* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Renal Disease / Eckel Service Overview
Survey
Document related concepts
Transcript
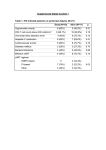
Prashanth Thakker Understand how to accurately diagnose, manage, and treat acute kidney injury Understand the etiology of chronic kidney disease and management of risk factors to reduce progression Manage patients with end stage renal disease by learning about indications for dialysis and common complications in the patient population Hypertension and electrolytes will be discussed at a later date** Get a good history (Baseline) Stop offending agents Treat underlying etiology An acute/abrupt worsening of renal function (<48 hours) ↑ Cr > 0.3mg/dl ↑ Cr >50% from baseline UOP <0.5mL/kg/hr for >6 hours History, history and more history Evaluate the urine for sediment FeNa or FeUrea (Urine Sodium x Plasma Cr)/(Plasma Sodium x Urine Cr) (Urine urea x Plasma Cr)/(Plasma Urea x Urine Cr) Renal Ultrasound Serologies Renal Biopsy History is key (volume, hemorrhage, ACE-I/ARB/NSAID, decreased effective circulatory volume – HF, cirrhosis) BUN/Cr ratio of >20 Urine Osm > 500 osm/kg FeNa <1%, FeUrea <35% Stop agents which could worsen underling azotemia (will discuss exogenous agents) Improve hemodynamics – if renal function improves then diagnostic and therapeutic Systemic Hypotension and… Usually associated with prior limited reserve or a co- existing insult (sepsis, drugs etc.) tubular and microvascular changes leading to tubular damage More than just hemodynamically mediated… Vascular changes in the setting of hemodynamic shift Sepsis/Cytokine induced direct endothelial damage leading to microvascular thrombosis, ROS production etc. renal tubular injury Rhabdomyolysis ATN History – traumatic crush injury, seizures, prolonged immobility Lab findings – elevated myoglobin, CK, UA heme+, low RBC Pathophysiology – renal vasoconstriction, direct tubular injury, and tubular obstr. Treatment – fluids *Hemolysis has a similar mechanism of action TLS (Tumor Lysis Syndrome), Multiple myeloma In TLS you have precipitation of Uric Acid causing tubular injury Severe hypercalcemia can cause significant vasoconstriction and tubular damage Myeloma proteins will precipitate and cause tubular obstruction Antimicrobials Tubular necrosis – amphotericin B, aminoglycosides AIN – PCN, cephalosporins, quinolones, sulfa, rifampin Vancomycin w/ high troughs? Tubular obstruction – acyclovir Direct tubular damage – foscarnet, pentamidine, cidofivir Contrast Induced Nephropathy ATN Serum creatinine rises in the first 24-48 hours, with peak 3-5 days and resolves in 1 week Be weary with patient with underling renal disease!! Pathophysiology involves direct tubular injury, hypoxia to the outer medulla due to occlusion of small vessels, transient tube obstruction Fluids (pre-post), +/- bicarbonate AIN Legionella Tubulointerstitial nephritis uveitis (TINU) syndrome Acute Nephritic Syndromes (to be discussed) TTP/HUS Recent GI disease, use of recent calcineurin inhibitors Atheroembolic Recent vascular manipulation (usually large vessels) Stop offending agents and treat underlying condition!! Rhabdomyolysis – fluids TLS – Allopurinol, Rasburicase Volume overload – salt/water restriction, diurese, ultrafiltration Hyperkalemia – decrease exogenous K+/meds ↑ K+, transient shift, and Kayexelate Metabolic Acidosis – Bicarb if pH <7.2 Hyperphosphatemia – phosphate binders, phosphate restriction DRUG DOSING Classification of CKD 1 (GFR > 90) – Treat underlying condition/comorbidities 2 (GFR 60 – 89) – Estimate Progression of disease 3a (GFR 45-59) – Evaluate + treat complications 3b (GFR 30-44) – Evaluate + treat complications 4 (GFR 15-29) – Prepare for RRT 5 (GFR <15) – HD if indicated Diabetic Glomerular Disease Glomerulonephritis Hypertensive Nephropathy Primary glomerulopathy with HTN (FSGS) Vascular and ischemic renal disease ADPKD Other cystic and tubulointerstitial kidney disease 1. Diabetic Nephropathy (55%) 2. Hypertensive nephropathy v Hypertension due to underlying vascular disease (33%) 3. Glomerulonephritis 4. Polycystic Kidney Disease 5. Obstructive Uropathy Incidence – 40% patients with DM develop diabetic nephropathy Progression usually seen in 5-10 years after DMI (seen as microalbuminuria), 30-300mg/g of albumin/creatinine ratio is considered microalbuminuria Pathophysiology – increased glomerular pressures, glycosylation end products cause vascular disruption, filter barrier disruption, and glomerulosclerosis Management – avoid progression through DM II control, blood pressure control (ACE-I/ARB to reduce intra-glomerular pressure) Uncontrolled HTN can cause permanent damage in 6% of patients with uncontrolled HTN Hypertension is the etiology for 27% of patients with ESRD Malignant hypertension in the setting of scleroderma and cocaine use can complicate the progression of hypertensive nephropathy ACE-I and adequate blood pressure control is the way to go! Nephritic v Nephrotic Nephritic Blood >> Protein 1-2g/day, pyuria, hematuria w/ casts, HTN, fluid retention Nephrotic Protein >> Blood 3.5g/day (definition) for ‘nephrotic range’ proteinuria Nephrotic syndrome ANCA + Vasculitis (Pauci-immune) – (40-45%) Wegener’s, Microscopic Polyangitis, Churg-Strauss Immune Complex Disease (granular) – (40-45%) Post strep GN, MPGN, Fibrillary GN, IgA nephropathy SLE, Cryoglobinemia, Endocarditis, HSP Anti-GBM (linear) - (15%) FSGS (40%) Idiopathic, HIV, heroin, obesity Membranous GN (30%) Idiopathic, HBV, HCV Minimal Change Disease (20%) Idiopathic, NSAIDS Membranoproliferative GN (5%) Infection (HCV, HBV), immune complex Diabetic Nephropathy AL/AA Amyloid Light-chain deposition disease Lupus (WHO class V) ADPKD occurs in 1:400–1:1000 individuals worldwide and accounts for ~4% of end-stage renal disease (ESRD) in the United States via the ADPKD-1 gene (85%)/ADPKD-2 gene Hypertension precedes renal dysfunction Associated complications include hepatic cysts, aortic root/annulus dilation, MVP, AI, Cerebral aneurysms Treatment – HTN management, cyst/Pyelo should be treated with TMP/SMX or fluoroquinolones due to good cyst penetration Potassium Hemostasis Metabolic Acidosis Disorders of Calcium and Phosphate Ischemic Vascular Disease Heart failure, HTN, LVH Anemia Abnormal Hemostasis Calcium x Phos product Calcium containing v non-calcium containing phos binders Calcitriol Osteitis fibrosa cystica Usually starts off as livedo reticularis and then advances to patches of ischemic necrosis Thought to be due to calcification of small-mid sized vessels leading to ischemia and necrosis Associated with high Ca-Phos product > 55 Management includes local wound care, decrease Ca-Phos product Reduction in erythropoietin leads to anemia usually in stage III or stage IV CKD Managed by administration of erythropoietin in conjunction with iron, vitamin B 12, and folate to ensure adequate production by the marrow Progression of CKD or AKI leading to any of the following: A – ACIDEMIA E – ELECTROLYTES (↑ K…↑P, ↑Mg, ↓Ca, ↓Na) I – INGESTION/TOXINS O – OVERLOAD (UF) U – UREMIA (pericarditis/encephalopathy) Continuous Renal Replacement Therapy Intermittent Hemodialysis Continuous Ambulatory Peritoneal Dialysis Continuous Cyclic Peritoneal Dialysis Hypotension Muscle Cramps Anaphylactoid Reaction to Dialysate Type A (IgE-mediated intermediate hypersensitivity reaction) may need steroids and epi Type B non-specific chest and back pain resolve over time Continuous Ambulatory Peritoneal Dialysis Dialysis solution is manually infused into the peritoneal cavity and exchanged 3-5 times a day. Gravity is used to move fluid out of the abdomen Continuous Cyclic Peritoneal Dialysis Dialysis solution is automatically cycled while the patient sleeps Complications Peritonitis (WBC >100/mm3) Non-peritonitis infections Weight gain Hypoprotenimia Etiology of ESRD Route of dialysis (HD or PD) – mostly HD Location and days of HD (last day of HD) Access Nephrologist Dry Weight Review labs closely Review medications and make sure renally dosed Fever Missed Hemodialysis Dyspnea Hyperkalemia Vascular Access Chest Pain Usually due to line infection, check all access sites! (other etiologies include HCAP, skin infection, C. dif) Cultures peripheral + HD line Review prior cultures including MIC (to see if they are building resistance) Empiric Treatment Cover gram positives for line infection. Gram negatives are covered if there patient is noted to be fairly ill. Vancomycin 20mg/kg load, followed by 10mg/kg post HD Zosyn 2,25q8h (HCAP), 2.25q12 otherwise Gentamicin is also an excellent choice given with HD Volume overload Coordinate ultrafiltration with HD unit Make sure patient has access, if no access and HD stable can wait for IR to place a line OR if there is concern for respiratory instability patient should go to MICU for temporary HD line placement (at this time it would be coordinated with renal MICU fellow) Hyperkalemia Temporary measures include insulin/D50, Sodium Bicarbonate, Albuterol. You can stabilize the cardiac membrane with calcium gluconate or chloride. Potassium binding agent in the GI tract kayexalate can be used Keep you senior and renal fellow informed as patient may need HD sooner than you think! Important to get history regarding last proper use. It is also important to examine the patient to look for thrill/bruit any signs of functionality of the graft or fistula Contact Vascular Surgery if there is any concern for thrombosis and need for declottication Again, urgent HD will always require the MICU Mr. G is a 65 year old male with a past medical history of CHF presenting with worsening dyspnea on exertion and orthopnea. Patient notes a 30lb weight gain over the last month and significant lower extremity edema. He takes Lasix, Metoprolol Succinate, Lisinopril, Aspirin, and Spironolactone. Patient is afebrile, blood pressure of 140/90, heart rate 105. Patient is warm and wet with an elevated JVP and significant +3 lower extremity edema. His labs are consistent with a creatinine of 2.9 with a baseline of 1.2. What do you want to do you think the etiology of the renal dysfunction is in this patient and what would your plan be? Kasper DL, Harrison TR. Disorders of the Kidney and Urinary Tract. In: Harrison's Principles of Internal Medicine. New York: McGraw-Hill, Medical Pub. Division; 2005. Armitage KB et al. Case Approach: A Resident Guide to Internal Medicine at UH Case Medical Center and the Cleveland VA 2016-2016. Cleveland: Case Medical Center; 2015. Sabatine MS. Renal Failure. In: Pocket Medicine. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011.