* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Week 5 Lecture 1 Chapter 4 The Tissue Level of Organization
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Artificial cell wikipedia , lookup
Microbial cooperation wikipedia , lookup
Chimera (genetics) wikipedia , lookup
State switching wikipedia , lookup
Neuronal lineage marker wikipedia , lookup
Hematopoietic stem cell wikipedia , lookup
Nerve guidance conduit wikipedia , lookup
List of types of proteins wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Cell theory wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
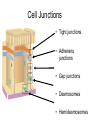
Week 5 The Tissue Level of Organization • Group of similar cells – common embryonic origin – common function • Histology – study of tissues • Pathologist – looks for tissue changes that indicate 4 Basic Tissues (1) • Epithelial Tissue – covers exposed surfaces ( skin ) – lines hollow organs, internal passageways and ducts ( digestive tract, urinary tract, reproductive) – forms glands- when cells sink under the surface • Connective Tissue – material found between cells – supports and binds structures together – stores energy as fat – provides immunity to disease 4 Basic Tissues (2) • Muscle Tissue – cells shorten in length producing movement • Nerve Tissue – cells that conduct electrical signals – detects changes inside and outside the body – responds with nerve impulses Biopsy • Removal of living tissue for microscopic examination – surgery – needle biopsy • Useful for diagnosis, especially cancer • Tissue preserved, sectioned and stained before microscopic viewing Maintaining the integrity of Epithelium To be effective as a barrier, an epithelium must form a complete cover or lining. 3 factors help maintain the integrity of the epithelium 1) 2) 3) Intercellular connection -Cell adhesion molecule, cell junctions Attachment to basement membrane – 2 layers, clear and dense layer Maintenance and repair –epithelium live hard lives. Exposed to enzymes, toxic chemicals, bacteria, and mechanical abrasions. Stem cells called GERMATIVE cells divide continually. Cell Junctions • Tight junctions • Adherens junctions • Gap junctions • Desmosomes • Hemidesmosomes Tight Junctions • Watertight seal between cells. Preventing passage of water and solutes • Plasma membranes fused with a strip of proteins • Common between cells that line GI and bladder • Don’t want acids, enzymes and waste leaking. Adherens Junctions • Holds epithelial cells together • Structural components – plaque = dense layer of proteins inside the cell membrane – microfilaments extend into cytoplasm – integral membrane proteins connect to membrane of other cell Desmosomes • Resists cellular separation, cell disruption, twisting, compression. • Similar structure to adherens junction except intracellular intermediate filaments cross cytoplasm of cell • Found in superficial layer of skin. (Skin peels when damages.) Gap Junctions • Tiny space between plasma membranes of 2 cells • Crossed by protein channels called connexons forming fluid filled tunnels allowing sugars, amino acids, and electrolytes to pass. • Cell communication rapidly with ions & small molecules • Muscle and nerve impulses spread from cell to cell – heart and smooth muscle of gut Epithelial Tissue -- General Features • Closely packed cells forming continuous sheets held together by cell junctions. • Cells sit on basement membrane • Apical (upper) free surface • Avascular---without blood vessels – nutrients diffuse in from underlying connective tissue • Good nerve supply • Rapid cell division if damaged via stem cells • Covering- line all passage ways that come into contact with outside world. Skin, Digestive, respiratory, reproductive, urinary, brain, blood vessels, heart. Functions • Physical protection – protects exposed and internal surfaces from abrasions, dehydration, and destruction from chemical agents. • Absorption – The lining of the gut and respiratory tract allow for nutrients to be absorbed from the gut and the exchange of gases between air in lungs and blood. • Excretion- The unique lining of the kidney tubules makes the excretion and concentration of excretory products in the urine possible. • Produces secretions – Glandular epithelial is