* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The Surgical Anatomy of the Perforating Branches of the Basilar Artery
Survey
Document related concepts
Transcript
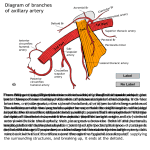
31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Neurosurgery Issue: Volume 33(1), July 1993, p 80–87 Copyright: Copyright © by the Congress of Neurological Surgeons Publication Type: [Surgical Anatomy] ISSN: 0148396X Accession: 0000612319930700000012 Keywords: Anatomy, Basilar artery, Brain stem, Cerebral artery, Cerebrovascular occlusive disease, Perforating artery [Surgical Anatomy] The Surgical Anatomy of the Perforating Branches of the Basilar Artery Marinkovic, Slobodan V. M.D., D.Sc.; Gibo, Hirohiko M.D., D.Sc. Author Information Institute of Anatomy, School of Medicine, University of Belgrade, Belgrade, Yugoslavia (SVM) and Department of Neurosurgery, Shinshu University, School of Medicine, Matsumoto, Japan (HG) Reprint requests: Hirohiko Gibo, M.D., Department of Neurosurgery, Shinshu University, School of Medicine, 311 Asahi, Matsumoto 390, Japan. Received, September 14, 1992. Accepted, February 9, 1993. ABSTRACT THE PERFORATING BRANCHES of the basilar artery were examined in 14 brain stems injected with india ink or methylmethacrylate. Three groups of the perforators were distinguished: the caudal, the middle, and the rostral. The caudal perforators varied in number from two to five and in diameter from 80 to 600 µm. In addition to their terminal branches, which entered the foramen cecum, the perforators occasionally branched off the pontomedullary artery, the pyramidal vessels, and the hypoglossal branches. The middle perforators arose either separately from the basilar artery or along with the basilar artery collateral branches. They ranged in number from five to nine and in diameter from 210 to 940 µm. The perforators gave rise to the pontomedullary artery (8.3%), the long pontine arteries (25.0%), and the anterolateral vessels (100%). The rostral perforators originated from the terminal part of the basilar artery (91.6%), as well as from the superior cerebellar artery (91.6%) and the posterolateral artery (16.6%). They varied in number from one to five and in diameter from 190 to 800 µm. The anastomoses among various perforating vessels were noted in 41.6 to 66.6% of the cases. The authors discussed the possible clinical significance of the anatomical data observed in this study. The perforating branches of the anterior cerebral, anterior communicating, middle cerebral, internal carotid, anterior choroidal, posterior communicating, and posterior cerebral arteries have been examined by many authors, including the authors from our laboratory (7,10–12,15,17,20–22,24–32,34,35,37,42,43). In regard to the perforators of the basilar artery (BA), however, they have not yet been examined in detail. In the last seven decades, to our knowledge, only a few publications appeared that only partially deal with the BA perforators (7,9,12–14,21,23,39). In these articles, not all of the microanatomical data can be found that are necessary for safe neurosurgical operations in the prepontine and interpeduncular cisterns, as well as for an understanding of certain syndromes that follow occlusions of the BA perforators (5,8,13,16). For these reasons, we decided to undertake a detailed study of the perforating branches of the BA. MATERIALS AND METHODS http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 1/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. The perforating arteries were examined in 14 brain stems. The brains were very carefully removed from the skull, in order to avoid damage to the brain stems, as well as to the vertebral arteries and BA. In each brain, plastic catheters were put in both vertebral arteries after ligation of the posterior communicating arteries. After perfusion with isotonic saline solution, the vertebrobasilar arterial system of 12 brain stems was injected with a 10% mixture of india ink and gelatin. After fixation in 10% formaldehyde solution for 3 weeks, microdissection of the perforating arteries was performed under a stereoscopic microscope. The arterial system of the remaining two brain stems was injected with methylmethacrylate to obtain the vascular casts. We have used for the statistical analysis only those specimens injected with india ink, that is, 12 brain stems. The vascular casts of the two remaining brain stems were excluded from the statistical analysis. RESULTS The BA gave rise to many side (collateral) branches, which can be divided into three groups: the cerebellar arteries, the large pontine vessels, and the perforating arteries. The latter arteries often branched off the anterolateral branches (Fig. 1). http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 2/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 1. The collateral branches of the BA, which were divided into the cerebellar arteries (striped), the large pontine arteries (white), and the perforating arteries (black). Note the anterolateral arteries (dotted). 