* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Proposal for a Functional Classification System of Heart Failure in
Cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Rheumatic fever wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Coronary artery disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Journal of the American College of Cardiology
2014 by the American College of Cardiology Foundation
Published by Elsevier Inc.
Vol. 63, No. 13, 2014
ISSN 0735-1097/$36.00
http://dx.doi.org/10.1016/j.jacc.2014.01.020
WORKGROUP REPORT
Proposal for a Functional Classification
System of Heart Failure in Patients With
End-Stage Renal Disease
Proceedings of the Acute Dialysis
Quality Initiative (ADQI) XI Workgroup
Lakhmir S. Chawla, MD,* Charles A. Herzog, MD,y Maria Rosa Costanzo, MD,z James Tumlin, MD,x
John A. Kellum, MD,k Peter A. McCullough, MD, MPH,{# Claudio Ronco, MD,**
for the ADQI XI Workgroup
Washington, DC; Minneapolis, Minnesota; Naperville, Illinois; Chattanooga, Tennessee;
Pittsburgh, Pennsylvania; Dallas and Plano, Texas; and Vicenza, Italy
Structural heart disease is highly prevalent in patients with chronic kidney disease requiring dialysis. More than 80%
of patients with end-stage renal disease (ESRD) are reported to have cardiovascular disease. This observation has
enormous clinical relevance because the leading causes of death for patients with ESRD are of cardiovascular
disease etiology, including heart failure, myocardial infarction, and sudden cardiac death. The 2 systems most
commonly used to classify the severity of heart failure are the New York Heart Association (NYHA) functional
classification and the American Heart Association (AHA)/American College of Cardiology (ACC) staging system. With
rare exceptions, patients with ESRD who do not receive renal replacement therapy (RRT) develop signs and
symptoms of heart failure, including dyspnea and edema due to inability of the severely diseased kidneys to excrete
sodium and water. Thus, by definition, nearly all patients with ESRD develop a symptomatology consistent with heart
failure if fluid removal by RRT is delayed. Neither the AHA/ACC heart failure staging nor the NYHA functional
classification system identifies the variable symptomatology that patients with ESRD experience depending upon
whether evaluation occurs before or after fluid removal by RRT. Consequently, the incidence, severity, and outcomes
of heart failure in patients with ESRD are poorly characterized. The 11th Acute Dialysis Quality Initiative has
identified this issue as a critical unmet need for the proper evaluation and treatment of heart failure in patients with
ESRD. We propose a classification schema based on patient-reported dyspnea assessed both pre- and postultrafiltration, in conjunction with echocardiography. (J Am Coll Cardiol 2014;63:1246–52) ª 2014 by the
American College of Cardiology Foundation
The literature provides multiple definitions of heart failure
(1). A recent attempt to describe this syndrome posited that
heart failure is a mechanical and neurohumoral syndrome in
which the heart fails as a pump, resulting in stasis of blood in
the lungs and venous system, fatigue, effort intolerance, and
reduced longevity. From a purely mechanical perspective,
heart failure is defined as a clinical syndrome that can result
from any structural or functional cardiac disorder impairing
ventricular filling or ejection of blood (2). Incidence of
structural heart disease is high in patients with advanced
chronic kidney disease (CKD), particularly those with endstage renal disease (ESRD) requiring dialysis. In large
observational cohort studies, more than 80% of patients with
ESRD are reported to have cardiovascular disease (3,4). This
observation is of paramount clinical relevance because the
leading causes of death for patients with ESRD are due to
From the *Department of Medicine, Division of Nephrology, Washington DC
Veterans Affairs Medical Center, and Department of Anesthesiology and Critical
Care Medicine, George Washington University Medical Center, Washington, DC;
yDepartment of Medicine, Division of Cardiology, Hennepin County Medical
Center, University of Minnesota, Minneapolis, Minnesota; zMidwest Heart
Specialists–Advocate Medical Group, Naperville, Illinois; xSoutheast Renal Research
Institute, Chattanooga, Tennessee; kCenter for Critical Care Nephrology, Department of Critical Care Medicine, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania; {Baylor University Medical Center, Baylor Heart and Vascular
Institute, Baylor Jack and Jane Hamilton Heart and Vascular Hospital, Dallas, Texas;
#Heart Hospital, Plano, Texas; and the **Department of Nephrology, Dialysis, and
Transplantation, International Renal Research Institute, San Bortolo Hospital,
Vicenza, Italy. A complete list of the ADQI Workgroup members is in the Online
Appendix. The 11th international ADQI Consensus Conference was funded in
part by generous support in the form of unrestricted educational grants from
Alere Medical, Astute Medical, Fresenius Medical Care, and Gambro Medical.
