICE guidance) 2.5 (NICE guidance), 2.8 (Drug addition) 2.12 (NICE guidance) 2.6 (NICE guidance) 2.12 (NICE guidance), 2.5 (minor amendment) 2.8 (minor amendment) 2.2 (NICE guidance) 2.9 (Drug deletion), (NICE guidance) Second line drugs Specialist drugs Contributors A Luck G Ells A Luck G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells G Ells Specialist only drugs Page 1 of 20 2.1 Positive inotropic drugs 2.1.1 Cardiac glycosides Digoxin Tablets 62.5 micrograms, 125 micrograms, 250 micrograms Elixir 50 micrograms/ml Injection 100 micrograms in 1ml, 500 micrograms in 2ml Occasionally necessary in hospital to treat Digoxin toxicity Digibind Notes: 1. Digoxin toxicity signs: nausea and vomiting, diarrhoea, visual disturbances, confusion and delirium. 2. Initiation with digoxin therapy requires a loading dose (see BNF). 3. Annual monitoring of urea and electrolytes is important as electrolyte disturbances increase the risk of toxicity from cardiac glycosides (Martindale Edition 32). 4. Serum levels should be assessed 7 – 14 days after adding or removing an interacting drug, and periodically, according to the clinical picture. It is usually only necessary to monitor digoxin levels if there are signs or symptoms present that suggest inadequate dose or drug toxicity. 5. Therapeutic drug monitoring: blood sample to be taken six to eleven hours post dose. Target is 1.0 to 2.60 nanomoles/litre (0.8 to 2.0 micro g/litre). 6. Plasma half-life is 30 to 50 hours. Time to steady state is 7 to 14 days. 2.1.2 Phosphodiesterase inhibitors Milrinone Injection 10mg in 10ml Restricted to ITU only for use in unresponsive heart failure 2.2 Diuretics Please see NICE Clinical Guidelines CG 127 (December 2016) before starting anti-hypertensive medication. Key priorities for implementation relating to drug treatment of hypertension include: Initiating treatment Offer antihypertensive drug treatment to people aged under 80 years with stage 1 hypertension who have one or more of the following: − target organ damage − established cardiovascular disease − renal disease − diabetes − a 10-year cardiovascular risk equivalent to 20% or greater. Offer antihypertensive drug treatment to people of any age with stage 2 hypertension. For people aged under 40 years with stage 1 hypertension and no evidence of target organ damage, cardiovascular disease, renal disease or diabetes, consider seeking specialist evaluation of secondary causes of hypertension and a more detailed assessment of potential target organ damage. This is because 10-year cardiovascular risk assessments can underestimate the lifetime risk of cardiovascular events in these people. Choosing antihypertensive drug treatment Offer people aged 80 years and over the same antihypertensive drug treatment as people aged 55–80 years, taking into account any comorbidities. Step 1 treatment Offer step 1 antihypertensive treatment with a calcium-channel blocker (CCB) to people aged over 55 years and to black people of African or Caribbean family origin of any age. If a CCB is not suitable, for example because of oedema or intolerance, or if there is evidence of heart failure or a high risk of heart failure, offer a thiazide-like diuretic. If a diuretic treatment is to be initiated or changed, offer a thiazide-like diuretic, such as chlortalidone (12.5–25.0 mg once daily) or indapamide (1.5 mg modified-release or 2.5 mg once daily) in preference to a conventional thiazide diuretic such as bendroflumethiazide or hydrochlorothiazide. For people who are already having treatment with bendroflumethiazide or hydrochlorothiazide and whose blood pressure is stable and well controlled, continue treatment with the bendroflumethiazide or hydrochlorothiazide. First line drugs Second line drugs Specialist drugs Specialist only drugs Page 2 of 20 Step 4 treatment For treatment of resistant hypertension at step 4: Consider further diuretic therapy with low-dose spironolactone (25 mg once daily) if the blood potassium level is 4.5 mmol/l or lower. Use particular caution in people with a reduced estimated glomerular filtration rate because they have an increased risk of hyperkalaemia. Consider higher-dose thiazide-like diuretic treatment if the blood potassium level is higher than 4.5 mmol/l. Further detail of this guidance available here The treatment of hypertension during pregnancy is outlined in: NICE CG 107: Hypertension in pregnancy - The management of hypertensive disorders during pregnancy 2.2.1 Thiazide and related diuretics Indapamide Tablets 2.5mg Tablets 1.5mg MR Preferred over conventional thiazides such as bendroflumethazide for hypertension Bendroflumethazide Tablets 2.5mg For resistant oedema / heart failure, under specialist supervision Chlorothiazide Suspension 250mg in 5ml Restricted to paediatrics only. Named patient use only Note: 1. NICE Clinical Guidelines CG 127 no longer recommends conventional thiazides such as bendroflumethazide and hydrochlorthiazide to treat hypertension. Patients whose blood pressure is stable and well controlled can, however, remain on these treatments until a change is clinically warranted. Bendroflumethazide remains on the formulary for these patients and also for use as an. First line drugs Second line drugs Specialist drugs Specialist only drugs Page 3 of 20 2. adjunct to loop diuretics in severe CCF and oliguria. Indapamide 1.5mg MR is reserved for patients with abnormal electrolytes on 2.5mg standard formulation. 2.2.2 Loop diuretics Furosemide Bumetanide Tablets 20mg, 40mg, 500mg Injection 20mg in 2 ml, 50mg in 5ml, 250mg in 25ml Liquid 1mg in 1ml, 40mg in 5ml Tablets 1mg, 5mg Injection 2mg in 4ml 1mg/1ml paediatric use only Notes: 1. Furosemide is the first line choice. 2. Bumetanide may be better absorbed than furosemide in patients with severe CCF. 3. Oral conversion: bumetanide 1mg = furosemide 40mg. 2.2.3 Potassium-sparing diuretics Amiloride Tablets 5mg LiquidSF 5mg in 5ml Spironolactone Tablets 25mg, 50mg, 100mg Suspension (1mg/1ml) 50mg/5ml 1mg/1ml paediatric use only Eplerenone Tablets 25mg Heart failure post MI Notes: 1. Routine co-prescribing of potassium sparing diuretics in combination with thiazide or loop diuretics should be reserved as second line when the patient is stabilised, except in patients where hypokalaemia has been demonstrated or in patients not taking an ACE inhibitor who are at risk from hypokalaemia e.g. those with severe CHD and arrhythmias and those taking digoxin. 2. In severe heart failure, spironolactone added to other treatments in a low dose (e.g. 25mg daily) can reduce mortality and morbidity. Careful monitoring for hyperkalaemia and hypovolaemia is required especially for people taking other diuretics and / or ACE inhibitors. 3. Spironolactone is also included for specific indications e.g. ascites, nephrotic syndrome, primary hyperaldosteronism, hypertension. 4. Eplerenone has outcome data for LVF post MI, but is much more expensive than spironolactone and there is no comparative data for this indication. 2.2.4 Potassium-sparing diuretics with other diuretics Fixed dose combinations of potassium sparing diuretics, for example, co-amilofruse (Frumil®, Frusene®) and coamilozide (Moduretic®) have NOT been considered as necessary in the formulary. 