1, the vertebral arteries; 2, the BA; 3, the caudal perforating artery; 4, the middle perforating artery; 5, the rostral perforating artery; 6, the pontomedullary artery; 7, the AICA; 8, the inferolateral pontine artery; 9, the superolateral pontine artery; 10, the posterolateral artery; 11, the SCA; 12, the right posterior cerebral artery; 13, the oculomotor nerve; 14, the crus cerebri; 15, the trigeminal nerve; 16, the pons; 17, the abducent nerve; 18, the facial and vestibulocochlear nerves; 19, the glossopharyngeal nerve; 20, the vagus nerve; 21, the accessory nerve; 22, the hypoglossal nerve; 23, the olive; 24, the pyramid; 25, the anterior median sulcus of the medulla, and the anterior spinal artery. The cerebellar arteries comprise the posterior inferior cerebellar artery, the anterior inferior cerebellar artery (AICA), and the superior cerebellar artery (SCA). The posterior inferior cerebellar artery arose from the BA in 25.0% of the brain stems. The AICA originated from the proximal half of the BA in 91.6%of the specimens. The SCA extended from the terminal part of the BA in all of the cases examined. The large pontine arteries comprise the pontomedullary artery, the posterolateral artery, and the long lateral pontine arteries (Fig. 1). The pontomedullary artery most often originated from the initial part of the BA and terminated in the retroolivary fossa of the medulla (Fig. 1). The posterolateral artery arose from the terminal part of the BA, just caudal to the SCA (Fig. 1). Finally, the long pontine arteries arose from the distal half of the BA and terminated close to the trigeminal nerve (Fig. 1). Commonly, two of them were present on each side of the brain stem: the rostral (superolateral) and the caudal (inferolateral) long pontine arteries (Fig. 1). The perforating branches originated directly from the BA (Fig. 1) but also occasionally from its collateral branches. The perforators varied in number from 10 to 17 per BA (mean, 12.9) (Table 1). They ranged in diameter from 80 to 940 µm (mean, 391.6 µm) (Table 1). According to their position, origination, course, branching pattern, relationships, the site of penetration, and the region of supply, the perforating branches of the BA can be divided into three groups: the caudal, the middle, and the rostral. Table 1. Characteristics of the Perforators of the Basilar Artery The caudal perforating arteries The caudal arteries (Figs. 1 and 2) arose from the initial part of the BA, between the junctional site of the vertebral arteries and the origin sites of the AICA. They arose from the dorsal surface of the BA, descended along the basilar sulcus, and then entered the foramen cecum, which is located at the junctional point of the pontomedullary sulcus and the anterior median sulcus (Figs. 1 and 2). http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 3/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 2. The caudal group of the perforating arteries (black). The individual perforator (1) arises from the AICA (2). The smaller common trunk (3), arising from the BA (4) (cut), gives off the individual arteries to the foramen cecum (5). The larger common trunk (6) branches off the pontomedullary artery (7), a twig to the foramen cecum, the twigs to the anterior median sulcus (8), the pyramidal branch (9), and the hypoglossal branch (10). 11, the right hypoglossal nerve; 12, the vertebral arteries (cut); 13, the abducent nerve. The caudal perforators ranged in number from two to five per BA and in diameter from 80 to 600 µm (Table 1). They averaged 1.7 in number on both the right and left sides. An absence of perforators was seen in 8.3% on the left side. In this case, a large common trunk of the perforators was noted on the opposite side. The caudal perforators originated as the individual vessels or by their own common trunks. The individual perforators ranged in number from zero to four per BA and in diameter from 80 to 350 µm (Table 1). The individual arteries were absent in 33.3% on the right side and in 41.6% on the left side of the brain stem. The common trunks existed in 66.6% on the right and in 75.0% on the left. The diameter of the common trunks varied from 250 to 600 µm (Table 1). The common trunks branched off into the individual vessels, usually before entering the foramen cecum (Fig. 2). The caudal perforators almost always originated from the BA. In addition to this, one or two of them were noted to arise from the AICA (8.3% on the right and 16.6% on the left), as the collateral branches of the pontomedullary artery or by the common stem with the same artery (33.3% on the right and 8.3% on the left) (Fig. 3), by a common trunk with a perforator from the middle group (8.3% on the left side only), and as the collateral branches of the PICA or of the common trunk of the posterior inferior cerebellar artery and the AICA (8.3% on each side). http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 4/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 3. The large common stem (1) of the caudal perforators arises by a short common trunk (2) with the left pontomedullary artery (3). 