The sponsors had no input on the content of this manuscript. Dr. Costanzo has
served as a consultant and speaker for Gambro Medical. All other authors have
reported that they have no relationships relevant to the contents of this paper to
disclose.
Manuscript received November 23, 2013; revised manuscript received January 4,
2014, accepted January 6, 2014.
JACC Vol. 63, No. 13, 2014
April 8, 2014:1246–52
Chawla et al.
Functional Classification of Heart Failure With End-Stage Renal Disease
cardiovascular disease, including heart failure, myocardial
infarction, and sudden cardiac death (3,5–7).
In CKD, and particularly ESRD, 3 major mechanisms
induce and exacerbate cardiomyopathy: volume overload,
pressure overload, and nonhemodynamic factors associated
with CKD. The nonhemodynamic factors are manifold, and
include activation of the renin-angiotensin system, catalytic
iron-dependent oxidative stress, inflammation, and stimulation
of profibrogenic factors (5,7) These pathological mechanisms
cause direct and immediate effects and affect long-term disease
progression in these patients (5,7).
The American Heart Association (AHA), American
College of Cardiology (ACC), and European Society of
Cardiology (ESC) have developed guidelines recommending
that heart failure be classified in a manner that reflects its
risk factors, severity, and natural history (2,8,9). In the
AHA/ACC guidelines, stage C heart failure defines patients
with current or prior symptoms of heart failure. The primary
form of maintenance renal replacement therapy (RRT)
worldwide is hemodialysis, and a smaller proportion of patients use peritoneal dialysis. With rare exceptions, lack of
fluid removal by RRT in patients undergoing dialysis leads
to dyspnea and congestion due to salt and water retention.
Thus, by definition, all patients undergoing dialysis, even
those with no structural heart disease, experience New York
Heart Association (NYHA) functional class (FC) III to IV
symptoms if fluid removal by RRT is delayed. Thus, management and treatment of patients undergoing dialysis with
heart failure is difficult due to the dynamic nature of fluid
overload.
A “real world” example is illustrated by the following
clinical vignette: a patient undergoing dialysis is referred
to the cardiologist because of worsening heart failure
symptoms. Because of transport to and from the dialysis
clinic in addition to the time required for dialysis, which
usually exceeds 6 h, patients on dialysis rarely schedule nonnephrology doctor’s visits on the same day as dialysis sessions. Thus, visits to the cardiologist almost always occur
prior to a dialysis day. During the visit, the cardiologist
correctly identifies fluid overload, and the patient is likely to
be returned to the nephrologist for “better” dialysis and more
ultrafiltration. This is problematic because the nephrologist
likely sent the patient to the cardiologist because the patient
was already receiving the maximal tolerable ultrafiltration.
The incidence, severity, and outcomes of heart failure in
patients undergoing dialysis are poorly characterized and
potentially undertreated, because the severity of symptoms
relative to the frequent changes in volume status occurring
before and after RRT are not witnessed and remain poorly
documented (5,7). In addition, none of the existing practice
guidelines for the treatment of fluid overload in patients on
dialysis comment on whether it is appropriate to apply the
AHA/ACC/ESC stages of heart failure or the NYHA FC
system (10).
For advancement in the treatment of heart failure in patients
on dialysis, a methodology that improves the characterization
1247
of heart failure in these patients is
Abbreviations
and Acronyms
essential and urgently required.
The implementation of classificaACC = American College of
tion systems for any disease synCardiology
drome can have a positive impact
ADQI = Acute Dialysis
on disease management (10–12).
Quality Initiative
For example, introduction of the
AHA = American Heart
CKD staging system and the Risk,
Association
Injury, Failure, Loss, End-stage
CKD = chronic kidney
renal disease (RIFLE) (11,12)
disease
staging system for acute kidney
ESC = European Society of
Cardiology
injury have allowed clinical investigators to better characterize
ESRD = end-stage renal
disease
disease processes, conduct epidemiological studies, guide clinical
FC = functional class
trial enrollment, standardize pracNYHA = New York Heart
Association
tice guidelines, and improve
clinicians’ ability to track disease
RRT = renal replacement
therapy
progression (13,14).