2.2.5 Osmotic diuretics Mannitol Used for cerebral oedema Infusion 20% - 500 ml 2.3 Anti-arrhythmic drugs Amiodarone Atropine Disopyramide First line drugs Tablets 100mg, 200mg Injection 150mg in 3 ml Pre-filled syringe 300mg in 10 ml Pre-filled syringe 1mg/10 ml, 3mg/30ml Injection 600mcg/1ml Capsules 100mg Tablets modified release 250mg Injection 50mg in 5 ml Second line drugs Specialist drugs Oral: Observe loading dose schedule Specialist only drugs Page 4 of 20 Dronedarone Tablets 400mg Multaq® Flecainide Tablets 50mg, 100mg Injection 150mg in 15 ml Mexiletine Propafenone Sotalol Adenosine Capsules 50mg, 200mg Tablets 150mg, 300mg Tablets 40mg, 80mg Injection 6mg in 2ml IV infusion Adenoscan® 30mg in 10ml Lidocaine Infusion 1g in 5% Glucose (500 ml) Injection (pre-filled syringe) 100mg in 5ml Procainamide Injection 100mg in 1ml Note: Amiodarone has a very long half-life (extending to several weeks). Following an oral loading dose (e.g. TDS for 1 week then BD for a further week) maintenance doses are administered ONCE DAILY. Dronedarone has recently been licensed to treat adults with a history of or current non-permanent AF either to prevent recurrence of AF or lower ventricular rate. It has been compared with amiodarone in a clinical trial and found to be less effective than amiodarone but with fewer adverse effects. Dronedarone is considerably more expensive than standard treatments hence it should only be used in accordance with NICE guidance (see below). NICE Guidance: Dronedarone for the treatment of non-permanent atrial fibrillation (Technology Appraisal 197 Aug 2010) Dronedarone is recommended as an option for the maintenance of sinus rhythm after successful cardioversion in people with paroxysmal or persistent atrial fibrillation: whose atrial fibrillation is not controlled by first-line therapy (usually including beta-blockers), that is, as a second-line treatment option and after alternative options have been considered and who have at least 1 of the following cardiovascular risk factors: o hypertension requiring drugs of at least 2 different classes o diabetes mellitus o previous transient ischaemic attack, stroke or systemic embolism o left atrial diameter of 50 mm or greater or o age 70 years or older and who do not have left ventricular systolic dysfunction and who do not have a history of, or current, heart failure. The MHRA Safety Update October 2011 advises that the benefits of using dronedarone now only outweigh the risks in a limited population of patients with paroxysmal or persistent atrial fibrillation. Dronedarone is now contraindicated in patients with: Unstable haemodynamic conditions History of, or current, heart failure or left ventricular systolic dysfunction Liver and lung toxicity related to previous use of amiodarone Permanent AF (ie, duration ≥6 months or unknown, and attempts to restore sinus rhythm no longer considered by physician) The MHRA now recommends regular cardiac, hepatic, renal and pulmonary monitoring (see below) Patients should receive regular cardiac examinations, including an ECG at least every 6 months, to identify those who revert to AF. Discontinuation of dronedarone should be considered for these patients Patients should be carefully evaluated for symptoms of heart failure during treatment Liver-function tests should be done: before starting treatment with dronedarone; after 1 week of treatment; after 1 month of treatment; then every month for 6 months; at month 9; at month 12; and periodically thereafter Plasma creatinine values should be measured before and 7 days after initiation of dronedarone, and renal function should be monitored periodically afterwards. Discontinue treatment in any patients with further elevations of serum creatinine Cases of interstitial lung disease, including pneumonitis and pulmonary fibrosis, have been reported in association with dronedarone. Onset of dyspnoea or non-productive cough may be related to pulmonary toxicity. If pulmonary toxicity is First line drugs Second line drugs Specialist drugs Specialist only drugs Page 5 of 20 suspected during treatment, relevant lung examinations should be considered and treatment discontinued if confirmed. 2.4 Beta-adrenoceptor blocking drugs Beta blockers are no longer recommended as first line treatment for hypertension (see NICE algorithm, page 3). Prescribing for new patients should follow NICE recommendations. Existing patients who are well controlled can be maintained on beta blockers until review needed. Tablets 25mg, 50mg, 100mg Syrup 25mg/5ml Injection 5mg in 10ml Tablets 1.25mg, 2.5mg, 5mg, 7.5mg, 10mg Not for new use first line in hypertension. Remains useful in angina. Labetalol Tablets 100mg, 200mg, 400mg Injection 100mg in 20 ml Hypertension in pregnancy only Propranolol Thyrotoxicosis, migraine and anxiety only Carvedilol Tablets 10mg, 40mg, 80mg and 160 mg Capsules M/R 80mg, 160mg Mixture 50mg in 5ml Injection 1mg in 1ml Tablets 3.125mg, 6.25mg, 12.5mg, Atenolol Bisoprolol Hypertension, angina and on specialist advice in heart failure Heart failure only 25mg Metoprolol Tablets 50mg, 100mg Injection 5mg in 5ml Angina Nebivolol Tablets 5mg Heart failure only for patients aged over 70 years Esmolol Injection 100mg/10 ml, 2.5g/10ml Notes: 1. Propranolol is included for the management of conditions such as thyrotoxicosis, migraine and anxiety only. Standard formulations should be used first line. For patients where compliance might be a problem, the modified release (M/R) formulation may be considered. 2. Labetalol may be used for the treatment of hypertension in pregnancy. 3. Sotalol is listed under anti-arrhythmic drugs as the CSM advises that its use should be limited to the treatment of ventricular arrhythmias or prophylaxis of supraventricular arrhythmias. 4. Acebutolol maybe useful for the small number of patients with palpitations with slow resting heart rate, as it has intrinsic sympathomimetic activity, but this use is unlicensed. Should be used under specialist supervision only. For the treatment of acute heart failure, see NICE CG 187 (October 2014) NICE CG108: Chronic heart failure - Management of chronic heart failure in adults in primary and secondary care (Aug 2010) This guidance outlines the diagnosis and treatment of chronic heart failure. Notes on use of beta blockers in heart failure: 1. Beta-blockers should be considered for patients in controlled heart failure. 2. The NSF states that in people with controlled heart failure beta-blockers started in low doses can reduce mortality when used with other treatments e.g. ACE inhibitors, diuretics and digoxin. 3. An appropriate specialist should initiate beta-blockers used in heart failure. 