* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download the adrenal cortex
Polycystic ovary syndrome wikipedia , lookup
Mammary gland wikipedia , lookup
Xenoestrogen wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Vasopressin wikipedia , lookup
Neuroendocrine tumor wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
Breast development wikipedia , lookup
History of catecholamine research wikipedia , lookup
Hypothalamus wikipedia , lookup
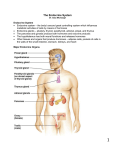
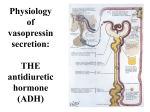
Endocrine Problems Gail L. Lupica PhD, RN, CNE Nurs 211 The Endocrine System Although the nervous system is the dominant controlling influence over the activities, and responses of the body; There is a secondary mechanism in place where one cell can influence the function of other cells, or target organs. This occurs through the secretion or inhibition of hormones into the bloodstream= The Endocrine System The cells and glands of the endocrine system each have very specific functions and coordinate with other cells to create an environment conducive to the survival of the total organism. The Diseases We’re Going to Look At Anterior Pituitary: • Hypersecretion of ACTH= Cushing’s Disease (neoplasm of gland) • Hypersecretion of Growth Hormone = Giantism • Hypersecretion of Growth Hormone = Acromegaly Posterior Pituitary: • Hypersecretion of ADH=SIADH Posterior Pituitary: • Hyposecretion of ADH= DI The Diseases We’re Going to Look At Adrenal Cortex: • Insufficient secretion= Addison’s Disease Adrenal Cortex: • Acute adrenal insufficiency=Adrenal Crisis Adrenal Cortex: • Hyperfunction= Cushing’s Syndrome Adrenal Medulla • Hyperfunction=Pheochromocytoma Pituitary Disorders The pituitary gland plays a vital role in the body’s ability to maintain homeostasis. Pituitary disorders involve an excess or deficiency in one or more of the pituitary hormones. The Hypothalamus controls many Pituitary functions. It signals to the pituitary to release or inhibit hormone secretion. The Pituitary gland (hypophysis) Anterior (6 hormones are secreted by the anterior pituitary) 1. ACTH: regulates secretion of adrenal hormones (increases in response to stress) 2. Growth hormone: has no specific target organ.(promotes growth of bone/cartilage etc…) 3. Thyroid stimulating Hormone OB… 4. Follicle Stimulating Hormone: testes/ovaries 5. Luteinizing Hormone: testes/ovaries 6. Lactogenic Hormone (Prolactin): breast dev/lactation The Pituitary gland (hypophysis) Posterior (these hormones are synthesized in the hypothalamus And stored in the posterior pituitary) 1. Anti-diuretic hormone (ADH): renal distal tubules become more permeable to water, causing a reabsorbtion (also has a vasopressor effect in high doses) (alcohol inhibits ADH secretion) 2. Oxytocin: uterine/lactation/fertilization 3. Melanocyte stimulating Hormone THE ADRENAL CORTEX: • Regulation of Adrenal hormones is accomplished through Adrenocorticotropic hormone (ACTH, which is produced by the anterior pituitary gland) – (Aldosterone secretion is primarily accomplished through the R-A-A system THE ADRENAL CORTEX…: • Is responsible for secretion of three major groups of steroid hormones: Mineralocorticoids (aldosterone): maintains sodium, and fluid balance Glucocorticoids (cortisol): provide the body with the materials needed for energy; proteins, fats, glucose, water Androgens (testosterone): hyper secretion can cause masculinizing changes Adrenals Adrenal glands are located just above each kidney. 1. Adrenal cortex 2. Adrenal medulla Although housed together, they are separate organs in physiologic function. The adrenal medulla is surrounded by the adrenal cortex. Adrenal medulla Produces and Secretes catecholamines 1. Epinephrine 2. Norepinephrine Cushing’s disease Cushing’s syndrome Hypersecretion of ACTH. (disease) Hypersecretion of ACTH by the anterior pituitary-causes increased release of both cortisol and androgenic hormones Hypersecretion of Cortisol. (syndrome) … too much cortisol secreted by the adrenal cortex organ itself Cushing’s- clinical manifestations serum glucose levels increased ….