* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download and they will dilat
Survey
Document related concepts
Transcript
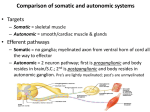
• what happens to local arterioles? they are sensitive to these mechanisms (due to increased metabolism), and they will dilate in response to them (they are called vasodilators). this decreases resistance therefore increases blood flow, oxygen delivery re-established until levels return to normal. • local vasodilators/products of metabolism: 1) Adenosine – an indicator that the cells are using ATP 2) Co2 3) Lactic acid 4) K+ 5) H+ • What are some local hormones? 1) prostaglandins which can cause constriction or dilation 2) NO from endothelium to cause relaxation 3) histamine to cause dilation, 4) endothelin from endothelium cells to cause VASOconstriction. • what are some methods of local regulation by physical factors? 1) heat, will cause vasodilation of arterioles. 2) also MYOGENIC response; this keeps blood flow constant. flow goes up initially when pressure goes up, but returns to normal quickly by resisting changes in tension. ONLY HAPPENS IN SPECIAL areas where you want to keep blood flow constant regardless of systemic pressure changes. Therefore these local hormones and products of metabolism and physical factors (only in certain areas) regulate local blood flow by vasoconstriction/dilation • Q: Each tissue has its own preferred local factor for regulating local blood flow, use the heart as an example of one of specialised methods for extracting oxygen, and why is this necessary? • A: The strongests stimulus for local dilation is a decrease in O2, then an increase in K+ and Adensosine. During systole, the heart is contracting and this restricts blood from reaching the coronary arteries, exactly when the heart is in most need of oxygen. for this reason, it has a specialised method wherein it can extract more oxygen that any other tissue. • Q: Use the brain as an example of local regulation of blood flow? • A: The brain uses local CO2 levels as the most sensitive way to regulate flow. Blood flow will increase markedly as CO2 goes up. This is because neuronal function is particularly affected by H+ levels. As acid goes up, brain activity is depressed; therefore must keep pH levels tightly regulated. • Q: Why is hyperventilation bad, and why does breathing into a bag help? • A: When you hyperventilate, you blow off a lot of CO2, without inhaling sufficient O2, the neurons will also become more excitable. As there is only low levels of CO2, and thus also low H+, the local tissues do not receive the stimulus to dilate and increase blood flow to the brain, so you become dizzy. Breathing into a bag allows for you to re-uptake CO2, causing vasodilation and allowing blood flow to increase and deliver more O2 to the neurons. • Q: Why is it good that cerebral blood flow is not regulated by ANS? • A: when you exercise, you do not want arteries in brain to vasoconstrict due to sympathethic effects, as you still require O2 to the brain, otherwise you would pass out. • Q: Use the skeletal muscle as an example for regulation of local blood flow? • A: All of the above metabolic factors. Also, the skeletal muscle pump which works during exercise, will pump harder, increasing blood flow into the skeletal muscle. This will carry with it the metabolic factors. Your blood flow stays high after exercise finished even though skeletal pump stopped, as the metabolic factors stay high in the muscle (accumulation of lactic acid must be removed) • Q: Why does blood pressure only go up by a small fraction during exercise, even though cardiac output increases significantly? • A: Total peripheral resistance decreases due to vasodilation, this is due to the binding of adrenaline to B-adrenoreceptors. The heart and coronary arteries, and arteries to brain also have B-receptors. (a1-adrenoreceptors are found in kidneys, gut – causes vasoconstriction.) • Q: what is the dominating signal for changes in blood pressure in the skeletal muscle? Why do these not dominate in the kidney, gut etc? • Metabolic factors, these override and dominate over adrenalin to cause vasodilation. These metabolic factors don’t dominate in kidney gut etc as these are not exercising tissues, therefore are primarily affected by adrenalin (binds to a-receptors) to cause constriction. • Q: What is the major factor for regulating blood flow in the skin? • A: Temperature, causing vasodilation to cool you down. Module 4 • Q: Anatomical differences between pre/post ganglionic fibres in sympathetic/parasympathethic? • A: In sympathetic, the preganglionic fibres are short, and synapse on the chain of ganglia, close to the spinal cord. The outflow onto post-ganglionic fibres which are also close to spinal cord, synapse onto target tissue. In para, the pre-ganglionic fibres synapse onto post-ganglionic fibres actually in the tissue, which go on to innervate the tissue. (therefore long pre-ganglionic fibres) • Q: What are special about the cells in the adrenal chromaffin glands? • A: They are honorary post-ganglionic fibres, therefore pre-ganglionic sympathethic fibres actually synapse on the tissue, to cause release of adrenalin from the cells. • Q: Draw differences between sympathethic and parasympathethic ganglia, highlighting the different NT’s and receptors. • IMPORTANT FACTORS FOR Cholinergic/CATCHEOLAMINergic: Synthesis, packaging, release, post-synaptic actions, degradation and uptake. • Q:How is AcH synthesised? • A: Choline + Acetyl Coa, this occurs in cytosol. Then is pumped into vesicle, using an active proton pump which pumps into H+. ACh then transported into vesicle using H+/AcH antiporter, down H+ gradient. • Q: What are two AcH receptors? • A: Nicotinic and Muscarinic. Nicotinic is a ligand gated ion channel and binding of AcH results in Na+ influx and depolarisation. Muscarinic is a GPCR, resulting in a signalling cascade through 2nd messengers and hyperpolarisation. • Q: What is involved in the parasympathethic activity on the heart? • A: The AcH secreted from the post-ganglionic neurons binds to GPCR muscarinic receptors on the cardiac cells, the B-y subunits of the g-protein interact with a K+ channel, opening it, causing hyperpolarisation through efflux of K+, to slow down contraction rate. • Q: How is AcH is removed from the synapse? • A: Through acetycholinesterase (which is targeted by herbicides) present in the synaptic cleft degrades AcH, the choline is then re-uptaken into the pre-synaptic region. • Q: How is adrenaline synthesised? • A: made from its pre-cursor Tyrosine->Dopamine (cytosol)-> (in granule) Noradrenaline>Adrenaline (in granule) (by enzymes). Dopamine is pumped in the same way as AcH through proton exchange. In the post-ganglionic sympathethic NS fibre, Dopamine Hydroxylase is the enzyme to convert Dopamine to Noradrenaline. In the chromaffin cells, PNMT is also present to convert Noradrenaline to Adrenalin. • Q: What are the post-synaptic actions of Catacholamines? • A: There are B1 (on the heart) (dilation, using Gas protein) and a1 (constriction, using Gai protein) receptors (blood vessels). All catecholamines are receptors are GPCRs. The type of G protein determines actions. • Q: How are catecholaminergic NT’s removed from the synapse? • A: Is reuptaken to presynaptic (uptake 1) or postsynaptic cell (via uptake 2) • Q: What does Cocaine do? • A: Blocks Uptake 1 in central synapse, keeping catcholamine NT in synapse, maintaining action on post-synaptic receptors, giving pleasurable feeling. • Q: What are sympathomimetic drugs and how do they take effect? • A: They mimic noradrenaline, therefore are recognised by uptake transporters, therefore are taken back up into pre-synaptic neurons, where they are also recognised as NT’s. They are