4. Nebivolol is only for heart failure patients aged over 70 years. The starting dose is 1.25mg for the first two weeks and then if tolerated 2.5mg for two weeks, then 5mg from then on. The following dose regimes are recommended for heart failure: (ref: BNF). First line drugs Second line drugs Specialist drugs Specialist only drugs Page 6 of 20 Bisoprolol Carvedilol Initially 1.25mg once daily (in the morning) for one week. If well tolerated, increase to 2.5mg once daily for one week. Then 3.75mg once daily for one week. Then 5mg once daily for four weeks. Then 7.5mg once daily for four weeks. Then 10mg once daily. Maximum dose is 10mg daily. Initially 3.125mg twice daily (with food). Dose increased at intervals of at least two weeks to 6.25mg twice daily. Then to 12.5mg twice daily. Then to 25mg twice daily. Increase to highest dose tolerated, maximum 25mg twice daily in patients with severe heart failure or less than 85kg body weight and 50mg twice daily in patients over 85kg. Beta blockers are also recommended for secondary prevention post myocardial infarction (see CG172: Secondary prevention in primary and secondary care for patients following a myocardial infarction Nov 2013) 2.5 Drugs affecting the renin-angiotensin system and some other antihypertensive drugs 2.5.1 Vasodilator antihypertensive drugs Hydralazine Tablets 25mg, 50mg Sodium Nitroprusside 50mg vial Note: 1. Hydralazine, when used alone causes tachycardia and fluid retention. 2. In patients who are intolerant of ACE inhibitors or for whom they are contra-indicated, hydralazine may be used in combination with long acting nitrates in moderate to severe chronic congestive cardiac failure, but this combination may be poorly tolerated (BNF). 2.5.2 Centrally acting antihypertensive drugs Methyldopa Tablets 125mg Moxonidine Tablets 200 micrograms and 400 micrograms Injection 150micrograms in 1ml Used as an alternative where other agents have caused side effects (4th line) Notes: Methyldopa is included for the treatment of hypertension in pregnancy only. 2.5.3 Adrenergic neurone blocking drugs Guanethidine Injection 10mg in 1ml Notes: 1. Used for nerve blocks in pain management unit only. 2. No cardiovascular use. 2.5.4 Alpha-adrenoreceptor blocking drugs Doxazosin Phenoxybenzamine Phentolamine Tablets 1mg, 2mg, 4mg Capsule 10mg Injection 10mg in 1ml See BNF chapter 7 for use in BPH Notes: 1. NICE/BHS guidelines suggest doxazosin therapy is additional to other antihypertensive medications. 2. The 4mg modified release formulation of doxazosin is significantly more expensive but does reduce post dose hypotension compared with the standard formulation. 3. In some patients it is safer to use the non-XL formulation bd to avoid this effect. 4. Following conversion from the XL formulation to the standard formulation, it is important to closely monitor blood pressure First line drugs Second line drugs Specialist drugs Specialist only drugs Page 7 of 20 There are two possible strategies to convert patients from modified release to standard doxazosin: In elderly patients, give half the dose of Cardura XL as standard doxazosin, i.e. 4mg XL switched to 2mg standard od. It may then be possible to increase the dose to 2mg bd. In younger patients, give the same dose as Cardura XL divided into a bd regime i.e. 4mg XL to 2mg bd standard. Refer to BNF Chapter 7 for drugs used in the management of benign prostatic hyperplasia. 2.5.5 Drugs affecting the renin-angiotensin system ACE inhibitors are recommended for secondary prevention post myocardial infarction (see CG172: Secondary prevention in primary and secondary care for patients following a myocardial infarction Nov 2013) 2.5.5.1 Angiotensin-converting enzyme (ACE) inhibitors Lisinopril Tablets 2.5mg, 5mg, 10mg, 20mg Ramipril Capsules 1.25mg, 2.5mg, 5mg, 10mg Perindopril Tablets 2mg, 4mg, 8mg See notes below Notes: 1. First doses of ACE inhibitors may cause hypotension especially in patients taking high doses of diuretics, on a low-sodium diet, on dialysis, dehydrated or with heart failure. 2. Renal function and blood pressure should be monitored before and during treatment and the dose reduced in renal impairment. Monitor one week after initiating treatment, one week after a dose increase and otherwise annually. 3. Whereas ramipril and perindopril have dual renal and hepatic excretion, lisinopril is solely renally excreted so more care is needed if the patient has impaired renal function. 4. PROGRESS (Perindopril Protection against Recurrent Stroke Study) BMJ 2005 331:235-236. The benefits of perindopril for the prevention of recurrent stroke are only proven in combination with a thiazide. 5. Perindopril should always be prescribed generically to avoid confusion with the branded product which is a different salt and needs a dose adjustment. 6. Occasionally captopril is useful in hospital for patients in whom initiation of ACE inhibitors proves difficult. 7. If an ACE inhibitor is required in breastfeeding mothers, captopril or enalapril are the agents of choice but should only be prescribed on the advice of a specialist. 2.5.5.2 Angiotensin-II receptor antagonists (ARBs) N.B. Where indicated ACE inhibitors should be tried in all patients before considering an Angiotensin II receptor antagonist Candesartan Irbesartan Losartan Tablets 2mg, 4mg, 8mg, 16mg Outcome data for heart failure Tablets 150mg, 300mg Reno vascular protection, diabetes Tablets 25mg, 50mg, 100mg Hypertension with LVH Valsartan Tablets 40mg, 80mg Sacubitril /valsartan▼ Entresto® tablets 24/26mg, 49/51mg, 97/103mg Post MI when ACE inhibitor not tolerated Notes: 1. No studies have shown that Angiotensin-II receptor antagonists are more effective than ACE inhibitors. They are certainly more expensive. The first-choice renin-angiotensin system drug for people at high risk of CV disease, with or without heart failure, is an ACE inhibitor. 2. Angiotensin-II receptor antagonists should be reserved for those patients on ACE inhibitors who suffer from unacceptable cough, but cough can still occur with ARBs. 3. Candesartan is licensed for heart failure and valsartan post MI. 4. Combining an ACE inhibitor with an angiotensin-II receptor agonist for hypertension is not supported by efficacy or safety data. The ONTARGET study suggests that adding an ARB to an ACE inhibitor in patients at high risk of CV events, who do not also have heart failure, does not prevent adverse CV events. Indeed, using the combination has been shown to increase the risk of adverse effects, serious enough to cause patients to stop treatment. 5. Irbesartan has data for prevention of progression of existing renal disease in type II Diabetes Mellitus. First line drugs Second line drugs Specialist drugs Specialist only drugs Page 8 of 20 6. Losartan has outcome data in diabetic nephropathy and decreased risk of stroke in hypertension with LVH. 7. Monitoring requirements as per ACE inhibitors above. 8. Sacubitril valsartan is a combination neprilysin and angiotensin II receptor inhibitor for the treatment of symptomatic chronic heart failure with reduced ejection fraction. It has been approved by NICE for use in accordance with NICE TA 388: Sacubitril valsartan for treating symptomatic chronic heart failure with reduced ejection fraction (April 2016) NICE has recommended sacubitril valsartan as an option only in people: with New York Heart Association (NYHA) class II to IV symptoms and with a left ventricular ejection fraction of 35% or less and who are already taking a stable dose of angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). Treatment with sacubitril valsartan should be started by a heart failure specialist with access to a multidisciplinary heart failure team. Prescribing may be transferred to primary care after dose titration to the maximum (tolerated) dose and once the patient is on a stable dose. GPs will be informed that a patient has been initiated on sacubitril valsartan via the “Screening Checklist and Notification of Initiation to GP” form. Once the patient is on a stable dose, GPs will be notified and asked to take over prescribing using the “Transfer of Prescribing Responsibility” form. These forms can be found at http://nww.esht.nhs.uk/clinical/cardiology/. 