adapted for secretory activity (hormones, mucus, digestive juices, and sweat) • Provides sensation – good nerve supply- sensory nerves of eyes, ears, nose, skin. • Specialized Epithelium – a) Microvilli – absorption/secretion – found in digestive and urinary tracts b) Cilia – Respiratory tracts, the synchronized beating moves mucous up from lungs to throat. Basement Membrane • Basal lamina – from epithelial cells – collagen fibers • Reticular lamina – secreted by connective tissue cells – reticular fibers-strength • holds cells to connective tissue • guide for cell migration during development Types of Epithelium • Covering and lining epithelium – epidermis of skin – lining of blood vessels and ducts – lining respiratory, reproductive, urinary & GI tract • Glandular epithelium – secreting portion of glands – thyroid, adrenal, and sweat glands Classification of Epithelium • Classified by arrangement of cells into layers – simple = one cell layer thick. Secretion or absorption (intestine ,lungs) – stratified = many cell layers thick. Located where protection from mechanical or chemical stresses are needed. ( skin , mouth ) – pseudostratified = single layer of cells where all cells don’t reach apical surface • nuclei at found at different levels so it looks multilayered • Classified by shape of surface cells – squamous =flat – cuboidal = cube-shaped – columnar = tall column – transitional = shape varies with tissue stretching Simple Squamous Epithelium • Single layer of flat cells – lines blood vessels (endothelium heart chambers), body cavities (mesothelium :pleura, pericardium, peritoneum) – very thin --- controls diffusion, osmosis and filtration – nuclei centrally located • Cells in direct contact with each other • Good for gas exchange at lungs(alveoli), absorption at intestines, and re-absorption loop of henley at kidneys Examples of Simple Squamous • Surface view of lining of peritoneal cavity • Section of intestinal showing serosa Simple Cuboidal Epithelium • • • • Single layer of cube-shaped cells viewed from the side Nuclei round and centrally located Lines tubes of kidney – proximal and distal tubules Absorption or secretion Example of Simple Cuboidal • Sectional view of kidney tubules Nonciliated Simple Columnar • Single layer rectangular cells • Unicellular glands =goblet cells secrete mucus – lubricate GI, respiratory, reproductive and urinary systems • Microvilli = fingerlike cytoplasmic projections – for absorption in GI tract (stomach to anus) Ex. Nonciliated Simple Columnar • Section from small intestine Ciliated Simple Columnar Epithelium • Single layer rectangular cells with cilia • Mucus from goblet cells moved along by cilia – found in respiratory system and uterine tubes Ex. Ciliated Simple Columnar • Section of uterine tube Stratified Squamous Epithelium • Several cell layers thick • Surface cells flat. Located where mechanical and chemical stresses are severe • Keratinized = surface cells dead and filled with keratin. This layer is tough and water resistant. – skin (epidermis) • Nonkeratinized- resists abrasions, but will dry out if not kept moist. No keratin in moist living cells at surface – mouth, vagina Example of Stratified Squamous • Section of vagina Papanicolaou Smear (Pap smear) • Collect sloughed off cells of uterus and vaginal walls • Detect cellular changes (precancerous cells) • Annually for women over 18 or if sexually active • HPV – 80 % of women over 50 have it. • Low risk- irregular cells, high risk- leads to cervix cancer. • Guardasil – protects only 4 out of 10 strains. Stratified Cuboidal Epithelium • Multilayered • Surface cells cuboidal – rare (only found in sweat gland ducts & male urethra) Stratified Columnar Epithelium • Multilayered • Surface cells columnar • Rare (very large ducts & part of male urethra) Transitional Epithelium • Multilayered • Surface cells varying in shape from round to flat if stretched • Lines hollow organs that expand from within (urinary bladder) Pseudostratified Columnar • Single cell layer • All cells attach to basement membrane but not all reach free surface • Nuclei at varying depths • Respiratory system, male urethra & epididymis Glandular Epithelium • Derived from epithelial cells that sank below the surface during