4, the foramen cecum; 5, the BA, displaced to the right; 6, the left AICA; 7, the left vertebral artery. In most of the cases, one or two caudal perforators originated between the level of the vertebral artery and the AICA (Figs. 2 and 3). In two hemispheres only (16.6%), one of the perforators arose at the level of the AICA, and in another two hemispheres, the perforator arose from the border between the BA and the vertebral artery. In addition to the terminal branches entering the foramen cecum, the caudal perforators also gave rise to the collateral branches in 58.3% of the brains. Thus, they branched off the pontomedullary artery in 25.0% on the right side and in 16.6% on the left side. The anterolateral branches arose from the caudal perforators in 8.3% on the right and in 16.6% on the left; some of these branches penetrated the abducent nerve. Certain caudal perforators, after giving off branches to the foramen cecum, gave off three kinds of branches over the ventral surface of the medulla (Fig. 2): first, the pyramidal branches that arose from the perforators in 33.3% on the right and in 25.0% on the left; second, the twigs to the rostral part of the anterior median sulcus of the medulla, which were seen in 16.6% on the right and in 8.3% on the left; finally, large branches to the hypoglossal nerve, either ipsilaterally (Fig. 2) or bilaterally. The latter branches coursed transversely across the pyramid to reach the rostral rootlets of the hypoglossal nerve. The hypoglossal branches existed in 16.6% on the right and in 33.3% on the left side. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 5/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. It should be mentioned that, in some cases, the complex perforating branches were present, such as those that gave rise to two, three, or even four different collateral branches. The complex branches were present in 25.0% of the hemispheres. Some of the complex arteries gave rise to the pontomedullary, pyramidal, and hypoglossal branches (Fig. 2). Anastomoses were present in 50.0% of the brains. They varied from one to three in number per brain and between 110 and 210 µm in diameter (mean, 145.6 µm). The anastomotic channels were most often (33.3%) noted between the caudal and the middle perforators of the BA. They were seen in 16.6% between the caudal perforators of the BA and the perforators of the vertebral or the anterior spinal arteries. The anastomoses were rarely (8.3%) noted among the caudal perforators themselves. The middle perforating arteries The middle perforating arteries originated from the middle part of the BA, that is, between the origin sites of the AICA and the posterolateral artery (Figs. 1 and 4). They arose from the dorsal surface of the BA, i.e., from the right and the left halves of that surface. The most caudal perforators of the middle group descended along the basilar sulcus or its edges, and the most rostral ones ascended along the same sulcus. The other perforators were often curved or tortuous. Their branches were often twisted around each other, but soon they took a radial course (Fig. 5). They most commonly entered the edges of the basilar sulcus. Figure 4. The middle group of the perforating arteries (black). 1, the foramen cecum; 2, the BA (cut); 3, the pontomedullary artery; 4, the AICA; 5, an anterolateral artery; 6, the common trunk of a middle perforator and the inferolateral pontine artery; 7, a large middle perforator, which gives rise to the superolateral pontine artery; 8, a middle perforator arising from the inferolateral artery; 9, a middle perforator originating from the origin site of the superolateral artery; 10, the SCA; 11, the posterior cerebral artery. The arrow indicates a common trunk of a middle perforator and an anterolateral artery. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 6/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 5. Two common trunks (1 and 2) of the middle perforating arteries arising very close to the left inferolateral (3) and the superolateral (4) pontine arteries (cut). Note the lower common trunk (2) giving off several individual vessels (arrows). 