2.5.5.3 Renin inhibitors Aliskiren Tablets 150mg, 300mg Notes: 1. Aliskiren is a direct inhibitor of renin, and targets the same system as ACE inhibitors and ARBs. 2. Data shows it to have similar efficacy to other antihypertensive drugs. 3. It may be used at Step 4 of the NICE/BHS hypertension guidelines (see page 3) where further diuretic, alpha blocker or beta blocker therapy has not been effective or is contraindicated. 2.6 Nitrates, calcium-channel blockers, and potassium channel activators 2.6.1 Nitrates Glyceryl trinitrate Isosorbide mononitrate Spray 400 micrograms Tablets 500 micrograms Patches 5mg/24hours and 10mg/24hours Buccal tablets 2mg, 3mg, 5mg Injection 5mg in 5ml, 50mg in 10ml Tablets 10mg, 20mg, 40mg Modified release tablets (various strengths available) see BNF Notes: 1. NICE CG126: Stable angina: management Offer people optimal drug treatment for the initial management of stable angina. Optimal drug treatment consists of one or two anti-anginal drugs as necessary plus drugs for secondary prevention of cardiovascular disease. 2. Nitrate free periods can be achieved by prescribing ordinary release nitrates twice a day, first thing in the morning and mid afternoon. 3. A modified release preparation (given once a day) may be useful to provide a nitrate free period where a patient requires high doses of isosorbide mononitrate. 4. Modified release TABLETS are more cost effective than capsules therefore when modified release isosorbide mononitrate is prescribed, use tablets, not capsules. 2.6.2 Calcium-channel blockers Amlodipine Adizem XL® or Tildiem LA® Tablets 5mg, 10mg Once a day diltiazem longer acting preparations First line drugs Second line drugs Specialist drugs Specialist only drugs Page 9 of 20 Adizem SR ® or Tildiem Retard ® Diltiazem Twice a day diltiazem longer acting preparations Modified release tablets 60mg administered twice or three times daily Verapamil Tablets 40mg, 80mg, 120mg, 160mg Modified release tablets 120mg Half Securon SR ®, 240mg Securon SR® Injection 5 mg in 2 ml Infusion 200mg/ml Tablets 30mg Nimodipine Notes: 1. Specify the brand when prescribing a modified release diltiazem preparation (excluding 60mg tablet). 2. Specify the brand when prescribing a modified release verapamil preparation. 3. Verapamil is used where there is co-existing paroxysmal supraventricular tachycardia, or atrial fibrillation ±hypertension ± angina. 4. Verapamil has several significant drug interactions (see BNF for comprehensive list) including: β-blockers when asystole, severe hypotension and heart failure may ensue; digoxin where the plasma levels of digoxin may be increased, and there is risk of AV block and bradycardia. 5. Nimodipine is included for the prevention and treatment of ischaemic neurological deficits following subarachnoid haemorrhage. 6. Although nifedipine has been removed from the formulary, patients currently taking nifedipine obtaining benefit with no adverse effects, should remain on the product and not be switched. 2.6.3 Other antianginal drugs Nicorandil Tablets 10mg, 20mg Ivabradine Tablets 5mg, 7.5mg Note: 1. Nicorandil has similar efficacy to other anti-angina drugs in controlling symptoms but there is little evidence about its efficacy in combination with other anti-angina drugs. However, when added to maximal therapy with other antiangina drugs in refractory unstable angina (unlicensed indication) it may produce additional benefit. 2. Nicorandil is a potassium channel activator with nitrate properties; therefore additional nitrates may not be needed. 3. Nicorandil is associated with a risk of gastrointestinal ulceration, including perianal ulceration. Although mouth ulceration has long been recognised as a side-effect of nicorandil treatment, its use has more recently been associated with ulceration of any region of the gastrointestinal tract including the perianal area. The ulceration is commonly severe and, in a few patients, has led to perforation. Time to onset may vary widely. These ulcers are refractory to treatment; they respond only to withdrawal of nicorandil, which should be done only under the supervision of a cardiologist. 4. It is recommended that nicorandil should only be prescribed on the advice of a specialist or by someone with a specialist interest. 5. Ivabradine may be useful for the symptomatic treatment of chronic stable angina pectoris in patients with normal sinus rhythm, for whom heart rate control is desirable, and who have a contra-indication or intolerance for betablockers and rate-limiting calcium-channel blockers. 6. The ‘Beautiful’ study demonstrated ivabradine safety with significant LV dysfunction, in addition to a beta blocker. With angina and impaired LV, ivabradine can be used in preference to a calcium antagonist. 7. NICE has approved the use of ivabradine as a treatment option for chronic heart failure in certain patients after a four week stabilisation period on optimised standard treatments (TA267 Nov 2012) 2.6.4 Peripheral and cerebral vasodilators NICE CG 147: Lower limb peripheral artery disease (August 2012) gives guidance on the diagnosis and management of lower limb peripheral artery disease. NICE has issued guidance on the use of vasodilators in peripheral artery disease (TA 223 May 2011) Only Naftidrofuryl oxalate is recommended as an option for the treatment of intermittent claudication in people with peripheral arterial disease for whom vasodilator therapy is considered appropriate after taking into account other treatment options. Treatment with naftidrofuryl oxalate should be started with the least costly licensed preparation. Patients should be assessed for improvements after 3 to 6 months First line drugs Second line drugs Specialist drugs Specialist only drugs Page 10 of 20 Naftidrofuryl oxalate Capsules 100mg 2.7 Sympathomimetics 2.7.1 Inotropic Sympathomimetics Dobutamine 2.7.2 Vasoconstrictor Sympathomimetics Ephedrine Injection 30mg in 1ml Metaraminol Injection 10mg in 1ml Noradrenaline Injection 4mg in 4ml Phenylephrine Injection 10mg in 1ml 2.7.3 Cardiopulmonary resuscitation Epinephrine (rINN) Injection 1mg in 10ml (Minijet®), Injection 1mg in 1ml Adrenaline (BAN) Injection 250mg in 20ml Note: Refer to BNF Chapter 3 for adrenaline used in the management of anaphylaxis. 2.8 Anticoagulants and reversal agents 2.8.1 Parenteral anticoagulants Enoxaparin Clexane® Pre-filled syringe for subcutaneous injection 100mg in 1ml, 120mg in 0.8ml, 150mg in 1ml, 20mg in 0.2ml, 40mg in 0.4ml, 60mg in 0.6ml, 80mg in 0.8ml For use in unstable angina and NSTEMI, DVT and PE Tinzaparin Innohep® 10,000u/ml for prophylaxis DVT, 20,000 u/ml for treatment of DVT and PE For use in DVT and PE Bivalirudin▼ Angiox® powder for reconstitution 250mg vial Epoprostenol Flolan® Infusion. Powder for reconstitution 500 micrograms Fondaparinux Heparin Arixtra® Injection Pre-filled syringe 2.5mg in 0.5ml Injection 2iu/ml in 500ml, 10iu/ml 5ml, 100iu/ml 2ml, 1000iu/ml 5ml and 20ml, 5000iu/ml 5ml, 25,000iu/ml 0.2ml and 5ml For use in unstable angina and NSTEMI 1. The use of antiplatelet therapy, thrombolytics and anti-thrombin treatment in patients with unstable angina and NSTEMI are covered in NICE CG 94: Unstable angina and NSTEMI 2. Bivalirudin is indicated for the treatment of STEMI in patients undergoing PCI when used in accordance with NICE TA 230: Bivalirudin for the treatment of STEMI (Jul 2011) 3. Guidance for the prevention of VTE in patients admitted to hospital is detailed in NICE CG 92: Venous thromboembolism - reducing the risks Prophylaxis for VTE prevention should continue for 14 days post knee revision and 35 days post hip revision. 