development • Exocrine glands – cells that secrete---sweat, tears, milk, ear wax, saliva, digestive enzymes onto free surface of epithelial layer – connected to the surface by tubes (ducts) • Endocrine glands – ductless glands (thyroid, pituitary, adrenal glands) – secrete hormones into the bloodstream – hormones help maintain homeostasis – Sjorgens syndrome – autoimmune disease of exocrine glands. Dry eyes, mouth Methods of Glandular Secretion • Merocrine (part)-- Most glands – cells release their products by exocytosis---saliva, digestive enzymes & sweat • Apocrine (off) – milk – upper part of cell possibly pinches off & dies – Holocrine (entire) -- oil gland – whole cells die & rupture to release their products Exocrine glands- 3 types • 1) Serous Glands – Secretes a watery solution that contains enzymes. Parotid gland. • 2) Mucous glands –secrete mucins that hydrate to form mucous. Salivary glands, submucosal glands of the small intestine. • 3) Mixed glands- submandibular Week 5 Connective Tissues • Cells rarely touch due to extracellular matrix • Matrix (fibers & ground substance secreted by cells • Consistency varies from liquid, gel to solid • Good nerve & blood supply except cartilage & ligaments) Extracellular Matrix The ties that bind us together – healthy ECM means reduced pain/degenerative changes and increased function Support for Extra-Cellular (Connective) Tissues Unhealthy ECM is found in patients that: – Are suffering from soft-tissue injury – Routinely suffer from repetitive injury – Have difficulty maintaining alignment – Are experiencing degradation of connective tissues Down-regulate the expression collagen-damaging enzymes (MMPs) to support balanced healing of extracellular matrix tissues Connective Tissues = Extracellular Matrix tendons joints ligaments cartilage fascia http://images.google.com/imgres?imgurl=http://www.pride.hofstra.edu/~akroto1/img009.jpg&imgrefurl=http://www.pride.hofstra.edu/~akroto1/bioengg.html&h=450&w=600&sz=75&hl=en&start=3& tbnid=9BMB7hzszEIkUM:&tbnh=101&tbnw=135&prev=/images%3Fq%3Dextracellular%26gbv%3D2%26hl%3Den Extracellular matrix is the structural scaffold for the cells and is the defining feature of connective tissue Non-cellular components • • • • Heparan sulfate • Chondroitin sulfate • Keratan sulfate • Laminin • Cellular Components • Fibroblasts • Chondrocytes • Osteoblasts Hyaluronic Acid Collagen Fibronectin Elastin The extracellular matrix is composed of tissues that serve multiple purposes “The ECM is a conglomerate of substances in which biochemicals and properties for of the connective tissues that Abiophysical complex weballow that construction of a flexible network that •integrates Provideinformation adhesion toloading cellsand from it into mechanical capacities…It •converts Act as a structural scaffold serves as a scaffold for adhesion of cells •mediated Actively participate in intracellular signaling by integrins, dystroglycan, and at the cell surface and loading of •proteoglycans Translates mechanical into cellular response tyrosine kinase receptors. The interaction between the ECM and the adhesion molecules leads to activation of intracellular signaling pathways and cytoskeletal rearrangement.” http://content.answers.com/main/content/img/McGrawHill/Encyclopedia/images/ Kjaer, M. Physiol. Rev. 84:649-698, 2004. CE157300FG0010.gif Extracellular matrix tissues are degraded after injury physiology of an injury Prostaglandins and thromboxanes are created which signal pain and induce inflammation Chondrocytes in the extracellular matrix release matrix metalloproteinase enzymes (MMPs) into the area of injury MMPs degrade collagens, elastins, basement membranes Down-regulate the expression of MMP-13 support connective tissue • “MMP-1 and MMP-13 are collagenolytic MMPs that have been most strongly associated with cartilage collagenolysis” • “chondrocytes are stimulated to secrete elevated levels of MMPs that, once activated, mediate the proteolysis of tendon, bone and cartilage.” Litherland et al., JBC, Papers in press, March 10, 2008 to Matrix metalloproteinases digest collagen and connective tissue Chondrocyte MMP-13 MMPs further degrade collagen tissue during injury or inflammation Collagen Triple Helix MMP-13 Modulate expression of