* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Acute Interstitial Nephritis
Survey
Document related concepts
Transcript
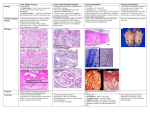
Tubulointristitial Nephritis Dr. Hamed Shakhatreh Consultant nephrologest Head of nephrology department,Al-basher hospital. M.O.H Primary interstitial nephropathies make up a diverse group of diseases that elicit interstitial inflammation associated with renal tubular cell damage. Traditionally, interstitial nephritis has been classified morphologically and clinically into: acute and chronic forms. Acute Interstitial Nephritis 70% Drug hypersensitivity 30% Antibiotics: PCNs (Methicillin), Cephalosporins, Cipro Sulfa drugs NSAIDs Allopurinol... 15% Infection Strep, Legionella, CMV, other bact/viruses 8% Idiopathic 6% Autoimmune Dz (Sarcoidosis, Tubulointerstitial nephritis/Uveitis) Drug Causes of AIN Antibiotics Cephalosporins, Ciprofloxacin, Ethambutol, Isoniazid, Macrolides, Penicillins, Rifampin, Sulfonamides, Tetracycline, Vancomycin NSAIDs Almost all agents, including selective COX-2 inhibitors Diuretics Furosemide, Thiazides, Triamterene Miscellaneous Acyclovir, Allopurinol, Amlodipine, Azathioprine, Captopril, Carbamazepine, Clofibrate, Cocaine, Diltiazem, Famotidine, Indinavir, Mesalazine, Omeprazole, Phenteramine, Phenytoin, Pranlukast, Propylthioruacil, Quinine, Ranitidine AIN from Drugs Renal damage is NOT dose-dependent May take weeks after initial exposure to drug More common is seen several months to a year after use But as early as 1 week after medication is begun Fever (27%) Serum Eosinophilia (23%) Maculopapular rash (15%) Bland sediment or WBCs, RBCs, non-nephrotic proteinuria WBC Casts are pathognomonic! Urine eosinophils on Wright’s or Hansel’s Stain Also see urine eos in RPGN, renal atheroemboli Leukocytoclastic vasculitis Interstitial nephritis Acute allergic IN- presents with fever, maculopapular rash, arthralgia, eosinophilia with use of certain drugs or systemic infection UA_ microscopic hematuria, pyuria, non nephrotic proteinuria, eosinophiluria Usually resolves after d/c of offending drug and steroids Clinical Presentation AIN of any cause Nausea Vomiting Malaise Drug-Induced AIN •Rash •Fever •Eosinophilia •Triad 15% 27% 23% 10% Laboratory Manifestions Acute rise in plasma creatinine concentration Eosinophilia and eosinophiluria Urine sediment: wbcs, rbcs, white cell casts Proteinuria (< 1 g/day) Infectious Causes of AIN Bacterial Corynebacterium diphtheriae, Viral legionella, staphylococci, streptococci, yersinia CMV, EBV, HIV, HCV, HSV, hantaviruses, mumps, polyoma virus Other Leptospira, mycobacterium, mycoplasma, rickettsia, syphilis, toxoplasmosis Acute bilateral pyelonephritis Flank pain, toxic, febrile U/A : pyoria, hematuria, proteinuria, bacteriuria B/C & U/C help to diagnosis Infiltrative/Autoimmne Causes of AIN Sarcoidosis Sjogren’s Syndrome Leukemia Lymphoma Systemic lupus erythematosus TINU SYNDROME Acute Kidney Injury Prerenal Hypovolemia Decreased cardiac output Renal vasoconstriction Intrinsic Acute Tubular Necrosis Glomerulonephritis Vascular disorders Postrenal Bladder Neck Ureteral Tubular Renal biopsy Indications Uncertainty of diagnosis Advanced Lack renal failure of spontaneous recovery following removal of offending drug Treatment Discontinuation of offending agent Corticosteroids Prednisone 1 mg/kg to a max of 40-60 mg x 1-2 weeks IV Methylprednisolone 0.5 – 1 g/day x 3 days AIN PROGNOSIS Most patients recover full kidney function in 1 year Poor prognostic factors AKI > 3 weeks Advanced age at onset Chronic Tubulointerstitial Disease