4. NICE CG 144: The management of venous thromboembolic diseases gives guidance on the care of adults with VTE 5. Approved dosing regimens for Angiox (bivalirudin) for PCI following reports of inappropriate use. See Direct Healthcare Professional Communication January 2013 First line drugs Second line drugs Specialist drugs Specialist only drugs Page 11 of 20 2.8.2 Oral anticoagulants Warfarin Tablets 0.5mg, 1mg, 3mg, 5mg Phenindione Apixaban▼ Dabigatran▼ Tablets 10mg, 25mg, 50mg Eliquis® 2.5mg, 5mg tablets See below for indications Pradaxa® capsules 75mg, 110mg, 150mg See below for indications Edoxaban▼ Rivaroxaban▼ Lixiana® tablets 15mg, 30mg, 60mg See below for indications Xarelto® tablets 2.5mg, 10mg, 15mg, 20mg See below for indications 1. Phenindione may be used exceptionally when warfarin is not appropriate. (Licensed indications differ). 2. Nurse Specialist, Haemostasis and Thrombolysis, available at EDGH and Conquest for expert advice on request. 3. All prescribers have a responsibility to ensure awareness of any existing medications the patient may be taking (including over the counter and herbal medicines) and the potential for interaction when prescribing anticoagulants. All prescribers should ensure that their practice is compliant with the recommendations of the NPSA Patient Safety Alert No.18: Actions that can make anticoagulant therapy safer 5. The formulary status of the oral thrombin inhibitors is dependent on the indication it is being used for – see table below. 6. For appropriate dosing in renal impairment please consult the appropriate summary of product characteristics for dabigatran, rivaroxaban, apixaban and edoxaban 7. Prophylaxis of venous thromboembolic events after elective hip and knee surgery Apixaban, Dabigatran and Rivaroxaban are all approved by NICE for the prophylaxis of venous thromboembolic events after elective hip and knee surgery as an alternative to low molecular weight heparins. No therapeutic monitoring is required. Patients are discharged with the full course of treatment. 8. Prevention of stroke and systemic embolism in adults with non-valvular atrial fibrillation Apixaban, Dabigatran, Edoxaban and Rivaroxaban are now licensed and approved by NICE to prevent stroke in patients with atrial fibrillation with a CHA2DS2-VASC score of ≥2 or in males with a CHA2DS2-VASC score ≥ 1. Prescribing should be in accordance with the approved treatment pathway below. 9. Acute DVT & PE treatment and VTE prophylaxis Rivaroxaban is approved by NICE as a treatment option for the treatment of acute DVT or PE and prevention of recurrent DVT and PE. Dabigatran is approved by NICE as a treatment option for treatment and secondary prevention of DVT and PE Apixaban is approved by NICE as a treatment option for treatment and secondary prevention of DVT and PE Edoxaban is approved by NICE as a treatment option for treatment and secondary prevention of DVT and PE 10. Prevention of atherothrombotic events in acute coronary syndrome Rivaroxaban in combination with aspirin and clopidogrel or aspirin alone is approved by NICE as a treatment option for preventing further atherothrombotic events in patients with ACS. Prescribing responsibility will remain with the cardiologists. 11. The MHRA drug Safety Update July 2012 gives updated advice on contraindications and warnings for dabigatran and on switching treatment to and from dabigatran. Dabigatran is contraindicated in clinical conditions associated with a significant risk of bleeding, such as: current or recent gastrointestinal ulceration oesophageal varices malignant neoplasms arteriovenous malformations recent brain or spinal injury vascular aneurysms recent brain, spinal or ophthalmic surgery major intraspinal or intracerebral vascular recent intracranial haemorrhage abnormalities 12. The benefits and risks of starting dabigatran should also be considered carefully for patients who may have other conditions that put them at an increased risk of major bleeding (but in whom treatment with dabigatran is not contraindicated) 13. The above has since been extended to include ALL new oral anticoagulants (apixaban, dabigatran and rivaroxaban in MHRA Drug Safety update (October 2013) 14. Use of dabigatran is contraindicated with dronedarone, and with other anticoagulants, except when switching treatment to or from dabigatran, or with the use of unfractionated heparin for maintenance of venous or arterial catheter patency 15. Concomitant use of antiplatelet agents increases the risk of major bleeding with dabigatran approximately twofold, therefore a careful benefit-risk assessment should be made prior to initiation of treatment First line drugs Second line drugs Specialist drugs Specialist only drugs Page 12 of 20 16. Pradaxa® (dabigatran) is now contraindicated in patients with prosthetic heart valve requiring anti-coagulant treatment. related to their valve surgery. This is regardless of the length of time elapsed since valve replacement took place. The contraindication is based on clinical trial data which showed an increased frequency of thromboembolic and bleeding events in the group of patients treated with dabigatran, compared with warfarin. See Boehringer Ingelheim letter January 2013 and MHRA Drug Safety Update March 2013 Formulary status of NOACs VTE prophylaxis (post surgical NB: Full course of treatment to be supplied by hospital Stroke prevention in AF Apixaban Dabigatran Edoxaban Rivaroxaban Adults(18+) Eliquis® 2.5mg twice daily for 1014 days (knees) or 32-38 days (hips) Adults (18 - 74): Pradaxa® 110mg stat then 220mg daily for 9 days (knees) or 27-34 days (hips) Adults (75+): Pradaxa® 75mg stat then 150mg daily for 9 days (knees) or 27-34 days (hips) N/A Adults(18+): Xarelto® 10mg daily for 14 days (knees) or 35 days (hips) Adults (18+) Eliquis® 5mg twice a day Adults (18-74): Pradaxa® 150mg twice daily Adults (75+): Pradaxa® 110mg twice daily Adults (18+): Lixiana® 60mg once a day In patients with one or more of the following: • Moderate or severe renal impairment (creatinine clearance (CrCL) 15-50 mL/min) • Low body weight ≤ 60 kg • Concomitant use of ciclosporin, dronedarone, erythromycin or ketoconazole. Lixiana® 30mg once a day After at least 5 days of parenteral anticoagulation: Adults (18+): Lixiana® 60mg once a day. Lixiana® 30mg once a day in patients with one or more risk factors (see above) Adults (18+): Xarelto® 20mg daily N/A Adults (18+) Xarelto® 2.5mg twice daily in combination with aspirin/ aspirin + clopidogrel. Treatment for up to 1 year. In patients with at least two of the following characteristics: age ≥ 80 years, body weight ≤ 60 kg serum creatinine ≥ 1.5 mg/dl (133 micromole/l). Eliquis® 2.5mg twice a day DVT and PE acute treatment & VTE prophylaxis Treatment of acute DVT and treatment of PE (Adults 18+): Eliquis® 10 mg twice daily for the first 7 days followed by 5 mg