The 11th Acute Dialysis
Quality Initiative (ADQI) meeting was convened to focus
on cardiorenal syndrome (15). The working group that
focused on cardiorenal syndrome type IV (advanced CKD
and progressive heart disease) identified this clinical and
research issue as a critical unmet need in the care of patients
on dialysis with heart failure. We based this assessment on
the fact that accurate risk stratification of patients with any
given disease state is essential to improve clinical status and
outcomes.
Workgroup Methodology
The specific methods for the ADQI conferences were
developed and refined over the first 4 international conferences (16). Briefly, our methods comprise: 1) a systematic
search for evidence, with review and evaluation of the
available literature; 2) establishment of clinical and physiological outcomes and of measures to be used for treatment
comparisons; 3) description of current practice and the
rationale for use of current techniques; and 4) analysis of
areas in which evidence is lacking and future research is
required to obtain new information. The topics chosen for
each conference are selected on the basis of the following
criteria: 1) prevalence of the clinical problem; 2) estimates
of variation in clinical practice; 3) potential influence
on outcome; 4) potential for development of evidence-based
guidelines; and 5) availability of scientific evidence. A
detailed report of the ADQI process has been published
previously (16).
Before the conference and according to the structure of
previous ADQI consensus meetings, we performed a systematic review of the literature (11,17). Specifically, we used
the search terms “heart failure,” “peritoneal dialysis,” “hemodialysis,” “renal replacement therapy,” “chronic kidney
disease,” “dialysis,” “guidelines,” “consensus,” and “end-stage
renal/kidney disease,” combined with “prognosis,” “major
Chawla et al.
Functional Classification of Heart Failure With End-Stage Renal Disease
1248
adverse cardiovascular events,” “myocardial infarction,”
“stroke,” “volume overload,” “fluid overload,” “sudden cardiac death,” “death,” and “mortality.” In view of the volume
of retrieved literature, only representative publications are
cited in this proposal. Furthermore, we opted to base our
staging proposal on clinical scenarios for which data are
ample. We also excluded the specific clinical situations
pertaining to renal or heart transplant or to mechanical
circulatory support.
Based on the literature identified prior to the conference,
the following key questions were considered:
1. Are there current heart failure staging systems that can
be applied specifically to patients undergoing dialysis?
2. What are the critical features of a staging system that
can be easily used by clinicians to establish appropriate
diagnostic and therapeutic approaches?
3. How can a new heart failure staging system specifically
address the unique nature of nonphysiological periodic
volume removal, which characterizes all forms of
dialysis?
Current Staging Systems of Heart Failure
Multiple heart failure staging systems and classification
schemes have been proposed. In 1977, Wagner and Cohn
(18) proposed a classification system based on 3 broad
pathophysiological mechanisms: systolic dysfunction, diastolic dysfunction, and volume overload. These 3 conceptual
etiologies remain relevant in the current assessment and
treatment of heart failure. Since 2005, the ESC/ACC/AHA
have developed consensus guidelines that include a staging
system for heart failure to reflect its severity as well as its
natural history (2). However, the most commonly used
system to characterize the severity of heart failure symptoms
is the NYHA FC (10) (Table 1), which is based on a
grading of dyspnea relative to the intensity of physical activity. The ESC/ACC/AHA and NYHA classification
systems have proven to be robust and have been used successfully to assess the epidemiology and severity of heart
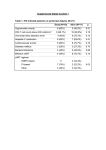
Table 1
New York Heart Association Function Classification
Class
Patient Symptoms
Class I (mild)
No limitation of physical activity. Ordinary physical
activity does not cause undue fatigue, palpitation,
or dyspnea.
Class II (mild)
Slight limitation of physical activity. Comfortable at rest,
but ordinary physical activity results in fatigue,
palpitation, or dyspnea.
Class III (moderate)
Marked limitation of physical activity. Comfortable at
rest, but less than ordinary activity causes fatigue,
palpitation, or dyspnea.