5, the BA slightly rotated to the right; 6, the basilar sulcus; 7, the left part of the ventral surface of the pons. The middle perforators were always present on both the right and the left sides (Fig. 4). They varied in number from five to nine per BA and in diameter from 210 to 940 µm. The perforators originated by the common trunks or as individual vessels. The common trunks, which were always present (Figs. 4 and 5), averaged 529.8 µm in diameter and 4.3 in number. The individual vessels ranged in caliber from 210 to 420 µm (Table 1). They were present in 66.6% on the right and in 8.3% on the left. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 7/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. In 25% of the brains, all of the middle perforators arose from the BA. In the remaining cases, some of them originated in relation to the other branches of the BA. Thus, they arose from the AICA in 16.6%, either from its initial part or the origin site. With the same frequency (16.6%), they were seen to arise in common with the pontomedullary artery. In 25% of the hemispheres, one or two of the perforators arose from the origin site of a long pontine artery (Figs. 4, 5, 6, 7, 8, 9) or from its initial part (Fig. 4, 5, 6, 7, 8). One or more perforators originated by the common trunks with the long pontine arteries in 33.3% of the hemispheres (Fig. 4, 5, 6). The common stems with the anterolateral arteries were seen less frequently (25%) (Fig. 4). Very rarely (8.3% each), the perforators arose in common with the posterolateral artery or with a perforator from the caudal group. Figure 6. A large common trunk (1) of the middle perforators shares the same origin site (arrow) with the inferolateral pontine artery (2). 3, the BA; 4, the left superolateral pontine artery; 5, the left part of the ventral surface of the pons; 6, the left AICA; 7, the left vertebral artery. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 8/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 7. The anastomotic channel (arrow) between a branch (1) of a middle common trunk (2) and an individual perforator (3) arising from the right AICA (4). 5, the BA; 6, the rootlets of the right abducent nerve. Figure 8. The lateral view of the BA (1), the distal segment (2) of the right posterior cerebral artery, and a common trunk (3) of the middle perforators. The common trunk gives rise to the long and short intrapontine branches (arrows). 4, a rostral perforating branch of the BA. The right SCA was cut. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 9/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 9. Three rostral perforating arteries (1, 2, and 3). One of them (1) represents a common trunk that arises from the BA (4) (cut). One of the individual arteries (2) originates from the SCA (5), and another one (3) arises from the posterolateral artery (6). 7, the interpeduncular fossa; 8, the left oculomotor nerve; 9, the posterior cerebral artery (cut); 10, the left crus cerebri; 11, the left mamillary body; 12, the pituitary stalk (cut); 13, the optic chiasm. As already mentioned, the majority of the perforators arose from the BA between the origin sites of the AICA and the posterolateral artery (Fig. 4). In only 16.6% of the hemispheres, they originated at the level of the AICA, and in 25%, they originated below that level. The shortest distance between the origin sites of the AICA and the nearest perforator ranged from 0.9 to 5.6 mm (mean, 2.7 mm). The perforators were never seen to arise rostral to the posterolateral artery. After taking their origin, the middle perforating vessels coursed caudally or rostrally and gave rise to the collateral and terminal branches. Various types of the collateral branches can be identified. The frequency of their origination from the perforating arteries varied considerably. Thus, the pontomedullary artery arose from the perforators in 8.3% only (Fig. 4), and the long pontine arteries originated from the perforators in 25% of the hemispheres (Fig. 4, 5, 6, 7). On the other hand, one or more perforators gave rise to the anterolateral branches in all of the cases examined (Fig. 4). These branches ranged in number from one to three per perforating artery and in diameter from 190 to 580 µm (mean, 318 µm). The caudal anterolateral arteries were in close relationship to the abducent nerve. They not only took part in supplying blood to it, but they also penetrated that nerve in 16.6% of the hemispheres (Fig. 4, 5). The complex arteries often existed within the middle group of the perforators (Fig. 4). Thus, they were seen in 41.6% on the right side and in 58.3% on the left side. The complex arteries usually consisted of a perforating artery, an anterolateral vessel, and a branch to the sixth nerve or a long pontine artery. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 10/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Anastomoses existed in 66.6% of the hemispheres, but only one or two of them were present in the same brain. They were most often found between the middle and caudal perforating arteries (33.3%) (Fig. 7). Anastomoses between the two adjacent middle perforators were seen in 25% of the hemispheres. Rightleft anastomoses, as well as vascular connections between the rostral and middle perforators, rarely existed (16.6%). The terminal branches of the middle perforators penetrated the edges of the basilar sulcus. They divided into the long and short intrapontine branches (Fig. 8), which coursed more or less close to the raphe of the pons. The rostral perforating arteries The rostral arteries originated from the terminal part of the BA and entered the interpeduncular fossa (Fig. 9). They ranged in number from one to five per BA (mean, 3.0) and from zero to three on the right or the left side, respectively. The perforators were absent in 8.3% on the left side and in 16.6% on the right side. The perforators arose as individual vessels and/or by their own common stems (Fig. 9). The individual vessels were present in 41.6% on the right and in 66.6% on the left. They averaged 250.6 µm in diameter. The common trunks existed in 66.6% on the right and in 50% on the left. The trunks varied in diameter from 250 to 800 µm (Table 1). One or two of the perforating vessels originated from the BA in 91.6% (Fig. 10). They arose with the same frequency from the SCA, i.e., in 50% on the right side and in 58.3% on the left side. They arose either from the origin site or from the initial part of the SCA (Fig. 10). The perforators originated from the posterolateral artery in 16.6% and from the anterolateral artery in 8.3% of the hemispheres. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 11/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 10. The caudal and slightly oblique view of the large rostral perforator (1) arising from the BA (2). 3, a rostral perforating vessel originating from the left SCA (4) (cut); 5, a mesencephalic perforator of the left posterior cerebral artery; 6, a large common trunk of the interpeduncular perforators of the right posterior cerebral artery; 7, the right SCA (cut); 8, the posterolateral artery (cut). Most of the arteries originated rostral to the SCA. However, one of them was seen to arise at the level of the SCA in 41.6% and one arose between the SCA and the posterolateral artery in 33.3% of the brains. One of the vessels arose from the border between the BA and the posterior cerebral artery in 16.6%. The distance between the origin sites of the perforators and the SCA ranged from 0.7 to 2.1 mm (mean, 1.3 mm). The distance between the origin sites of the perforators and the bifurcation site of the BA varied from 0.9 to 3.9 mm (mean, 2.5 mm). The rostral perforating vessels gave rise to the anterolateral branches in 50% of the brains. The anterolateral branches coursed close to or along the pontomesencephalic sulcus. http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 12/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Anastomoses were present in 41.6% of the brains. Most of them were unilateral, but rightleft anastomoses were also seen occasionally. The anastomoses interconnected the rostral perforators themselves, these vessels and the interpeduncular (thalamoperforating) branches of the posterior cerebral artery, and finally the rostral perforators and the main stem of the SCA. The anastomotic channels ranged in diameter from 75 to 230 µm (mean, 138 µm). The rostral perforating arteries were located within the interpeduncular cistern, where they gave rise to their terminal and collateral branches (Fig. 11). The perforators entered the most caudal part of the interpeduncular fossa, just caudal to the penetration sites of the mesencephalic perforators of the posterior cerebral artery (Fig. 11). Figure 11. Three rostral perforating arteries. One of them (1) (cut) arises from the BA (2), another one (3) arises from the border between the BA and the posterior cerebral artery (4), and still another (5) arises from the small SCA (6). 