twice daily for up to 6 months (see below) Prevention of recurrent DVT and PE (Adults 18+): Eliquis® 2.5 mg twice daily following completion of 6 months of treatment with Eliquis® 5 mg twice daily or with another anticoagulant (see SPC for further information) Prevention of atherothrombotic events in acute coronary syndrome First line drugs N/A Second line drugs After at least 5 days of parenteral anticoagulation: Adults (18-74): Pradaxa® 150mg twice daily Adults (75-79): Pradaxa® 110mg – 150mg twice daily depending on pts individual risk/benefit Adults (80+) Pradaxa® 110mg twice daily See SPC for other groups where dose will depend on individual patient’s risk benefit ratio N/A Specialist drugs Adults (18+) Xarelto® 15mg twice daily from days 1 to 21 Xarelto® 20mg daily from day 22 onwards Specialist only drugs Page 13 of 20 Treatment Pathway – Prevention of stroke and systemic embolism in adults with non-valvular atrial fibrillation Assess risk of bleeding using the HAS-BLED score and address the following modifiable risk 2 factors where appropriate Uncontrolled hypertension Poor INR control Concomitant drugs which increase bleeding risk Harmful alcohol consumption CHA2DS2-VASc score ≥ 2 or CHA2DS2-VASc score 1 1, 2 and male Has the patient been prescribed warfarin? NO 3,4 YES Explore reasons for poor concordance with the patient. Revisit anticoagulation options including no treatment, using the NICE Patient 4 Decision Aid NO Informed discussion between clinician and patient about the risks and benefits of warfarin, apixaban, dabigatran and rivaroxaban for that patient. This must take into account contraindications (e.g.renal & liver 5,6 function) , co-morbidities, concomitant medication and 7 concordance . Is the patient complying with treatment? (assess at ≥ 3 months) YES Does the patient have good INR control? (TTR ≥ 65%) NO Can the patient be (re)considered for warfarin? YES NO Continue on warfarin YES Prescribe warfarin Consider prescribing apixaban, dabigatran or rivaroxaban particularly in patients with: 7 - Poor INR control despite evidence they are complying 5 - Contraindications , allergy to or intolerable side effects from warfarin 1 From NICE CG 180 June 2014 available at: http://www.nice.org.uk/Guidance/CG180 Patients eligible for but not taking anticoagulants should have their stroke and bleeding risk reviewed annually. 3 Patient FAQs can be found at: http://nww.searchgpinfo-sussex.nhs.uk/prescribing/docs/2014/OAC_AF_FAQs 4 A patient decision aid can be found at http://guidance.nice.org.uk/CG180/PatientDecisionAid/pdf/English 5Many contraindications to warfarin also apply to the NOACs. Specialist advice may need to be sought before initiating warfarin– contraindicated patients on apixaban, dabigatran or rivaroxaban. 6 Renal function should be assessed prior to the initiation of dabigatran and then at least once a year as needed. Monitoring of the renal function of patients on apixaban and rivaroxaban at baseline and then at least once a year should be considered. 7 Poor concordance with warfarin is not an indication for initiating a NOAC as these drugs have shorter half-lives. 2 First line drugs Second line drugs Specialist drugs Specialist only drugs Page 14 of 20 2.8.3 Protamine Sulphate Protamine Injection 50mg in 5ml Used to treat overdosage of unfractionated or low molecular weight heparins 2.8.4 Idarucizumab ▼ Idarucizumab Praxbind® Injection 2.5g in 50ml Praxbind is a humanised monoclonal antibody fragment (Fab) that binds to dabigatran with very high affinity thereby reversing its effect. It is indicated to rapidly reverse the effects of dabigatran for emergency surgery or urgent procedures and in the event of life-threatening or uncontrolled bleeding. For use only in accordance with the protocol Management of stroke Alteplase is recommended by NICE to treat acute ischaemic stroke in adults. See NICE TA 264 for further details. 2.9 Antiplatelet drugs Aspirin Clopidogrel Dipyridamole Dispersible tablets 75mg Tablets 75mg Tablets 100mg Modified release capsules 200mg Prasugrel Tablets 5mg, 10mg Ticagrelor Tablets 90mg, 60mg Abciximab Eptafibitide See protocols To be used as adjunct to PTCA See protocols For high risk unstable angina Notes: 1. Enteric-coated aspirin tablets are not recommended. There is no convincing evidence that at a daily dose of 75 mg using enteric-coated rather than soluble aspirin reduces the risk of gastrointestinal bleeding. (Ref: DTB Jan 1997 p7-8). 2. The use of clopidogrel with low dose aspirin is recommended for up to 1 year after acute coronary syndromes, up to 1 year after drug eluting stent insertion and up to 3 months after bare metal stenting and occasionally for longer at the discretion of the operator. 3. Current evidence demonstrates that after one year of clopidogrel with low dose aspirin, the risks of continued treatment outweigh the benefits. 4. See NICE CG 94 (March 2010) Unstable angina and NSTEMI and CG172: Secondary prevention in primary and secondary care for patients following a myocardial infarction Nov 2013 for further information. 5. Clopidogrel should NOT be substituted for aspirin, where patient has GI discomfort or bleed. Gastroprotection with PPI should be considered (lansoprazole 15mg capsules). 6. Prasugrel (Efient®) is an antiplatelet agent with a similar mode of action to clopidogrel. 7. It is licensed for use in conjunction with aspirin for the prevention of atherothrombotic events in patients with acute coronary syndrome (i.e., unstable angina, non-ST segment elevation myocardial infarction [UA/NSTEMI] or ST segment elevation myocardial infarction [STEMI]) undergoing primary or delayed percutaneous coronary intervention (PCI). 8. In certain patient groups it has demonstrated superior efficacy to clopidogrel but at a cost of an increased risk of major bleeding. 9. It is administered as a 60mg loading dose with a maintenance dose of 10mg daily for up to 12 months. A 5mg daily maintenance dose is recommended for individuals weighing less than 60kg. 10. NICE TA 317 (July 2014): Prasugrel 10 mg in combination with aspirin is recommended as an option for preventing atherothrombotic events in adults with acute coronary syndrome (unstable angina [UA], non-ST segment elevation myocardial infarction [NSTEMI] or ST segment elevation myocardial infarction [STEMI]) having primary or delayed percutaneous coronary intervention. 11. Ticagrelor (Brilique®) is a new antiplatelet agent licensed for use in combination with aspirin to prevent atherothrombotic events after acute coronary syndrome. 12. In studies ticagrelor was found to be more effective at preventing further atherothrombotic events than clopidogrel but at the expense of an increased risk of bleeding and increased incidence of dypsnoea. First line drugs Second line drugs Specialist drugs Specialist only drugs Page 15 of 20 13. Initiation must be undertaken by a cardiologist. GPs may prescribe continuation of treatment on the advice of the specialist for up to 12 months. 