chronic interstitial nephritis (CIN) follows a more indolent course and is characterized by tubulointerstitial fibrosis and atrophy associated with interstitial mononuclear cell infiltration. Over time, glomerular and vascular structures are involved, with progressive fibrosis and sclerosis within the kidney Causes of chronic interstitial nephritis Toxins( analgesic nephropathy, lead nephropathy) Infection (chronic pyelonephritis) Autoimmune( Sjogren syndrome, SLE, renal rejection) Metabolic( hyperuricemia, hypercalcemia) Radiation Neoplastic infiltration( leukemia, lymphoma, multiple myeloma) Hereditary renal diseases(ADPKD,MCD,MSK) Analgesic abuse nephropathy chronic interstitial nephritis Result from excessive consumption (NSAID & Aspirin) Dose dependent (at least 1 kg) Being responsible for 1% to 3% of ESRD cases Bacterial infection bacterial infection of the renal parenchyma causes interstitial nephritis infection without anatomical abnormality seldom produces permanent damage obstruction (stones, prostate etc) in combination with infection can cause progressive disease tuberculosis causes extensive destruction from granulomata, fibrosis and caseation At first, interstitial edema and PMN infiltration, then formation of irregular abscesses and eventually scars Risk factors: diabetes mellitus obstruction delayed antimicrobial therapy severe infection with ATN reflux nephropathy papillary necrosis Urinary tract obstruction Consequences of urinary tract obstruction Reduced glomerular filtration rate Reduced renal blood flow (after initial rise) Impaired renal concentrating ability Impaired distal tubular function Nephrogenic diabetes insipidus Renal salt wasting Renal tubular acidosis Impaired potassium concentration Reduced RBF leads to renal ischemia tubular atrophy Phase A Phase B Intraluminal pressure RBF GFR ... due to ... due to ... due to obstruction h Peristalsis Vasodilation h Intratubular pressure Prostacyclin Prostraglandi n E2 ... due to ... due to ... due to Disorganised peristalsis dilation of tubules and ureter Vasoconstricti on Angiotensin II Thromboxan e A2 Continuing obstruction vasoconstrict ion Acute urinary tract obstruction Functional consequences Ureteric and tubular pressure Renal blood flow (RBF) GFR 0 6 Hours 12 baseline 18 myeloma Bence-Jones protein (light chains from malignant plasma cell clone) causes interstitial nephritis, tubular obstruction(cast nephropathy) and amyloid deposition Myeloma kidney :the classic pathologic include THP+LC casts in dilated, atrophic distal tubuls with infiltration monocyte & macrophage & plasma cells that produce giant cells LCs are nephrotoxic through direct injury of tubular epithelial cells & intrarenal obstruction from cast formation Predisposing factors: LC concentration LC isoelectric point intraluminal PH tubular flow rate presence of Tamm-Horsfall Pr Hypercalcemic Nephropathy Chronic hypercalcemia is seen in Hyperparathyroidism Sarcoidosis Multiple myeloma Vitamin D toxicity Metastasis bone disease Hypercalcemia decrease GFR through renal vasoconstriction Calcium deposition in distal nephron and interstitial that leads to mononeuclear cell infiltration and tubular necrosis Defective concentration ability, poliuria, nocturia Nephrocalcinosis & nephrolitiasis WBC Casts Cells in the cast have nuclei (unlike RBC casts) Pathognomonic for Acute Interstitial Nephritis Match: 1. hyaline casts 2. muddy brown casts 3. RBCs 4. RBC casts 5. Oval fat bodies 6. eosinophils A. ATN B. prerenal azotemia C. glomerulonephritis D. nephrolithiasis E. interstitial disease F. nephrotic syndrome THANK YOU