MMPs to support healthy remodeling of connective tissue MMP-1 MMP-13 MMP- 2 MMPs are released from the chondrocyte in response to injury or inflammation MMP-9 Clinical conditions associated with expression of MMPs Periodontal disease Tendon injury Fracture healing increased MMPs Wound repair Degenerative discs MMPs are a primary target to address tendonitis and connective tissue disorder Am J Sports Med. 2007 May;35(5):763-9. Epub 2007 Feb 9. Links Matrix metalloproteinase inhibitors prevent a decrease in the mechanical properties of stress-deprived tendons: an in vitro experimental study. Arnoczky SP, Lavagnino M, Egerbacher M, Caballero O, Gardner K. “An increase in matrix metalloproteinases (MMPs) and the resulting degradation of the extracellular matrix have been implicated in the pathogenesis of tendinopathy. Matrix metalloproteinase inhibitors prevented the activation of MMP-13 and significantly inhibited pericellular matrix degeneration and the loss of material properties associated with stress “Matrix metalloproteinase inhibitors supportiverole role deprivation. Matrix metalloproteinase inhibitorsmay mayplay play aa supportive treatment of tendinopathy by limiting the MMPin in thethe treatment of tendinopathy by limiting the MMP-mediated degradation the extracellular mediatedof degradation ofmatrix.” the extracellular matrix.” Nutritional strategy to balance the expression of MMPs Poly(ADP-ribose) polymerase inhibition reduces TNF-induced inflammatory response in rheumatoid synovial fibroblasts. García S, Bodaño A, Pablos JL, Gómez-Reino JJ, Conde C. Comparative effects of 2 antioxidants, selenomethionine and onPARP catabolic and either anabolic “Weepigallocatechin-gallate, show, for the first time, that inhibition withgene expression of articular chondrocytes. specific inhibitors or by siRNA transfection significantly reduced Andriamanalijaona R, chemokine Kypriotou expression M, Baugé C, Legendre F, TNF-induced cytokine and in Renard fibroblastE,like Raoudi M, Boumediene K, Gatto H, Monginoux P, Pujol JP. synoviocytes cells from RA patients. PARP inhibitors also Laboratory of Connective Tissue Biochemistry, Faculty of Medicine, 14032 Caen Cedex, decreased TNF-induced RA FLS proliferation…PARP inhibition France. reduced TNF-induced JNK the phosphorylation and AP-1 (Se-met) and OBJECTIVE:. To determine effects of selenomethionine and epigallocatechinNFkappaB binding activities were activation partially of impaired by treatment gallate (EGCg) on gene expression, mitogen-activating kinases, and DNA binding nuclearinhibitors factor-kappaB (NF-kappaB) and apolipoprotein-1 (AP-1) in articular chondrocytes. withofPARP or by PARP-1 knockdown…PARP inhibition METHODS: Chondrocytes, cultured in low-oxygen tension, were pretreated with Lreduces the production of inflammatory mediators and the selenomethionine or EGCg for 24 h, followed by interleukin 1 (IL-1beta) for 1 h (nuclear and proliferation of RA FLS (in response to TNF) suggesting that PARP cytoplasmic extracts) or 24 h (RNA extraction). Reverse transcription-polymerase chain inhibitors have therapeutic benefits in RA.” reactioncould was performed to determine mRNA levels of matrix metalloproteinases (MMP-1, -3, Ann13), Rheum Dis. 2007 21 aggrecanases (-1, Sep -2), IL-1beta, inducible nitric oxide synthase, cyclooxygenases (-1, -2), • Hops & Berberine to modulate MMP-13 • Selenium to address MMP-1 & MMP-2 • Folic acid to impact MMP-9 • Niacinamide to address tissue-damaging PARS type II collagen and aggrecan, and transforming growth factor-beta (TGF-beta1, -2, -3) and their receptors I and II. Activity of mitogen-activating protein kinases (MAPK) was assayed by Western blot and AP-1/NF-kB DNA binding by electrophoretic mobility shift assay. RESULTS: Pretreatment with 0.5 microM Se-met prevented IL-1beta-induced MMP-1 and aggrecanase-1 expression, and reduced the IL-1(10ng/ml) ( g/ml) - + 1 + 0.1 + 0.05 + B CT • 1) Fibrous-CT Proper • A) Loose (areolar) • B) Adipose • C) Reticular • D) Dense 1) Irregular 2) Regular a) collagenous b) elastic • 2) BONE a) Compact b) Spongy • 3) Cartilage a) Hyaline b) fibrocartilage c) elastic • 4) Blood CT • Situated throughout the body but never exposed to outside environment. • Many CT are highly vascular