* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Is it safe to perform dental surgery using local anesthesia with
Cardiac contractility modulation wikipedia , lookup
Cardiovascular disease wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
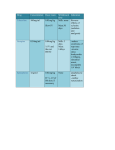
Remote ischemic conditioning wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Coronary artery disease wikipedia , lookup
Is it safe to perform dental surgery using local anesthesia with vasoconstrictor in coronary artery disease patients? 1. Introduction A best evidence topic was constructed according to a structured protocol. This protocol is fully described in the ICVTS [1]. 2. Clinical scenario Last week, a 60-year-old male with chronic coronary artery disease and arterial hypertension came to the cardiologist´s office with dental pain. His dentist asked the cardiologist´s advice as he was aware of the potential risk of local anesthesia with vasoconstrictor and cardiovascular side effects. The cardiologist himself was concerned about those effects of local anesthesia, and resolved to check the literature. 3. Three-part question In [patients with chronic coronary artery disease and need of dental surgery] does [local anesthesia with vasoconstrictor] have an acceptable [safety profile]? 4. Search strategy Search strategy using Medline from 1950 to June 2012 using the PubMed interface ((“Anesthesia, Dental” [Mesh] OR “Anesthesia, Local” [Mesh]) AND ‘’Dental Care for Chronically Ill” [Mesh])). The reference lists of key papers were searched and the ‘related articles’ function was utilized. 5. Search outcome One hundred and eighty-eight papers were found using the reported search on PubMed. From these, one paper was identified that provided the best evidence to answer the question. This is presented in Table 1. Table 1. Best evidence paper Author, date, journal, and country Study type level of evidence Patient group Outcome Key results Comments Neves et al., (2007), Single centre study Arq Bras Cardiol, Brazil, [2] Number of patients n = 62 Blood pressure, heart rate, ischemia and arrhythmias There was a rise in systolic and diastolic blood pressure from baseline to the procedure in both groups (14 mm Hg and 5 to 7 mmHg, respectively), when they were evaluated separately. No significant difference was found between the epinephrine and nonepinephrine groups. The study demonstrate that the use of vasoconstrictors in local dental anesthesia in patients with coronary heart disease is safe. Patient Randomized demographics controlled Age: 58.7 ± 8.8 trial (level 2) years [3] Male:Female: 51:11 Inclusion criteria: Clinical: patients with coronary artery disease (≥ 70% lumen stenosis) and exercise stress test positive for myocardial ischemia performed within less than three months in the absence of recent acute myocardial infarction Dental: fully or partially dentate requiring lower molar, premolar, or canine restoration Exclusion criteria: Authors’ conclusions: Blood pressure and heart rate did not differ, and there were no myocardial ischemia and cardiac arrhythmia with Mean heart rate epinephrinecontaining and did not differ epinephrine-free between the anesthetic epinephrine solution, in and nonpatients taking epinephrine drugs, the groups at baseline, during majority of whom were on betathe procedure blockers. (p = 0.1967), and over the 24 hours (p = 0.8417) Ten patients (17.9%) had ST segment depression greater than 1 mm from baseline, six (20.7%) in the non-epinephrine group (14.8%) Neoplasias, septicemia, pregnancy, unstable angina, and malignant hypertension Comorbidities: 24 patients (38.7%) were diagnosed with systemic hypertension and 24 with diabetes (38.7%). All patients continued their medication, especially betablockers (87.1%), lipidlowering agents (87.1%), antiplatelets (83.9%), and nitrates (54.8%) Angiography: Coronary angiography revealed singlevessel disease in seven (11.3%) patients, twovessel disease in 18 (29%) patients, and three-vessel disease in 37 (59.7%) patients. Study groups 2% lidocaine +1:100,000 epinephrine (epinephrine group): 30/62 2% lidocaine and four (14.8%) in the epinephrine group, but no significant difference was found between both groups (p = 0.731). Over the 24 hours, 17 patients (30.4%), ten (34.5%) belonging to the non-epinephrine group and seven (25.9%) belonging to the epinephrine group, experienced supraventricular extrasystoles (SVES) and/or ventricular extrasystoles (VES). During the procedure, however, only seven (12.5%) patients had arrhythmias, four (13.8%) in the nonepinephrine group and three (11.1%) in the epinephrine group, but no significant difference was found between the two groups (p = 1.00) without epinephrine (nonepinephrine group): 