Class IV (severe)
Unable to carry out any physical activity without
discomfort. Symptoms of cardiac insufficiency
at rest. If any physical activity is undertaken,
discomfort is increased.
Data from the Criteria Committee of the New York Heart Association (10).
JACC Vol. 63, No. 13, 2014
April 8, 2014:1246–52
failure. They have been the basis for establishing inclusion
criteria and response to therapy in seminal clinical trials
conducted in patients with heart failure (19–21).
However, neither of these staging systems can be used in
their current forms to assess the severity of heart failure
in patients on dialysis because dyspnea in these patients is
not solely attributable to heart failure and its severity changes
in relation to the timing of volume removal. For nearly all
patients undergoing dialysis, delay in or absence of RRT
results in dyspnea due to fluid overload even if the patient’s
heart is structurally normal. Thus, all patients on dialysis can
theoretically be considered in NYHA FC III to IV, which
can improve to NYHA FC I after fluid removal. In patients
not on dialysis with acutely decompensated heart failure,
euvolemia can be restored and maintained for variable periods of time with appropriate medical therapies; however,
all patients undergoing dialysis begin to retain salt and water
immediately after RRT treatment, and accumulation continues until the next prescribed RRT (this occurs in both
peritoneal dialysis and hemodialysis to varying degrees).
We concluded that a staging system for heart failure in
patients on dialysis must be able to define heart failure
symptoms in relation to the response to the periodic nonphysiological volume removal that occurs with all forms of
dialysis. Thus, the timing of assessment and the periodicity
of dialysis must be taken into account. In addition, we
sought to develop a patient-centered staging system that was
easily understandable by care providers and therefore easily
usable for planning further diagnostic evaluations and
treatment for patients with coexisting heart failure and
dialysis-requiring ESRD.
Proposed Staging System
We considered a number of possible solutions to the
problem outlined in the previous text. To specifically
exclude patients with normal hearts on dialysis, the proposed classification system incorporates echocardiographic
criteria that indicate the presence of underlying structural
heart disease. We modified the NYHA FC of dyspnea
severity into a new system with a description of heart failure
symptoms and their response to fluid removal by RRT/
ultrafiltration. The 3 elements of our proposed staging
schema are as follows:
1. Standardized echocardiographic evidence of structural
and/or functional heart abnormalities;
2. Dyspnea occurring in the absence of primary lung
disease, including isolated pulmonary hypertension;
and
3. Response of congestive symptoms to RRT/ultrafiltration.
The standardized echocardiographic criteria are based
on the evidence of mild to moderate echocardiographic
disease cutoffs that are detailed in the American Association
of Echocardiography consensus guidelines (which are
consistent with the European Society of Echocardiography
JACC Vol. 63, No. 13, 2014
April 8, 2014:1246–52
Table 2
Chawla et al.
Functional Classification of Heart Failure With End-Stage Renal Disease
Echocardiography Criteria*
LVH (LV mass index >110 g/m2 for women and >130 g/m2 for men or
>47 g/m2.7 for women and >50 g/m2.7 for men). Latter measure is
LV mass calculated by the area-length method and indexed to height
(22,38,39).
Increased LV volume index >86 ml/m2 diastolic or >37 ml/m2 systolic.
Left atrial enlargement (left atrial volume index 34 ml/m2).
Diastolic dysfunction (ASE grade 2).
Moderate to severe mitral or aortic valvular disease (stenosis or regurgitation).
RV systolic dysfunction by accepted criteria (e.g., TAPSE <17 mm).
LV ejection fraction 45%.
Regional wall motion abnormality of LV (>10% of the myocardium).
*At least 1 (of 8) listed criteria must be abnormal to fulfill the definition of echocardiographic
evidence of heart disease.
LV ¼ left ventricle; LVH ¼ left ventricular hypertrophy; RV ¼ right ventricle; TAPSE ¼ tricuspid
annular plane systolic excursion.
guidelines) (22,23). The echocardiographic criteria that
suggest or are supportive of cardiac disease are summarized
in Table 2.
The classification system that we propose is summarized
in Figure 1.