except ligaments and cartilage. • Has sensory receptors for pain, temperature and pressure. • FUNCTIONS • 1) structural framework – bones, muscles, tendons, ligaments • 2) transports fluids and dissolved materials – blood • 3) protects delicate organs • 4) stores energy reserves especially in the form of lipids – adipose • 5) defends body from invading microorganisms – WBC’s • 3 components 1) specialized cells, 2) extracellular proteins 3) ground substance #’s 2 & 3 = MATRIX 1st type of CT to appear in embryo is MESENCHYME. It has STEM CELLS which gives rise to all other CT’s. Blast type cells = retain ability to divide & produce matrix (fibroblasts- most abundant and permanent resident of CT, it’s always present, secretes hyaluronan which is the cement that holds epithelial cells together, chondroblasts, & osteoblasts) Cyte type cells = mature cell that can not divide or produce matrix (chondrocytes & osteocytes) Macrophages develop from monocytes ( mesenchymal cells- stem cells ) engulf bacteria & debris by phagocytosis Plasma cells develop from B lymphocytes produce antibodies that fight against foreign substances Mast cells (WBC- produces heparin, histamine, serotonin) produce histamine that dilate small BV Adipocytes (fat cells) store fat Fibroblasts, adipocytes, mesenchymal permanent residents. Connective Tissue Ground Substance • Supports the cells and fibers • Helps determine the consistency of the matrix – fluid, gel or solid • Contains many large molecules – hyaluronic acid is thick, viscous and slippery – condroitin sulfate is jellylike substance providing support – adhesion proteins (fibronectin) binds collagen fibers to ground substance Types of Connective Tissue Fibers • Collagen (25% of protein in your body TENDONS & LIGAMENTS) – tough, resistant to pull, yet pliable – formed from the protein collagen • Elastin (lungs, blood vessels, ear cartilage) – smaller diameter fibers formed from protein elastin surrounded by glycoprotein (fibrillin) – can stretch up to 150% of relaxed length and return to original shape ( Diabetes, Glucose ) • Reticular (spleen, lymph nodes, liver) – thin, branched fibers that form framework of organs – Stabilize organs, blood vessels/nerves despite gravity – Similar to collagen but arranged differently, not aligned Marfan Syndrome • Inherited disorder of fibrillin gene • Abnormal development of elastic fibers • Tendency to be tall with very long legs, arms, fingers and toes • Life-threatening weakening of aorta may lead to rupture or aneurism. Mature Connective Tissue • CT proper – many cells with fibers in ground substance • Loose connective tissue – adipose or fat • Dense connective tissue – tendons • Supporting CT – less diverse cells more dense fibers • Cartilage • Bone • Fluid CT – Contains dissolved proteins • Blood • Lymph Loose Connective Tissues • Loosely woven fibers throughout tissues. • The PACKING MATERIAL of the body. • Surrounds and supports blood vessels, nerves, store lipids, route for diffusion, and fills spaces between organs. • Types of loose connective tissue – areolar connective tissue – adipose tissue – reticular tissue Areolar Connective Tissue • Cell types = fibroblasts, plasma cells, macrophages, mast cells and a few white blood cells • All 3 types of fibers present: collagen, elastin, reticular • Gelatinous ground substance- can distort without damage b/c loosely arranged fibers. Forms layer that separates skin from muscle. • Good blood supply so common injection site for drugs. Areolar Connective Tissue • Black = elastic fibers, • Pink = collagen fibers • Nuclei are mostly fibroblasts Adipose Tissue • • • • • • Peripheral nuclei due to large fat storage droplet Deeper layer of skin, organ padding, yellow marrow Reduces heat loss, energy storage, protection Stores toxins- insects & pesticides Fat cells increase until puberty Liposuction is temp fix b/c mesenchyme cells regenerate fat cells Reticular Connective Tissue • Network of fibers & cells that produce framework of organ • Holds organ together (liver, spleen, lymph nodes, bone marrow) Dense Connective Tissue • More fibers present but fewer cells • Types of dense connective tissue – 1) dense regular connective tissue – tendons, ligaments – 2) dense irregular connective