14. NICE TA 260: Ticagrelor for the treatment of acute coronary syndromes (ACS) (Oct 2011) recommends that: Ticagrelor 90mg in combination with low-dose aspirin is recommended for up to 12 months as a treatment option in adults with acute coronary syndromes (ACS) that is, people: with ST-segment-elevation myocardial infarction (STEMI) – defined as ST elevation or new left bundle branch block on electrocardiogram – that cardiologists intend to treat with primary percutaneous coronary intervention (PCI) or with non-ST-segment-elevation myocardial infarction (NSTEMI) or admitted to hospital with unstable angina – defined as ST or T wave changes on electrocardiogram suggestive of ischaemia plus one of the characteristics defined in section 1.2. Before ticagrelor is continued beyond the initial treatment, the diagnosis of unstable angina should first be confirmed, ideally by a cardiologist. 15. NICE TA 420: Ticagrelor for preventing atherothrombotic events after myocardial infarction (December 2016) Ticagrelor 60mg, in combination with aspirin, is recommended within its marketing authorisation as an option for preventing atherothrombotic events in adults who had a myocardial infarction and who are at high risk of a further event. Treatment should be stopped when clinically indicated or at a maximum of 3 years 16. Ticagrelor has a twice daily dosage regime. 17. NICE TA 210: Clopidogrel and modified release dipyridamole for the prevention of occlusive vascular events (review of TA 90) (Dec 2010) NICE has recommended that: Clopidogrel is an option to prevent occlusive vascular events: For people who have had an ischaemic stroke, have peripheral arterial disease or multivascular disease; or For people who have had a myocardial infarction only if aspirin is contra-indicated or not tolerated The combination of MR dipyridamole and aspirin is used as part of the prevention of occlusive vascular events in people who have had a transient ischaemic attack; or an ischaemic stroke if clopidogrel is contraindicated or not tolerated Modified release dipyridamole alone is an option to prevent occlusive vascular events For people who have had an ischaemic stroke only if aspirin and clopidogrel are contraindicated or not tolerated; or For people who have had a transient ischaemic attack only if aspirin is contraindicated or not tolerated. MHRA Drug Safety Update – Interaction between the use of clopidogrel and PPI’s – April 2010 In light of the most recent evidence, the previous advice on the concomitant use of clopidogrel with proton pump inhibitors has now been modified. Use of either omeprazole or esomeprazole with clopidogrel should be discouraged. The current evidence does not support extending this advice to other PPIs. 2.10 Myocardial infarction and fibrinolysis 2.10.1 Fibrinolytic drugs Streptokinase Tenecteplase Urokinase Injection 1.5 million units See ESHT guidelines 30 – 50mg according to body weight See ESHT guidelines 10,000 unit vial 2.11 Antifibrinolytic drugs and haemostatics Tranexamic Acid Aprotinin Etamsylate First line drugs Tablets 500mg 50ml vial Tablets 500mg Second line drugs Specialist drugs Specialist only drugs Page 16 of 20 2.12 Lipid-lowering drugs Tablets 10mg Bezafibrate Fenofibrate (Bezalip mono®) Modified Release Tablets 400mg Supralip® 160 Tablets 160mg Ezetimibe NB: Licensed for use in primary hypercholesterolaemia and homozygous familial hypercholesterolaemia Fibrates Specialist input should be sought when prescribing a fibrate in combination with a statin Statins Atorvastatin Tablets 10mg, 20mg, 40mg, 80mg Simvastatin Tablets 20mg, 40mg, Rosuvastatin Crestor® Tablets 5mg, 10mg, 20mg, 40mg On specialist recommendation: for treatment of familial hypercholesterolaemia and in patients intolerant to 3 other statins Omega-3 fatty acid compounds Omega-3-acid Ethyl Esters On specialist recommendation for treatment of hypertriglyceridaemia Omacor® capsules Reduction in Low density lipoprotein cholesterol Dose (mg/day) 5 10 20 40 80 27%1 33%2 Fluvastatin - - 21%1 Pravastatin - 20%1 24%1 29%1 - Simvastatin - 27%1 32%2 37%2 42%3,4 Atorvastatin - 37%2 43%3 49%3 55%3 Rosuvastatin 38%2 43%3 48%3 53%3 - 1 20% - 30%: low intensity 31% - 40%: medium intensity 3 above 40%: high intensity 4 Advice from the MHRA: there is an increased risk of myopathy associated with high-dose (80 mg) simvastatin. The 80 mg dose should be considered only in patients with severe hypercholesterolaemia and high risk of cardiovascular complications who have not achieved their treatment goals on lower doses, when the benefits are expected to outweigh the potential risks. 2 See NICE guidance CG181 (July 2014) Lipid modification: cardiovascular risk assessment and modification of blood lipids for the primary and secondary prevention of cardiovascular disease The decision whether to start statin therapy should be made after an informed discussion between the clinician and the person about the risks and benefits of statin treatment, taking into account additional factors such as potential benefits from lifestyle modifications, informed patient preference, comorbidities, polypharmacy, general frailty and life expectancy. 1. Offer atorvastatin 20mg for primary prevention of CVD to people who have a 10% or greater 10-year risk of developing CVD. Estimate the level of risk using the QRISK2 assessment tool 2. For people 85 years or older consider atorvastatin 20mg for primary prevention as statins may be of benefit in reducing the risk of non-fatal myocardial infarction. Be aware of factors that may make treatment inappropriate (see above). 3. Start statin treatment in people with CVD with atorvastatin 80mg. Use a lower dose of atorvastatin if any of the following apply: a. potential drug interactions b. high risk of adverse effects c. patient preference 4. Consider statin treatment for the primary prevention of CVD in all adults with type 1 diabetes. First line drugs Second line drugs Specialist drugs Specialist only drugs Page 17 of 20 5. Offer statin treatment for the primary prevention of CVD to adults with type 1 diabetes who: a. are older than 40 years or b. have had diabetes for more than 10 years or c. have established nephropathy or d. have other CVD risk factors. 6. Start treatment for adults with type 1 diabetes with atorvastatin 20mg 7. Offer atorvastatin 20mg for the primary prevention of CVD to people with type 2 diabetes who have a 10% or greater 10-year risk of developing CVD. Estimate the level of risk using the QRISK2 assessment tool. 8. Offer atorvastatin 20mg for the primary or secondary prevention of CVD to people with CKD. a. Increase the dose if a greater than 40% reduction in non-HDL cholesterol is not achieved (see recommendation 1.3.28) and eGFR is 30 ml/min/1.73 m2 or more. b. Agree the use of higher doses with a renal specialist if eGFR is less than 30 ml/min/1.73 m 2. 9. Measure total cholesterol, HDL cholesterol and non-HDL cholesterol in all people who have been started on highintensity statin treatment at 3 months of treatment and aim for a greater than 40% reduction in non-HDL cholesterol. If a greater than 40% reduction in non-HDL cholesterol is not achieved: a. discuss adherence and timing of dose b. optimise adherence to diet and lifestyle measures 10. Consider increasing dose if started on less than atorvastatin 80 mg and the person is judged to be at higher risk because of comorbidities, risk score or using clinical judgement. Advice and monitoring for adverse effects 1. Advise people who are being treated with a statin: a. that other drugs, some foods (for example, grapefruit juice) and some supplements may interfere with statins and b. to always consult the patient information leaflet, a pharmacist or prescriber for advice when starting other drugs or thinking about taking supplements. 