7, the right SCA; 8, the mesencephalic perforator of the posterior cerebral artery; 9, the common trunk of the interpeduncular perforators of the posterior cerebral artery; 10, the left oculomotor nerve; 11, the transitional zone (cut) between the basis pontis and the crus cerebri; 12, the interpeduncular cistern. The caudal view of the specimen after transverse sectioning of the brain stem. The BA was displaced ventrally. DISCUSSION http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 13/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. When our results are compared with the findings of the other authors (7,9,13,14,23,39), one can notice certain similarities but also some differences. Thus, our description of the shape, direction, and branching pattern of the perforators is in accordance to the findings of the mentioned authors. As for the total number of perforators, however, there are discrepancies between their data (6 to 10 vessels) and our results (10 to 17 vessels). Some of the mentioned authors have probably overlooked some of the perforators, especially those from the caudal and the rostral groups, which are “hidden” between the BA and the basilar sulcus. Some of the other findings in this study seem to be mentioned rarely in the literature. This is especially true for the relationships of the perforators to the hypoglossal and abducent nerves, as well as to the side branches of the BA (Figs. 2 and 4). We hope that these findings, together with the observations of other authors, may help the neurosurgeons and neurologists to explain some symptoms and signs in patients with certain vascular syndromes of the brain stem. The perforating branches of the BA usually divide into the short and long terminal intrapontine vessels. The short arteries mainly irrigate the medial part of the pyramidal bundles. The long arteries supply the structures of the pontine tegmentum close to the raphe and the fourth ventricle, particularly the raphe nuclei, the paramedian reticular formation, the medial longitudinal fasciculus, the medial part of the medial lemniscus, and the abducent nucleus (7,14,21). However, there is a lack of precise data concerning the irrigation region of each of the three groups of BA perforators, especially in relation to their anatomical variability. The perforating branches of the BA can be affected by certain cerebrovascular diseases and malformations, particularly by aneurysms, arteriovenous malformations (AVMs), and occlusive disease. The infratentorial arterial aneurysms comprise between 2.5 and 15% of all saccular aneurysms. Of these, the aneurysms of the BA account for 59 to 77% (18,33,38,44). They are often associated with BA fenestration (3,18). The fusiform aneurysms may involve a shorter or longer segment of the BA (2,44). The saccular aneurysms can be located at the BA bifurcation point; at the origin site of the SCA; between the SCA and the P1 segment of the posterior cerebral artery; at the origin site of a long lateral pontine artery; at the middle part of the BA trunk, i.e., between the two long pontine arteries; at the origin site of the AICA; between the AICA and the right or the left vertebral artery; and at the vertebrobasilar junction. In any of these cases, the aneurysms may compress, stretch, distort, or embolize certain perforating branches of the BA. The infratentorial AVMs comprise between 5 and 7% of all intracranial AVMs (1,6,41,45). Some of them can be superficial or deep pontine malformations. The deep pontine AVMs can be paramedian, lateral, and dorsal (subventricular) ones. It is very likely that most of the paramedian and some of the subventricular AVMs have the BA perforators as the feeding arteries. The occlusive cerebrovascular disease involving the vertebrobasilar arterial system has been described by many authors (4,5,8,16,19,36,40). In some of these cases, the thrombic and embolic events affected the perforating branches of the BA. The type of clinical syndrome depends on the type of affected BA perforators, especially on their region of supply and their relationship with other collateral branches of the BA. According to our findings, the anastomoses involving the BA perforators ranged from 41.6 to 66.6%. The anastomotic channels could compensate the blood flow in some cases with occlusion of the perforators of the BA. REFERENCES: (1–45) 1. Batjer H, Samson D: Arteriovenous malformations of the posterior fossa. Clinical presentation, diagnostic evaluation, and surgical treatment. J Neurosurg 64:849–856, 1986. SFX [Context Link] 2. Batjer H, Purdy DP: Enlarging thrombosed aneurysm of the distal basilar artery. Neurosurgery 26:695– 700, 1990. SFX Buy Now [Context Link] http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 14/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. 