* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download MULTIDRUG-RESISTANT TUBERCULOSIS: What Nurses Should
West Nile fever wikipedia , lookup
Bioterrorism wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Marburg virus disease wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Onchocerciasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Neonatal infection wikipedia , lookup
Hepatitis C wikipedia , lookup
Sarcocystis wikipedia , lookup
Visceral leishmaniasis wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Leptospirosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Schistosomiasis wikipedia , lookup
Trichinosis wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
History of tuberculosis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Mycobacterium tuberculosis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
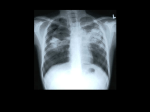
MULTIDRUG-RESISTANT TUBERCULOSIS: What Nurses Should Know Felissa R. Lashley, RN, PhD, FAAN, FACMG Professor, College of Nursing, and Interim Director, Nursing Center for Bioterrorism and Infectious Disease Preparedness, College of Nursing Rutgers, The State University of New Jersey This module is designed to highlight important information about multidrug resistant tuberculosis (MDR-TB). MDR-TB is also considered to be a potential agent for bioterrorism and is considered as a possible Category C bioterrorism agent by the Centers for Disease Control and Prevention (CDC). This module was supported in part by USDHHS, HRSA Grant No. T01HP01407. Multidrug-Resistant Tuberculosis (MDR-TB) MDR-TB is considered as a Category-C biological agent in regard to its potential for use in bioterrorism by the CDC. These agents are considered as possible emerging public health threats and are considered as such in the module on Biological Weapons: Essential Information on Category C Agents. XDR-TB (extensively resistant tuberculosis) refers to cases of TB that are resistant to isonazid , rifampin, the second line drugs, the fluoroquinolones, and at least one of three injectable drugs. i.e. amikacin. Objectives Describe the signs and symptoms commonly associated with pulmonary TB. Identify persons at high risk for MDR-TB. Describe reasons for development of drug resistance in the treatment of TB. Identify possible clinical outcomes after acquisition of Mycobacterium tuberculosis. Identify appropriate infection control for persons with MDR-TB. Definition MDR-TB is defined as a case of TB caused by a strain of M. tuberculosis that is resistant to two or more antituberculosis drugs. Some define MDR-TB as a case of TB caused by a strain of M. tuberculosis that is resistant to isoniazid and rifampin. Etiology Both tuberculosis infection and tuberculosis (TB) are due to the tubercle bacilli. The most common in the US is Mycobacterium tuberculosis. M. tuberculosis is a nonmotile, non-spore forming rod shaped bacillus with no capsule. It does not produce toxin. It is known as acid fast because of staining characteristics. It can survive for long periods under adverse conditions. Description Infection with M. tuberculosis can be pulmonary or extrapulmonary. Pulmonary TB is the most common form in developed countries. In extrapulmonary TB, signs and symptoms depend on the affected organ system as well as systemic symptoms. Major concerns about MDR-TB arose in the early 1990s when nosocomial outbreaks occurred. Concerns about XDR-TB arose in about 2000, and appears most prevalent in South Africa, parts of Asia especially South Korea and Eastern Europe. Epidemiology MDR-TB is particularly common in: Resource poor areas Global "hot spots" such as some areas in the former Soviet Union, India, the Dominican Republic, Ivory Coast, and others Congregate settings such as prisons or long-term care facilities Epidemiology cont.-2 In practice, MDR-TB develops either because the person is infected initially with a: Drug-resistant strain (primary), or Susceptible strain that becomes resistant (secondary) Primary resistance would be most likely in regard to bioterrorism use. Epidemiology cont.-3 Reasons for secondary resistance are numerous and complex: Wrong drugs used in an improper way Failure to assess drug susceptibility patterns of the organism A large bacterial load, especially in the case of cavitation Poor adherence to the treatment regimen Epidemiology cont.-4 TB (including MDR-TB) and HIV co-infections are relatively common globally and each condition adversely affects the other. In the US in 2007, the overall number of TB cases reported in the U.S. was 13, 293. In the U.S. between 1993 and 2006, 49 cases of XDR-TB were reported, and in 2006, 116 cases of MDR-TB were reported. The overall case rate was 4.4 cases per 100,000 population. U.S. born blacks and foreign born persons account for a disproportionate number of cases. Epidemiology cont.-5 TB remains a major global problem. Each year about 2 million people die of TB each year worldwide. In 2006, WHO reported 9.2 million new cases of TB. In the U.S., 49 cases of XDR-TB were reported between 1993 and 2006. Transmission Person-to-person through inhalation of droplet nucleii Infected person usually coughs or sneezes and projected infected droplet nucleii into the air Ingestion of contaminated food or water (rare in US) Direct inoculation is rare although infection through transplants has occurred. Outcomes of Contact with M. tuberculosis Many factors determine outcome such as: Host susceptibility, such as genetic factors and immune status Organism characteristics, such as virulence Environment, such as length of time and proximity of contact between the susceptible person and the person with TB Sequence of Events in Brief: After M. tuberculosis enters the body, possible events include: No infection Tuberculous infection Remains dormant in latent form (90%) Progression to clinical disease (10%) Within a year or two (5%) Years later (5%) Thus, persons may have: Latent TB infection in which persons are infected with tubercle bacilli but are not infectious to others nor show clinical symptoms but do usually have a positive reaction to the tuberculin skin test but usually negative chest radiograph. They may be candidates for preventive drug therapy, OR Active TB in which they are infected with tubercle bacilli, usually have positive sputum smears and cultures, usually have a positive reaction to the tuberculin skin test, usually have clinical symptoms, and may be infectious to others before treatment is effective. Clinical Manifestations MDR-TB are or are not clinically distinguishable from drug-susceptible TB at the outset. Signs, symptoms, and radiological findings are similar initially to drugsusceptible TB. In the non-bioterrorist setting, reasons to suspect drug resistance are: A history of previously treated TB in a person presenting with active TB High community rates of drug resistant TB Positive HIV status High likelihood of exposure to nosocomial, prison or community sources of MDR-TB The infected person is from a country with a high MDR-TB rates Contacts with persons with MDR-TB Infected person has received inadequate treatment regimens for >2 weeks Smears or cultures remain positive despite 2 months of treatment for TB Symptoms of Pulmonary TB include: Cough (usually productive and maybe bloody) Low-grade fever Sweating Chills at night Fatigue Malaise Anorexia Weight loss Dull, aching chest pain or tightness Symptoms of extrapulmonary TB depend on the organ system involved but may include systemic symptoms such as malaise Diagnosis generally consists of: Medical history, Clinical signs and symptoms, Chest x-ray for pulmonary TB, Sputum smear and/or culture for acid-fast bacilli, and possibly A tuberculin skin test. Diagnosis notes Tuberculin skin test with purified protein derivative as screen; anergy may be seen in elderly and the immunosuppressed. Chest x-ray or radiograph of extrapulmonary site shows characteristic findings of abnormalities in apical or posterior segments of upper lobe or superior segments of lower lobe but is not used to confirm diagnosis of pulmonary TB. Appearance may be unusual in HIV-positive persons Sputum smears and cultures for tubercle bacilli. Treatment Initial non-MDR-TB therapy in drugsusceptible disease calls for 8 weeks of therapy with isoniazid, rifampin, pyrazinamide, and ethambutol followed by a continuation regimen of isoniazid and rifampin for 18 more weeks as the most frequent option. Aggressive treatment is suggested. Treatment cont.-2 Usually the initial regimen for MDRTB will consist of at least 3 TB drugs the patient has not used before (a single drug should never be added) and as many as 6 drugs. There are detailed dosages and possible options available depending on many factors. Newer guidelines should always be consulted. Treatment cont.-3 MDR-TB treatment depends on the drug resistance pattern present: It may include directly observed therapy Occasionally, surgical resection may be used in treatment Detailed information about management options are given in the references (see CDC reference in particular) Prevention MDR-TB may be prevented by clinicians: Choosing the appropriate therapeutic regimen based on clinical, microbiological, pathological, radiological and epidemiological information, and Assuring a regimen with the highest likelihood of adherence to therapy. Management, including Infection Control Teaching the patient and family about preventing transmission, especially etiquette and hygiene, use of masks where indicated, and handwashing. Isolation precautions are usually needed until there have been 3 negative sputum cultures. Ascertaining likelihood of adherence and using measures to enhance adherence. Promptly isolate persons suspected or known to have TB. Use appropriate infection control. MDR-TB For sputum positive pulmonary MDR-TB, appropriate infection control includes: infection control Special airborne precautions, including isolation in a negative pressure isolation room, and appropriate air handling. Staff should wear appropriate personal protection devices, and close door behind them. Staff should remove personal protection devices before exiting anteroom and sanitize hands after leaving room. See infection control module details, and CDC, (2005). Guidelines for preventing the transmission of My cobacterium, 2005. Murphy, R.A. (2008) The emerging crisis of drug-resistant tuberculosis in South Africa: Lessons from New York City. Clinical Infectious Diseases 46, 1729-1732 For sputum positive pulmonary MDR-TB, appropriate infection control includes: Special airborne precautions, including isolation in a negative pressure isolation room. Staff should wear powered-air purifying respirators (PAPRs), and close door behind them. Staff should remove PAPR before exiting anteroom and sanitize hands after leaving room. See infection control module for details or CDC (2005). MDR-TB References CDC. (2003). Treatment of TB. American Thoracic Society, Centers for Disease Control and Prevention, and Infectious Disease Society of America. MMWR, 52 (RR-11),1-88. Lashley, F.R., & Durham, J.D. (Eds.). (2007). Emerging infectious diseases: Trends and issues. 2nd edition. New York: Springer Publishing Co. Mukherjee, J.S., Rich, M.L., Socci, A. R. et al. (2004). Programers and principles in treatment of multidrugresistant tuberculosis. Lancet, 363, 474-481. CDC (2008). Trends in tuberculosis- United States, 2007. MMWR 57, 281-285. CDC (2005) Guidelines for preventing the transmission of tuberculosis; healthcare settings, 2005. MMWR,54,1-141. Yew, W.W. and Leung, C.C. (2008) Management of multidrug-resistant tuberculosis: Update 2007. Respirology, 13, 21-46.