Patients who present with severe dyspnea that is relieved
by RRT/ultrafiltration are categorized by their post-therapy
status. For example, a patient with echocardiographic evidence of left ventricular hypertrophy who presents to the
dialysis clinic with dyspnea at rest, undergoes RRT, and
Figure 1
1249
then experiences no symptoms would be classified as ADQI
class 2R. In addition, the RRT/ultrafiltration metric does
not necessarily suggest a single therapy. Symptomology
relieved by RRT/ultrafiltration assumes that the patient is
receiving RRT at the appropriate frequency.
Strengths and limitations. Like previously published
staging systems, the proposed classification system will
require prospective testing and validation in appropriate
patient cohorts. In addition, because echocardiographic
findings are a prerequisite for entry into the classification
system, standardization of the collection and documentation
of these echocardiographic data is imperative.
Studies in patients undergoing dialysis that deployed
continuous hemodynamic monitoring before, during, and
after RRT with ultrafiltration have demonstrated that interdialytic volume accumulation results in increased pressures in
the pulmonary artery and right ventricle (Fig. 2) (24,25). The
proposed staging system accommodates the “tidal nature” of
nonphysiological volume removal. Another strength of this
proposed system is that symptom grading is similar to grading
in other heart failure symptom scales (e.g., the NYHA FC
system) that are familiar to clinicians. In addition, the proposed staging system is based on patient-reported symptomology and is thus patient centered.
Patients with heart failure on dialysis pose unique diagnostic and therapeutic challenges; for example, a patient
ADQI Heart Failure in ESRD Classification System
Classification is determined by a dyspnea assessment before and after renal replacement therapy (RRT)/ultrafiltration (UF). When patients have the same class assessment
before and after RRT/UF, they are scored by their post-treatment assessment. The classification scheme assumes that the class assignment represents the patient’s
achievement of optimized UF and is representative of the patient’s usual level of dyspnea before and after RRT/UF. *If dyspnea symptoms improve to class I levels, the patient
would be classified as class 2R. zIf dyspnea symptoms improve to class II levels, the patient would be classified as class 3R. ADQI ¼ Acute Dialysis Quality Initiative;
ESRD ¼ end-stage renal disease; NYHA ¼ New York Heart Association.
1250
Figure 2
Chawla et al.
Functional Classification of Heart Failure With End-Stage Renal Disease
JACC Vol. 63, No. 13, 2014
April 8, 2014:1246–52
Changes in Right Heart Pressures Over 8 Days in Patients Undergoing Hemodialysis
Eight-day continuous hemodynamic trend from a patient who underwent thrice-weekly hemodialysis (HD). A marked reduction in right ventricular systolic pressure (RVSP) and
right ventricular diastolic pressure (RVDP), as well as estimated pulmonary artery diastolic (ePAD) pressure, was seen during each dialysis session, followed by progressive
pressure increments until the next dialysis session. The most marked increase in cardiac pressures was seen the day after a weekend (i.e., an extra day without dialysis). The
solid line shows the median value, and the shaded areas are the range (6th and 94th percentiles). HD procedures are indicated at the top of the graph. bpm ¼ beats/min.
(Permission pending.)
with mild left ventricular dysfunction undergoing dialysis
who becomes dyspneic may be deemed to have fluid overload and referred back to the nephrologist for standard
thrice-weekly hemodialysis and additional ultrafiltration.
Thus, RRT is a form of treatment for ESRD with heart
failure. However, in some cases, this therapy fails to improve
or resolve the symptoms of dyspnea. This clinical scenario
raises multiple questions regarding presence and severity
of heart failure, type of monitoring required, and therapeutic
approaches needed to treat the persistent symptoms. A
validated classification system would prove useful here and
could potentially be useful for uniform assessment of heart
failure in patients undergoing dialysis. In addition, surveillance of these patients will allow better understanding of the
temporal aspects of heart failure and ESRD. Specifically,
does heart failure usually precede ESRD, is it the reverse, or
is this a cardiorenal interaction?
Validation of the proposed system would start with
classification of a large cohort of patients undergoing
dialysis. The initial assessment would include collection and
documentation of appropriate echocardiographic data.
Echocardiography is recommended for all patients on
dialysis within 1 to 3 months of starting RRT (5,7). In
addition, patients would be queried about the presence of
dyspnea pre- and post-RRT/ultrafiltration. Simple tools
such as the Likert scale and visual analogue scale have been
shown to be useful in the assessment of dyspnea in patients
with heart failure and could be used as appropriate (26,27).