tissue- Dermis, scars, deep fascia, surrounds organs like liver and spleen – 3) elastic connective tissue – walls of arteries, spinal ligaments Dense Regular Connective Tissue • Collagen fibers in parallel bundles with fibroblasts between bundles of collagen fibers • White, tough and pliable when unstained (forms tendons, ligaments, aponeurosis) Dense Irregular Connective Tissue • • • • Collagen fibers are irregularly arranged (interwoven) Tissue can resist tension from any direction Found in Liver, kidneys, spleen. Very tough tissue -- white of eyeball, dermis of skin Elastic Connective Tissue • Branching elastic fibers and fibroblasts • Can stretch & still return to original shape-walls of arteries • Lung tissue, vocal cords, ligament between vertebrae • Elastin –vs- Collagen in certain ligaments. Spine/knee Cartilage • Network of fibers in rubbery ground substance. Firm gel from polysacharide derivative called chondroitin sulfate. • Resilient and can endure more stress than loose or dense connective tissue • It’s avascular. Chondrocytes produce chemicals that discourage their growth called anti-angiogenesis factor • So all exchange of nutrients and wastes products must occur by diffusion. • Types of cartilage – hyaline cartilage – fibrocartilage – elastic cartilage Hyaline Cartilage • • • • Bluish-shiny white rubbery substance Chondrocytes sit in spaces called lacunae No blood vessels or nerves so repair is very slow Reduces friction at joints as articular cartilage Fibrocartilage • Many more collagen fibers causes rigidity & stiffness • Strongest type of cartilage (intervertebral discs) Elastic Cartilage • Elastic fibers help maintain shape after deformations • Ear(Eustachian tube), nose, vocal cartilages Bone (Osseous) Tissue • Spongy bone- found in epiphysis- framework for blood production – sponge-like with spaces and trabeculae – trabeculae = struts of bone surrounded by red bone marrow – no osteons (cellular organization) • Compact bone- found in diaphysis- mineral reservoir – solid, dense bone – basic unit of structure is osteon (haversian system) • Protects, provides for movement, stores minerals, site of blood cell formation • 2/3 of matrix is calcium salts ( calcium phosphates) cement • 1/3 of matrix is collagen fibers= steel reinforcing rods Compact Bone • Osteon = lamellae (rings) of mineralized matrix – calcium & phosphate---give it its hardness – interwoven collagen fibers provide strength • Osteocytes in spaces (lacunae) in between lamellae • Canaliculi (tiny canals) connect cell to cell. They are the branching network for the exchange of materials between blood vessels and osteocytes. Normal Bone VS Osteoporotic Bone (Cod Fish Vertebra) Hyperkyphosis BLOOD • Temp – 100-100.5, PH 7.35- 7.45, Volume for males is 5-6 liters for females 4-5 liters. ( if one eats too much salt then one retains water. This increases blood volume which will increase blood pressure.) DIURETICS- get rid of excess water to decrease blood pressure. • 55% of total blood volume is PLASMA : matrix 91.5% water / 7% proteins / 1.5% solutes • 45% is RBC’s & WBC’s- formed elements • RBC- NO NUCLEUS. Does not use oxygen to make ATP. So it delivers all of it to lungs. PH of lung is basic so hemoglobin carries oxygen, but at cell blood is acidic so it is released. Blood • Connective tissue with a liquid matrix = the plasma • Cell types = red blood cells (erythrocytes), white blood cells (leukocytes) and cell fragments called platelets • Provide clotting, immune functions, carry O2 and CO2 Whole Blood Factors assisting with circulation • Skeletal muscle contraction and one way valves in the veins • Respiratory movements (Diaphragmatic) • Massage therapy • B-Vitamins • Omega 3’s • Red Wine Anatomy of an Artery Pathophysiology • • • • • • • • • • • 1. Vascular irritants irritate the tunica interna of the blood vessel. Vascular Irritants: a. Smoking b. Alcohol c. Fried foods d. Chemical produced during stress e. Caffeine f. Physical trauma g. Normal wear and tear (aging) (anti-oxidant vitamins improve circulation) h. Environmental toxins I. Homocysteine: intermediate chemical substance in the metabolism of the amino acid cysteine that is a strong vascular irritant. Folic acid, vitamin B12 and vitamin B6 will prevent