3. Black SPW, Ansbacher LE: Saccular aneurysm associated with segmental duplication of the basilar artery. A morphological study. J Neurosurg 61:1005–1008, 1984. SFX [Context Link] 4. Bogousslavsky J, Meienberg O: Eyemovement disorders in brainstem and cerebellar stroke. Arch Neurol 44:141–148, 1987. SFX [Context Link] 5. Brazis PW: The localization of lesions affecting the brainstem, in Brazis PW, Masdeu JC, Biller J (eds): Localization in Clinical Neurology. Boston, Little, Brown and Company, 1985, pp 225–238. [Context Link] 6. Drake CG, Friedman AH, Peerles SJ: Posterior fossa arteriovenous malformations. J Neurosurg 64:1– 10, 1986. SFX [Context Link] 7. Duvernoy HM: Human Brainstem Vessels. Berlin, SpringerVerlag, 1978, pp 6–24. [Context Link] 8. Fisher CM: Lacunar strokes and infarcts: A review. Neurology 32:871–876, 1982. [Context Link] 9. Foix C, Hillemand P: Irrigation de la protubérance. C R Soc Biol (Paris) 92:35–36, 1925. [Context Link] 10. Gibo H, Kobayashi S, Kyoshima K, Hokama M: Microsurgical anatomy of the arteries of the pituitary stalk and gland viewed from above. Acta Neurochir (Wien) 90:60–66, 1988. SFX [Context Link] 11. Gibo H, Lenkey C, Rhoton AL: Microsurgical anatomy of the supraclinoid portion of the internal carotid artery. J Neurosurg 55:560–574, 1981. SFX [Context Link] 12. Gibo H, Ohigashi Y, Kobayashi S, Shimizu Y: Importance of the central branches in surgery of superior cerebellar aneurysms. Microsurgical anatomy of the central branches arising from the proximal superior cerebellar artery, in Sugita K, Shibuya M (eds): Intracranial Aneurysms and Arteriovenous Malformations. State of Art. Nagoya, Japan, Nagoya University COOP Press, 1990, pp 227–234. [Context Link] 13. Gillilan LA: The correlation of the blood supply to the human brain stem with clinical brain stem lesions. J Neuropathol Exp Neurol 23:78–108, 1964. SFX Buy Now [Context Link] 14. Gillilan LA: Anatomy and embryology of the arterial system of the brain stem and cerebellum, in Vinken PJ, Bruyn GW (eds): Handbook of Clinical Neurology. Amsterdam, NorthHolland Publishing Co., 1975, pp 24–44. [Context Link] 15. Gomes F, Dujovny M, Umansky F, Ausman JI, Diaz FG, Ray WJ, Mirchandani HG: Microsurgical anatomy of the recurrent artery of Heubner. J Neurosurg 60:130–139, 1984. SFX [Context Link] 16. Haines DE: Correlative Neuroanatomy. The Anatomical Bases of Some Common Neurological Deficits. Munich, Urban and Schwarzenberg, 1985, pp 38–53. [Context Link] 17. Haymaker W: Blood supply of the human hypothalamus, in Nauta WJH, Haymaker W, Anderson E (eds): The Hypothalamus. Springfield, IL, Charles C Thomas, 1969, pp 210–218. [Context Link] 18. Hoffman WF, Wilson CB: Fenestrated basilar artery with an associated saccular aneurysm. Case report. J Neurosurg 50:262–264, 1979. SFX [Context Link] 19. Kistler JP, Buonanno FS, DeWitt LD, Davis KR, Brady TJ, Fisher CM: Vertebralbasilar posterior cerebral territory stroke—delination by proton nuclear magnetic resonance imaging. Stroke 15:417–426, http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 15/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. 1984. SFX [Context Link] 20. Lang J, Schaffrath H, Fischer G: Weitere Befunde zu den Rami diencephalici. Neurochirurgia (Stuttg) 30:103–107, 1987. SFX [Context Link] 21. Lazorthes G, Gouazé A, Salamon G: Vascularisation et Circulation de L'Encéphale. Paris, Masson, 1976, pp 196–204. [Context Link] 22. Leeds NE: The striate (lenticulostriate) arteries and the artery of Heubner, in Newton T, Potts DG (eds): Radiology of the Skull and Brain. Angiography. St. Louis, CV Mosby, 1974, vol 2, bk 2, pp 1527–1539. [Context Link] 23. Mahmood A, Dujovny M, Torche M, Dragovi< L, Ausman JI: Microvascular anatomy of the foramen caecum medullae oblongatae. J Neurosurg 75:299–304, 1991. SFX [Context Link] 24. Marinkovi< SV, Kovacevi< MS, Marinkovi< JM: Perforating branches of the middle cerebral artery. Microsurgical anatomy of their extracerebral segments. J Neurosurg 63:266–271, 1985. [Context Link] 25. Marinkovi< SV, Milisavljevi< MM, Kovacevi< MS, Stevi< ZD: Perforating branches of the middle cerebral artery. Microanatomy and clinical significance of their intracerebral segments. Stroke 16:1022– 1029, 1985. [Context Link] 26. Marinkovi< S, Milisavljevi< M, Kovacevi< M: Anatomical bases for surgical approach to the initial segment of the anterior cerebral artery. Microanatomy of Heubner's artery and perforating branches of the anterior cerebral artery. Surg Radiol Anat 8:7–18, 1986. [Context Link] 27. Marinkovi< S, Milisavljevi< M, Kovacevi< M: Interpeduncular perforating branches of the posterior cerebral artery. Microsurgical anatomy of their extracerebral and intracerebral segments. Surg Neurol 26:349–359, 1986. [Context Link] 28. Marinkovi< SV, Milisavljevi< MM, Marinkovi< ZD: Microanatomy and possible clinical significance of anastomoses among hypothalamic arteries. Stroke 20:1341–1352, 1989. [Context Link] 29. Marinkovi< S, Milisavljevi< M, Marinkovi< Z: Branches of the anterior communicating artery. Microsurgical anatomy. Acta Neurochir (Wien) 106:78–85, 1990. [Context Link] 30. Marinkovi< SV, Milisavljevi< MM, Marinkovi< ZD: The perforating