Assessment of patient symptoms pre- and post-RRT is
routine and considered standard of care. However, these
data may not always be gathered in standard database data
fields, and standardization may be required. Once the
prevalence of the various stages of the new classification
system is determined, follow-up to assess outcomes would
be needed. Our operating hypothesis is that mortality risk
would increase through each of the proposed stages. After
initial longitudinal assessment, the proposed staging system
might be useful for clinical trial entry and design. For
example, does more frequent hemodialysis improve ADQI
class function? Are outcomes for patients with advanced
heart failure and ESRD improved with peritoneal dialysis
versus hemodialysis? In addition, certain standard heart
failure medications (e.g., angiotensin-converting enzyme
inhibitors, angiotensin II receptor blockers, beta-blockers)
might be better suited for certain ADQI heart failure
stages than for others. Recent data suggest that treating
patients with ESRD with spironolactone may improve
structural heart disease and improve survival, and the proposed classification schema should be deployed in
conjunction with future studies of aldosterone blockade in
patients with ESRD (28,29).
In addition to future research concerning the descriptive
epidemiology and prognosis of patients on dialysis classified with this new scheme, future studies may use novel
technologies such as advanced imaging and biomarkers to
aid in support of the classification or in the traditional
domains of testing (screening, diagnosis, prognosis, and
management) (30,31).
JACC Vol. 63, No. 13, 2014
April 8, 2014:1246–52
Chawla et al.
Functional Classification of Heart Failure With End-Stage Renal Disease
Future Directions
Important therapies for patients with heart failure on dialysis
may include more frequent hemodialysis, preference for
peritoneal dialysis, or polyelectrolytes that remove sodium
via the gut (32). For patients who are dyspneic even with
good volume control, standard heart failure therapies may
require additional adjustments. However, before treatment
advances can be made, it is essential to be able to differentiate patients with fluid overload alone in the absence of
structural heart disease from patients in whom fluid overload
and dyspnea can be directly attributed to underlying cardiac
disease.
The precise criteria that define echocardiographic evidence of structural heart disease are an important component
of any proposed classification, specifically, the differentiation
of heart failure with preserved ejection fraction versus volume overload alone. Both clinical entities can present with
clinical and echocardiographic features of “diastolic dysfunction.” For the subset of patients in whom this distinction is
required, we propose a diagnostic pathway to ascertain the
correct diagnosis (Online Appendix). The distinction can
be particularly important in patients undergoing dialysis
due to the high prevalence of left ventricular hypertrophy.
Schwartzenberg et al. (33) demonstrated that 35% of patients with heart failure with preserved ejection fraction,
despite elevated left ventricular end-diastolic pressure values,
experienced a drop in stroke volume with intravenous nitroprusside. This appears to be due to excessive reduction in
filling pressure and thus filling volume (end-diastolic volume)
due to diastolic dysfunction. Many patients on dialysis would
be expected to experience something similar with volume
removal during RRT.
The dynamic assessment (i.e., before and after ultrafiltration) is particularly important given that asymptomatic diastolic dysfunction is prevalent in the community and may
be more prevalent in the ESRD population (34). As suggested in the Kidney Disease: Improving Global Outcomes
consensus guideline, echocardiography should be performed
in all incident patients on dialysis (5). Novel and known
cardiac biomarkers, along with dynamic exercise testing, may
also be useful in identifying important subgroups (35).
More invasive hemodynamic monitoring may be of benefit
for some patients and for research purposes (24). In the
development of a new classification schema, the epidemiology and phenotype of this population should be well
characterized. Other important considerations include the
standardization of dyspnea assessment and timing of echocardiographic assessment (36).
At the end of 2010, the patient population on dialysis was
more than 300,000 in Europe and 414,000 in the United
States; these numbers are projected to increase as the population ages (37). Patients undergoing dialysis are characterized by a tremendous burden of structural heart disease
and are uniquely susceptible to the consequences of nonphysiological changes in volume status (5). Therefore, the
1251
standardization of heart failure diagnosis, prognosis, and
treatment is an urgent concern for these patients and for the
clinicians charged with delivery of their medical care.
Acknowledgments
The authors thank Kiran Khush for reviewing this manuscript and Nan Booth, MSW, MPH, ELS, of the Minneapolis Medical Research Foundation, for manuscript editing.