2. Remind the person to restart the statin if they stopped taking it because of drug interactions or to treat intercurrent illnesses. 3. Before offering a statin, ask the person if they have had persistent generalised unexplained muscle pain, whether associated or not with previous lipid-lowering therapy. If they have, measure creatine kinase levels. a. If creatine kinase levels are more than 5 times the upper limit of normal, re-measure creatine kinase after 7 days. If creatine kinase levels are still 5 times the upper limit of normal, do not start statin treatment. b. If creatine kinase levels are raised but less than 5 times the upper limit of normal, start statin treatment at a lower dose. 4. Advise people who are being treated with a statin to seek medical advice if they develop muscle symptoms (pain, tenderness or weakness). If this occurs, measure creatine kinase. 5. Measure baseline liver transaminase enzymes (alanine aminotransferase or aspartate aminotransferase) before starting a statin. Measure liver transaminase within 3 months of starting treatment and at 12 months, but not again unless clinically indicated. 6. Do not routinely exclude from statin therapy people who have liver transaminase levels that are raised but are less than 3 times the upper limit of normal. 7. Do not stop statins because of an increase in blood glucose level or HbA1c. 8. Statins are contraindicated in pregnancy Intolerance of statins 1. If a person is not able to tolerate a high-intensity statin aim to treat with the maximum tolerated dose. 2. The following strategies can be tried to manage adverse events: a. stop the statin and try again when the symptoms have resolved to check if the symptoms are related to the statin b. reduce the dose within the same intensity group c. change the statin to a lower intensity group. Interactions Statins may differ in terms of their pharmacology and interactions with other drugs. Simvastatin has been the subject of a Drug Safety Update (August 2012) which reports contraindications and maximum dose recommendations when taken in combination with specific drugs. Rosuvastatin should only be used on the advice of a lipid clinic specialist in the following situations: Patients with familial hypercholesterolaemia (FH) not achieving the 50% reduction target specified in NICE CG71: Identification and management of familial hypercholesterolaemia (which may also include FH First line drugs Second line drugs Specialist drugs Specialist only drugs Page 18 of 20 patients who cannot tolerate atorvastatin) Patients who have CVD or who are at high risk of CVD who have tried and are intolerant to 3 different statins after seeking advice from a specialist (which could be e-mail or telephone advice) Specific patients with complex co-morbidities referred to the lipid clinic and on specialist advice NICE TA 385 (Feb 2016): Ezetimibe for treating primary heterozygous-familial and non-familial hypercholesterolaemia 1. Ezetimibe monotherapy is recommended as an option for the treatment of adults with primary (heterozygousfamilial or non-familial) hypercholesterolaemia who would otherwise be initiated on statin therapy (as per NICE guidance CG181) but who are unable to do so because of contraindications to initial statin therapy. 2. Ezetimibe monotherapy is recommended as an option for the treatment of adults with primary (heterozygousfamilial or non-familial) hypercholesterolaemia who are intolerant to statin therapy. 3. For the purposes of this guidance, intolerance to initial statin therapy should be defined as the presence of clinically significant adverse effects from statin therapy that are considered to represent an unacceptable risk to the patient or that may result in compliance with therapy being compromised. Adverse effects include evidence of new-onset muscle pain (often associated with levels of muscle enzymes in the blood indicative of muscle damage), significant gastrointestinal disturbance alterations of liver function tests. 4. Ezetimibe, coadministered with initial statin therapy, is recommended as an option for the treatment of adults with primary (heterozygous-familial or non-familial) hypercholesterolaemia who have been initiated on statin therapy (as per NICE guidance CG181) when: serum total or low-density lipoprotein (LDL) cholesterol concentration is not appropriately controlled either after appropriate dose titration of initial statin therapy or because dose titration is limited by intolerance to the initial statin therapy and consideration is being given to changing from initial statin therapy to an alternative statin. 5. For the purposes of this guidance, appropriate control of cholesterol concentrations should be based on individualised risk assessment in accordance with national guidance on the management of cardiovascular disease for the relevant populations. 6. When the decision has been made to treat with ezetimibe co-administered with a statin, ezetimibe should be prescribed on the basis of lowest acquisition cost. Additional guidance 1. NICE guidance on Identification and management of familial hypercholesterolaemia (CG71 Aug 2008 rev Jul 2016) 2. CG172: Secondary prevention in primary and secondary care for patients following a myocardial infarction Nov 2013 PCSK9 inhibitors Alirocumab▼ Praluent® Solution for injection, 75mg, 150mg PFS, Pen ▼ Repatha® Solution for injection, Evolocumab 140mg PFS, Pen NICE has approved the use of the monoclonal antibodies, Alirocumab and Evolocumab to treat patients with primary hypercholesterolaemia or mixed dyslipidaemia where LDL-C concentrations remain above the threshold specified in the table below despite maximal tolerated lipid lowering therapy. These treatments are self-administered by subcutaneous injection every 2 weeks. Assessment, initiation, prescribing and monitoring of these treatments is through lipid clinics only. LDL-C concentrations above which alirocumab and evolocumab are recommended Without CVD With CVD High risk of CVD 1 Primary non-familial Not recommended at any Recommended only if hypercholesterolaemia or LDL-C concentration LDL-C concentration is mixed dyslipidaemia persistently above First line drugs Second line drugs Specialist drugs Very high risk of CVD 2 Recommended only if LDL-C concentration is persistently above Specialist only drugs Page 19 of 20 4.0 mmol/litre 3.5 mmol/litre Recommended only if LDL-C concentration is persistently above 3.5 mmol/litre Primary heterozygous-familial Recommended only if hypercholesterolaemia LDL-C concentration is persistently above 5.0 mmol/litre 1 High risk of CVD is defined as a history of any of the following: acute coronary syndrome (such as myocardial infarction or unstable angina needing hospitalisation); coronary or other arterial revascularisation procedures; chronic heart disease; ischaemic stroke; peripheral arterial disease. 2 Very high risk of CVD is defined as recurrent cardiovascular events or cardiovascular events in more than 1 vascular bed (that is, polyvascular disease). Abbreviations: CVD, cardiovascular disease; LDL-C, low-density lipoprotein cholesterol. First line drugs Second line drugs Specialist drugs Specialist only drugs Page 20 of 20