branches of the internal carotid artery: The microsurgical anatomy of their extracerebral segments. Neurosurgery 26:472–479, 1990. [Context Link] 31. Milisavljevi< MM, Marinkovi< SV, Gibo H, Puskas LF: The thalamogeniculate perforators of the posterior cerebral artery: The microsurgical anatomy. Neurosurgery 28:523–530, 1991. [Context Link] 32. Pedroza A, Dujovny M, CabezudoArtero J, Umansky F, Kim Berman S, Diaz FG, Ausman JI, Mirchandani G: Microanatomy of the premamillary artery. Acta Neurochir (Wien) 86:50–55, 1987. SFX [Context Link] 33. Rhoton AL: Anatomy of saccular aneurysms. Surg Neurol 14:59–66, 1980. SFX [Context Link] 34. Rhoton AL, Fujii K, Fradd B: Microsurgical anatomy of the anterior choroidal artery. Surg Neurol http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 16/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. 12:171–187, 1979. SFX [Context Link] 35. Rosner SS, Rhoton AL, Ono M, Barry M: Microsurgical anatomy of the anterior perforating arteries. J Neurosurg 61:468–485, 1984. SFX [Context Link] 36. Savoiardo M, Bracchi M, Passerini A, Visciani A: The vascular territories in the cerebellum and brainstem: CT and MR study. AJNR 8:199–209, 1987. SFX [Context Link] 37. Schlesinger B: The Upper Brainstem in the Human. Its Nuclear Configuration and Vascular Supply. Berlin, SpringerVerlag, 1976, pp 76–142. [Context Link] 38. Solomon RA, Stein BM: Surgical approach to aneurysms of the vertebral and basilar arteries. Neurosurgery 23:203–208, 1988. [Context Link] 39. Stephens RB, Stilwell DL: Arteries and Veins of the Human Brain. Springfield, Illinois, Charles C. Thomas, 1969, pp 71–123. [Context Link] 40. Ueda K, Toole JF, McHenry LC: Carotid and vertebrobasilar transient ischemic attacks: Clinical and angiographic correlation. Neurology 29:1094–1101, 1979. SFX [Context Link] 41. Veerapen RJ, Sbeih IA, O'Laoire SA: Surgical treatment of cryptic AVM's and associated hematoma in the brain stem and spinal cord. J Neurosurg 65:188–193, 1986. SFX [Context Link] 42. Vincentelli F, Lehman G, Caruso G, Grisoli F, Rabehanta P, Gouaze A: Extracerebral course of the perforating branches of the anterior communicating artery: Microsurgical anatomical study. Surg Neurol 35:98–104, 1991. SFX [Context Link] 43. Yasargil MG: Microneurosurgery. Vol I. Microsurgical Anatomy of the Basal Cisterns and Vessels of the Brain, Diagnostic Studies, General Operative Techniques and Pathological Considerations of the Intra cranial Aneurysms. Stuttgart, Georg Thieme Verlag, 1984, pp 128–134. [Context Link] 44. Yasargil MG: Microneurosurgery. Vol II. Clinical Considerations, Surgery of the Intracranial Aneurysms and Results. Stuttgart, Georg Thieme Verlag, 1984, pp 232–260. [Context Link] 45. Yasargil MG: Microneurosurgery. Vol IIIA. AVM of the Brain, History, Embryology, Pathological Considerations, Hemodynamics, Diagnostic Studies, Microsurgical Anatomy. Stuttgart, Georg Thieme Verlag, 1987, pp 63–73. [Context Link] COMMENTS These authors have provided a concise review of the origin and termination of the perforating branches of the basilar artery. The relevance of this information to the treatment of infratentorial aneurysms and arteriovenous malformations is reviewed, and the vascular syndromes associated with the occlusion of the various groups of perforating branches are discussed. This represents a nice addition to our understanding of the anatomy of this critical area. Albert L. Rhoton Gainesville, Florida COMMENTS http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 17/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. More than three centuries have passed since Thomas Willis, Professor of Natural History at Oxford University, published his Cerebri Anatomy and illustrated, with considerable accuracy, the arteries at the base of the brain. It is astonishing that Professor Marinkovi< and Dr. Gibo have added useful anatomical information in 1993. They have provided us with a fresh look at anatomy, which is so important to cranial base and cerebrovascular surgeons, and have depicted it in a way that is readily understandable and applicable. Sidney J. Peerless Miami, Florida KEY WORDS: Anatomy; Basilar artery; Brain stem; Cerebral artery; Cerebrovascular occlusive disease; Perforating artery IMAGE GALLERY Select All Export Selected to PowerPoint Table 1 Figure 2 Figure 1 Figure 4 Figure 3 http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi Figure 5 18/19 31.05.2016 Ovid: The Surgical Anatomy of the Perforating Branches of the Basilar Artery. Figure 7 Figure 8 Figure 6 Figure 9 Figure 10 Figure 11 Back to Top © 2016 Ovid Technologies, Inc. All rights reserved. About Us Contact Us Terms of Use OvidSP_UI03.20.00.112, SourceID 105955 http://ovidsp.tx.ovid.com/sp3.20.0b/ovidweb.cgi 19/19