The authors thank the AARVI Onlus Foundation of
Vicenza for hosting the ADQI Consensus Conference.
Reprint requests and correspondence: Dr. Lakhmir S. Chawla,
Department of Anesthesiology and Critical Care Medicine, George
Washington University Medical Center, 900 23rd Street NW,
RILF, G-105, Washington, DC 20037. E-mail: minkchawla@
gmail.com.
REFERENCES
1. Felker GM, Adams KF Jr., Konstam MA, O’Connor CM,
Gheorghiade M. The problem of decompensated heart failure: nomenclature, classification, and risk stratification. Am Heart J 2003;145:S18–25.
2. Hunt SA. ACC/AHA 2005 guideline update for the diagnosis and
management of chronic heart failure in the adult: a report of the
American College of Cardiology/American Heart Association Task
Force on Practice Guidelines (Writing Committee to Update the 2001
Guidelines for the Evaluation and Management of Heart Failure).
J Am Coll Cardiol 2005;46:e1–82.
3. House AA. Cardio-renal syndrome type 4: epidemiology, pathophysiology and treatment. Semin Nephrol 2012;32:40–8.
4. Cheung AK, Sarnak MJ, Yan G, et al. Cardiac diseases in maintenance
hemodialysis patients: results of the HEMO study. Kidney Int 2004;
65:2380–9.
5. Herzog CA, Asinger RW, Berger AK, et al. Cardiovascular disease in
chronic kidney disease. A clinical update from Kidney Disease:
Improving Global Outcomes (KDIGO). Kidney Int 2011;80:572–86.
6. Herzog CA, Mangrum JM, Passman R. Sudden cardiac death and
dialysis patients. Semin Dial 2008;21:300–7.
7. K/DOQI clinical practice guidelines for cardiovascular disease in
dialysis patients. Am J Kidney Dis 2005;45:S1–153.
8. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for
the diagnosis and treatment of acute and chronic heart failure 2012:
the Task Force for the Diagnosis and Treatment of Acute and Chronic
Heart Failure 2012 of the European Society of Cardiology. Developed
in collaboration with the Heart Failure Association (HFA) of the ESC.
Eur J Heart Fail 2012;14:803–69.
9. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline
for the management of heart failure: a report of the American College
of Cardiology Foundation/American Heart Association Task Force on
Practice Guidelines. J Am Coll Cardiol 2013;62:e147–239.
10. The Criteria Committee of the New York Heart Association. Diseases
of the Heart and Blood Vessels: Nomenclature and Criteria for
Diagnosis. 6th edition. Boston, MA: Little Brown, 1964.
11. Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal
failureddefinition, outcome measures, animal models, fluid therapy
and information technology needs: the Second International Consensus
Conference of the Acute Dialysis Quality Initiative (ADQI) Group.
Crit Care 2004;8:R204–12.
12. Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice
guidelines for chronic kidney disease: evaluation, classification, and
stratification. Ann Intern Med 2003;139:137–47.
13. Weiner DE, Tighiouart H, Amin MG, et al. Chronic kidney disease as a
risk factor for cardiovascular disease and all-cause mortality: a pooled
analysis of community-based studies. J Am Soc Nephrol 2004;15:1307–15.
14. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic
kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351:1296–305.
1252
Chawla et al.
Functional Classification of Heart Failure With End-Stage Renal Disease
15. Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal
syndrome. J Am Coll Cardiol 2008;52:1527–39.
16. Kellum JA, Bellomo R, Ronco C. Acute Dialysis Quality Initiative
(ADQI): methodology. Int J Artif Organs 2008;31:90–3.
17. Kellum JA, Ronco C, Mehta R, Bellomo R. Consensus development in
acute renal failure: the Acute Dialysis Quality Initiative. Curr Opin Crit
Care 2005;11:527–32.
18. Wagner S, Cohn K. Heart failure. A proposed definition and classification. Arch Intern Med 1977;137:675–8.
19. Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor
blocker valsartan in chronic heart failure. N Engl J Med 2001;345:
1667–75.
20. Cohn JN, Archibald DG, Ziesche S, et al. Effect of vasodilator
therapy on mortality in chronic congestive heart failure. Results of a
Veterans Administration cooperative study. N Engl J Med 1986;314:
1547–52.