32/62 6. Results Neves et al [2] investigated patients with clinical symptoms of stable angina and on drug therapy, with angiographically proven coronary stenosis > 70% in at least one major artery and who underwent restorative dental treatment under anesthesia with and without a vasoconstrictor. Thirty patients were randomly assigned to receive 2% lidocaine and 1:100,000 epinephrine (epinephrine group), and 32 to receive 2% lidocaine without epinephrine (nonepinephrine group) for local anesthesia. All patients underwent 24-hour electrocardiography (Holter) and ambulatory blood pressure monitoring (ABPM). Each patient (30 in the epinephrine group and 32 in the non-epinephrine group) underwent a single restorative procedure under inferior alveolar anesthesia. In the epinephrine group, 15 patients were given one anesthetic cartridge (1.8 mL), and 15 patients, two anesthetic cartridges (3.6 mL). In the non-epinephrine group, 15 patients were given one cartridge, and 17 patients, two cartridges. Mean duration of procedures in both groups did not differ (p = 0.200). No clinical events were observed. When the epinephrine and non-epinephrine groups were compared in terms of blood pressure, no significant difference was found. The number of cartridges used, one or two, with or without epinephrine, did not differ between the two groups regarding mean systolic (p = 0.208) and diastolic (p = 0.118) blood pressure, and there was no influence by the use or not of beta-blockers. The Holter showed no difference in mean heart rate between both groups at baseline, during the procedure (p = 0.197), and over the 24 hours (p = 0.842). The number of cartridges used, with or without epinephrine did not change the results. The frequency of ST-segment depression had no significant difference between the two groups. All episodes occurred at least two hours after the dental procedure had been finished. Over the 24 hours, supraventricular and/or ventricular extrasystoles occurred in the nonepinephrine group (34.5%), and in the epinephrine group (25.9%) with no statistical significant difference. However, during the dental procedure, they occurred just in 13.8% (non-epinephrine group) and 11.1% (epinephrine group). 7. Clinical bottom line The use of vasoconstrictors in local dental anesthesia in patients with coronary heart disease seems to be safe. In one randomized clinical trial, no difference was observed in blood pressure, heart rate, myocardial ischemia and cardiac arrhythmias. References [1] Dunning J, Prendergast B, Mackway-Jones K. Towards evidence-based medicine in cardiothoracic surgery: best BETS. Interactive Cardiovascular Thoracic Surgery. 2003;2:405–9. [2] Neves RS, Neves IL, Giorgi DM, Grupi CJ, César LA, Hueb W et al. Arquivos Brasileiros de Cardiologia. 2007;88(5) :482-8. [3] Centre for Evidence Based Medicine. OCEBM 2011 Levels of Evidence System [Internet]. Oxford: University of Oxford, Oxford Centre for EvidenceBased Medicine; [updated 2012 Sep 13; cited 2012 Oct 2]. Available from: http://www.cebm.net/index.aspx?o=5653. ABSTRACT A best evidence topic in dentistry was written according to a structured protocol. The question addressed was whether in patients with chronic coronary artery disease and need of dental surgery, local anesthesia with vasoconstrictor has an acceptable safety profile. Altogether, 188 relevant papers were identified, of which one represented the best evidence to answer the question. The author, journal, date, country of publication and relevant outcomes are tabulated. The study comprised one randomized controlled trial. According to this trial, thirty patients were randomly assigned to receive 2% lidocaine and 1:100,000 epinephrine (epinephrine group), and 32 to receive 2% lidocaine without epinephrine (nonepinephrine group) for local anesthesia. When the epinephrine and non-epinephrine groups were compared in terms of blood pressure, no significant difference was found. The Holter showed no difference in mean heart rate between both groups at baseline, during the procedure (p = 0.197), and over the 24 hours (p = 0.842). The frequency of ST-segment depression had no significant difference between the two groups. Over the 24 hours, supraventricular and/or ventricular extrasystoles occurred in the nonepinephrine group (34.5%), and in the epinephrine group (25.9%) with no statistical significant difference. However, during the dental procedure, they occurred just in 13.8% (non-epinephrine group) and 11.1% (epinephrine group). We conclude that the use of vasoconstrictors in local dental anesthesia in patients with coronary heart disease seems to be safe. Key words: Coronary Artery Disease; Anesthesia, Vasoconstrictor Agents; Review; Best Evidence Topic Dental; Lidocaine;