the build up of homocysteine in the blood. • • Homocysteine • • Folic B12 B6 Acid Normal Artery VS Atherosclerotic Artery Blocked Artery Balloon Angioplasty and Stent Balloon Catheter and Stent Collateral Circulation • Alternate routes of blood flow developed primarily within the arterial system which help to compensate for atherosclerosis and arteriosclerosis in the body. Collateral circulation develops with time and exercise. High Density Lipoproteins • High Density Lipoproteins/ HDL’s (Good) • • cholesterol Tissues --------------> Liver Low Density Lipoproteins • Low Density Lipoproteins/ LDL’s (Bad) • • cholesterol Liver -----------------> Tissues Lymph • Interstitial fluid being transported in lymphatic vessels • Contains less protein than plasma • Move cells and substances (lipids) from one part of the body to another • Lymph vessels return lymph to larger veins near the heart. • Recirculation of fluid from the cardiovascular system to the interstitial fluid to the lymph back to the cardiovascular system. Wastes and toxins are removed, alerts immune system of infections. Microcirculation The Lymphatic System • The Lymphatic system is a separate and parallel circulatory system designed to: • a) retrieve fluids filtered out of blood vessels and return it back to the general circulation • b) perform important immune system functions • c) absorb dietary fats and fat soluble nutrients from the gastro-intestinal tract The lymphatic system absorbs fluid, macromolecules, microorganisms, toxins, waste products and foreign substances from the interstitial tissue. Numerous substances (electrolytes, proteins, hormones, toxins, debris) and immunocompetent cells (lymphocytes, macrophages) pass through the regional lymph nodes, where this fluid is filtered, purified and concentrated. The Lymphatic System Muscle • Cells that shorten, lengthen and remain same length • Provide us with motion, posture and heat • Types of muscle – skeletal muscle-voluntary - striated – cardiac muscle-involuntary -striated – smooth muscle- involuntary Skeletal Muscle • Cells are long cylinders with many peripheral nuclei • Visible light and dark banding (looks striated) • Voluntary or conscious control Cardiac Muscle • Cells are branched cylinders with one central nuclei • Involuntary and striated • Attached to and communicate with each other by intercalated discs and desmosomes Smooth Muscle • Spindle shaped cells with a single central nuclei • Walls of hollow organs (blood vessels, GI tract, bladder) • Involuntary and nonstriated Nerve Tissue • Cell types -- neurons and neuroglial (supporting) cells • Nerve cell structure – nucleus & long cell processes conduct nerve signals • dendrite --- signal travels towards the cell body • axon ---- signal travels away from cell body Membranes • Epithelial layer sitting on a thin layer of connective tissue (lamina propria) • Types of membranes – mucous membrane – serous membrane – synovial membrane – cutaneous membrane (skin) Mucous Membranes • Lines a body cavity that opens to the outside – mouth, vagina, anus etc • Epithelial cells form a barrier to microbes • Tight junctions between cells • Mucous is secreted from underlying glands to keep surface moist Serous Membranes • Simple squamous cells overlying loose CT layer • Squamous cells secrete slippery fluid • Lines a body cavity that does not open to the outside such as chest or abdominal cavity • Examples – pleura, peritoneum and pericardium – membrane on walls of cavity = parietal layer – membrane over organs in cavity = visceral layer Synovial Membranes • Line joint cavities of all freely movable joints • No epithelial cells---just special cells that secrete slippery fluid Tissue injury and repair • The first sign of healing is inflammation- Redness, swelling, warmth, pain. • The repair process is called regeneration • When there is an increase in pathogens, toxins, waste, this will stimulate the release of mast cells which will release histamines, heparin, and prostoglandins. • This will INCREASE the blood flow, pain, and increase vessel permeability. • This will INCREASE the temperature, oxygen and nutrients, and phagocytic activity and removal of toxins, and waste • The RESULT is REGENERATION. • Normal tissues are restored.