(gluconeogenesis) eventually the islet cells of the pancreas cannot produce enough insulin and DM results. Loss of protein stores occurs, muscle wasting Humoral immunity is reduced, decreasing the threshold to infection Skin tissues lose collagen, and become very thin: tearing and bruising easily Cushing’s disease Cushing’s syndrome Excess body and facial hair growth in women (from excess androgen secretion) Mood swings and psychosis may occur as the effect of excess cortisol on cognitive function. Truncal obesity: results from the mobilization of fat in the lower parts of the body, to the trunk causing the abdomen to become protuberant as the extremities become thin and wasted. Cushing’s disease Cushing’s syndrome Purple striae: appear on the abdomen as a result of the stretching of the abdominal skin. They’re purple due to the collagen deficit in the tissues. Round facial features: fat accumulation around the neck and cervical area is termed the buffalo hump. 3/4/10 Cushing’s management Return cortisol levels to normal! So must determine the underlying cause of the hypersecretion. Surgery to remove neoplasms. Physical therapy to improve muscle strength. Cushing’s Nursing Diagnoses Risk for Infection R/T impaired immune response and tissue repair Risk of Altered Health Maintenance R/T insufficient knowledge of disease process Body Image Disturbance Risk for Fluid and Electrolyte imbalance Critical Thinking 1. 2. 3. Explain to your patient why they can get Cushingoid features from too much steroids, from a tumor on their anterior pituitary OR from hypersecretion from the adrenal cortex. What causes all the excess hair growth and acne on the patient with Cushingoid features? What mechanism/feedback loop activates aldosterone secretion from the adrenal cortex? Under what circumstance(s)? Hyper secretion of Somatotropin (Growth Hormone) ACROMEGALY rare condition. • Excess secretion of somatotropin affects all actively growing cells. • It is characterized by an increase in connective tissue, cartilage, and soft tissue, and by growth and thickening of the bones in the hands feet and face. • Glucose metabolism is altered and patients develop secondary DM. • Urinary excretion of Na+, K+, and phosphorous decreases so fluid retention is a problem. Hyper secretion of Somatotropin (Growth Hormone) ACROMEGALY o Neurologic changes o Headaches o Slow changes in appearance. o Enlargement of ears, nose, and circumference of chest. o Arthritic changes in the joints of the long bones and spine. o Muscle weakness, osteoporosis. • ACROMEGALY o Mandibular growth produces projection of lower jaw. o Hands and feet become wide o Soft tissue changes. o Cardiomegaly. • Diagnosis: o H&P, elevated serum growth hormone levels • Treatment: o Surgery o Somatostat Hyper secretion of Somatotropin (Growth Hormone) GIGANTISM • Hypersecretion of Growth Hormone (GH) occurs before puberty…before closure of growth plates. • Growth proportional growth in the length of all bones occurs. Diabetes Insipidus ADH is synthesized in the hypothalamus and stored in the posterior pituitary 1. ADH: renal distal tubules become more permeable to water, causing a reabsorbtion (also has a vasopressor effect in high doses) (alcohol inhibits ADH secretion) Diabetes Insipidus (DI) Anti diuretic hormone is suppressed from the post pituitary. The patient therefore diureses. What will you see? 1. Copious urine output! 2. High serum sodium > 145 Why? 3. Low urine specific gravity 1.001-1.005 Why? What kind of problems do you think would prompt this? DI- treat, Nsg Dx Treat underlying cause May give exogenous ADH (nasally, IV, po) Give IV fluid resusitation/replacement I&O What is your PRIMARY Nursing Diagnosis? Syndrome of Inappropriate Antidiuretic hormone (SIADH) Occurs when there is over secretion of ADH from the posterior pituitary ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH ADH SIADH 1. 2. 3. 