* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Key issues in Chronic Heart Failure Chronic Heart Failure (CHF)
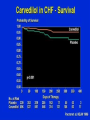
Discovery and development of beta-blockers wikipedia , lookup
5-HT3 antagonist wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Psychopharmacology wikipedia , lookup
NK1 receptor antagonist wikipedia , lookup
Prescription costs wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
CONTEMPORARY STANDARDS IN TREATMENT OF CHRONIC HEART FAILURE JERZY JANKOWSKI MD DEPARTMENT OF CLINICAL PHARMACOLOGY http://www.zfk.ump.edu.pl/ Key issues in Chronic Heart Failure Chronic Heart Failure (CHF) is Common- 2% of the population Dangerous- high mortality Disabling- high morbidity Costly- 2% of health care budget Treatable- very successful pharmocological therapy developed Definition of CHF Heart failure (HF) is the inability of the heart to maintain an output adequate to meet the metabolic demands of the body. Definition of HF I. Symptoms and signs of heart failure (at rest or during exercise) and II. Objective evidence (preferably by echocardiography) of Cardiac dysfunction (systolicand/ordiastolic) (at rest) and (in cases where the diagnosis is in doubt) and III. Response to treatment directed towards heart failure *Criteria I and II should be fulfiled in all cases. Pathophysiology of Heart Failure Autonomic and hormonal control of cardiovascular function Pathophysiology of Heart Failure Pathophysiology of Cardiac Performance Cardiac performance is a function of 4 factors PRELOAD AFTERLOAD CONTRACTILITY HEART RATE Preload Diuretics in Heart Failure Loop diuretics: furosemide, torsemide Thiazide and thiazide-like diuretics: hydrochlorothiazide chlorthalidone K+ sparing diuretics: Na+ channel inhibitors: amiloride, triamterene Aldosteron antagonists: spironolactone,eplerenone Diuretics in Heart Failure Loop Diuretics Furosemide, torsemide, ethacrinic acide, torsemide Secreted into the tubular fluid by proximal tubule cells Loop Diuretics: Side Effects and Drug Interaction Volume depletion, hyponatremia, hypokalemia Hypocalcemia, hypomagnesemia, hypochloremia Ototoxicity – especially with ethacrynic acid Hypotension Metabolic effects – hyperuricemia, hyperglycemia, hypercholesterolemia (↑LDL, ↓HDL, ↑TGL) Cardiac glycosides (risk of ventricular arrhythmias) Aminoglycoside antibiotics, cisplatin (risk of ototoxicity) Loop Diuretics: Drug Interaction NSAIDs – reduced effects Probenecid – blocks secretion into the distal tubule and decreases the response to the LD Thiazide Diuretics Hydrochlorothiazide – the prototype for this class of drugs Thiazide-like – chlorthalidone, indapamide and metolazone (long acting diuretics) The same mechanism of action Thiazide Diuretics – Side Effects Electrolyte abnormalities – hypokaliemia, hyponatremia, hypercalcemia, hypomagnesemia, hypochloremia, hypovolemia Hyperuricemia, hyperglycemia (reduced effecacy of hypoglycemic drugs Increased plasma levels of LDL and TGL Sexual dysfunction Cardiac arrhythmias Drug interactions – as loop diuretics Aldosterone Antagonists Aldosterone Antagonists Aldosterone Antagonists Aldosterone Antagonists RALES TRIAL RALES TRIAL Aldosterone Antagonists EPHESUS TRIAL EPHESUS TRIAL EPHESUS TRIAL EPHESUS TRIAL EPHESUS TRIAL EPHESUS TRIAL Cardiac glycosides Cardiac glycosides – mechanism of action Pharmacokinetics (Digoxin, Digitoxin) Highly variable kinetics + VERY narrow therapeutic index = need to individualize dose regiments Relatively long half-lives of elimination accumulation to stedy state loading doses employed delays following changes in therapy Pharmacokinetics Plasma concentration determinations Effective range = 1.0 – 2.5 ng/ml Toxic range = 1.5 – and up Rarely essential to a diagnosis of toxicity Estimate of degree of overdose Can be used to calculate dose adjustments Comparative Pharmacokinetics Toxicity Gastrointestinal (relate to vagal effects) anorexia abdominal discomfort vomiting diarrhea Toxicity Cardiac disturbances premature ventricular depolarization nodal rhytms A – V dissociation Treatment of Toxicity • Stop giving the drug (for a time) • Potassium (if hypokalemic) • Cholstyramine, activated charcoal (to bind digoxin in GI tract and shorten half-life ) • Digoxin Antibodies (Fab fragments) • Antiarrhythmics (very cautiously) • Electrotherapy (defibrillation only in the case of VF Drug Interactions • Increased plasma concentration – verapamil, diltiazem, quinidine, amiodaron, spironolacton • Changes in plasma electrolyte – diuretics, salts (K+, Ca++), adrenocorticoids • Changes in digoxin absorption – antacids, cholestyramine, laxatives, antidiarrheal absorbents • Changes in cardiac cell activity sympathomimetics