21. The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative
North Scandinavian Enalapril Survival Study (CONSENSUS). N Engl
J Med 1987;316:1429–35.
22. Lang RM, Bierig M, Devereux RB, et al. Recommendations for
chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber
Quantification Writing Group, developed in conjunction with the
European Association of Echocardiography, a branch of the European
Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440–63.
23. Barbieri A, Bursi F, Mantovani F, et al. Left ventricular hypertrophy
reclassification and death: application of the recommendation of the
American Society of Echocardiography/European Association of
Echocardiography. Eur Heart J Cardiovasc Imaging 2012;13:109–17.
24. Kjellstrom B, Braunschweig F, Lofberg E, Fux T, Grandjean PA,
Linde C. Changes in right ventricular pressures between hemodialysis
sessions recorded by an implantable hemodynamic monitor. Am J
Cardiol 2009;103:119–23.
25. Braunschweig F, Kjellstrom B, Soderhall M, Clyne N, Linde C. Dynamic changes in right ventricular pressures during haemodialysis
recorded with an implantable haemodynamic monitor. Nephrol Dial
Transplant 2006;21:176–83.
26. Allen LA, Metra M, Milo-Cotter O, et al. Improvements in signs and
symptoms during hospitalization for acute heart failure follow different
patterns and depend on the measurement scales used: an international,
prospective registry to evaluate the evolution of measures of disease severity
in acute heart failure (MEASURE-AHF). J Card Fail 2008;14:777–84.
27. Metra M, O’Connor CM, Davison BA, et al. Early dyspnoea relief
in acute heart failure: prevalence, association with mortality, and
effect of rolofylline in the PROTECT study. Eur Heart J 2011;32:
1519–34.
JACC Vol. 63, No. 13, 2014
April 8, 2014:1246–52
28. Matsumoto Y, Mori Y, Kageyama S, et al. Spironolactone reduces
cardio- and cerebrovascular morbidity and mortality in hemodialysis
patients. J Am Coll Cardiol 2013;63:528–36.
29. Ito Y, Mizuno M, Suzuki Y, et al. Long-term effects of spironolactone
in peritoneal dialysis patients. J Am Soc Nephrol 2013 Dec 12 [E-pub
ahead of print].
30. Safley DM, Awad A, Sullivan RA, et al. Changes in B-type natriuretic
peptide levels in hemodialysis and the effect of depressed left ventricular
function. Adv Chronic Kidney Dis 2005;12:117–24.
31. Maisel AS, Katz N, Hillege HL, et al. Biomarkers in kidney and heart
disease. Nephrol Dial Transplant 2011;26:62–74.
32. Wang AY, Sanderson JE. Treatment of heart failure in long-term
dialysis patients: a reappraisal. Am J Kidney Dis 2011;57:760–72.
33. Schwartzenberg S, Redfield MM, From AM, Sorajja P, Nishimura RA,
Borlaug BA. Effects of vasodilation in heart failure with preserved or
reduced ejection fraction: implications of distinct pathophysiologies
on response to therapy. J Am Coll Cardiol 2012;59:442–51.
34. Redfield MM, Jacobsen SJ, Burnett JC Jr., Mahoney DW, Bailey KR,
Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction
in the community: appreciating the scope of the heart failure epidemic.
JAMA 2003;289:194–202.
35. Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with
preserved ejection fraction. Circ Heart Fail 2010;3:588–95.
36. Pang PS, Tavares M, Collins SP, et al. Design and rationale of the
URGENT dyspnea study: an international, multicenter, prospective
study. Am J Ther 2008;15:299–303.
37. 2012 Atlas of CKD & ESRD. United States Renal Data System.
Available at: http://www.usrds.org/atlas12.aspx. Accessed February 3,
2014.
38. de Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA,
Laragh JH. Effect of growth on variability of left ventricular mass:
assessment of allometric signals in adults and children and their capacity
to predict cardiovascular risk. J Am Coll Cardiol 1995;25:1056–62.
39. Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of obesity
on left ventricular mass and geometry. The Framingham Heart study.
JAMA 1991;266:231–6.
Key Words: chronic kidney disease - classification
ESRD - fluid overload - heart failure.
-
dyspnea
-
APPENDIX
For a complete list of the ADQI Consensus Group members, as well as
supplemental information, please see the online version of this article.