4. What will you see? The body is NOT diuresing. Therefore fluid is reabsorbed into the vascular space Pt will be oliguric. Serum sodium will be very low (< 135). Why? Specific gravity of urine will be high. Why? (Pt suffers from symptoms of a dilutional hyponatremia) Anterior Pituitary Disorders/ TUMORS • TUMORS are the most common cause of primary (anterior) pituitary disorders. • The most common manifestation is headache. …visual disturbances due to the expansion of the mass on the optic nerve. • The pituitary hormones may hyper secrete or hypo secrete hormones. Anterior Pituitary Disorders/ TUMORS TREATMENT • Transphenoidal microsurgery is an approach through the mouth, and along the floor of the nasal passage. • The dura mater is incised and the abnormal tissue is identified and removed. To prevent CSF leakage, the dura mater may be patched with a piece of fascia, or muscle taken from the leg. Transphenoidal microsurgery • Pre-op • Teach- Can’t sneeze, blow nose, cough, bend over. TREATMENT Transphenoidal microsurgery • Post-op ASSESS neoro staus q1h x 24h , then q4 • The nose is packed and a gauze dressing or sling is worn under the • Prophylactic antibiotics o Diabetes Insipidus o The patient may need lifelong hormone replacement therapy. o Monitor nasal drainage for HALO sign TREATMENT Transphenoidal microsurgery o Post-op nursing care is aimed at measures that reduce ICP. o Patient’s suture line is at the junction of the gums and upper lip. Patients must avoid trauma to the suture line- (Use a foam toothette, instead of a bristled brush.) Adrenocortical Insufficiency=Addison’s disease • Clinical Manifestations: Skin color changes occur: hyperpigmentation due to uninhibited ACTH release from the anterior pituitary. Muscle weakness& fatigue Hypotension Nausea, vomiting, weight loss, diarrhea Loss of hair Hypoglycemia • 3/4/10 Adrenal crisis (Addisonian crisis, acute adrenal insufficiency) • A sudden decrease or absence of adrenocortical hormones. • Often occurs when a person is exposed to major stresses, such as trauma, infection, surgery, or major illness. (May be due to hemorrhage, infection, or infarction within the adrenal gland itself) Adrenal crisis (Addisonian crisis, acute adrenal insufficiency) • Clinical Manifestations: Severe dehydration Weakness Confusion Decreased sodium reabsorption, and increased potassium retention Circulatory deterioration Hypovolemic shock: sodium, water, and chloride are excreted in great amounts Cardiac dysrhythmias • Adrenal crisis (Addisonian crisis, acute adrenal insufficiency) • Management: Fluid replacement: Isotonic dextrose and saline Parenteral Dextrose IV Hydrocortisone Monitor serum glucose, electrolytes Hemodynamic and cardiac monitoring • Eventual hormone replacement Adrenal Medulla - Pheochromocytoma The function of the adrenal medulla is to produce and secrete catecholamines. Epinephrine-80% (heart, BMR) Norepinephrine-20% (also secreted by the sympathetic nerve terminals; arteriole vasoconstriction) Pheochromocytoma They are rare adrenal medullary tumors whose primary clinical manifestations is that of hypertension. They produce and secrete excessive quantities of epinephrine and norepinephrine into the bloodstream. The individual remains in a fight or flight state. Pheochromocytomaclinical manifestations Arterial Hypertension Excessive perspiration Palpitations Headaches Hyperventilation Flushing Later: Cardiomegaly, LV failure, CHF Pheochromocytoma o o o o H&P Urinary catecholamines Elevated blood glucose levels CT, MRI of tumor o Diagnosis Management Surgical excision of tumors Pheochromocytoma Pre-op Stimulant free diet Bedrest Regitine (alpha adrenergic blocker) and/or Minipress Inderal Post op Monitor for Hypovolemic shock caused by rapid relaxation of constricted blood vessels! Monitor for transient hypertensive episodes! PheochromocytomaNursing Diagnoses Risk for altered systemic tissue perfusion R/T fluctuations in CV status Anxiety R/T increased circulating catecholamines Altered Nutrition R/T increased metabolic rate Risk for Altered health Maintenance R/T insufficient knowledge of follow up care.