* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Endocrine System
Neuroendocrine tumor wikipedia , lookup
Triclocarban wikipedia , lookup
Polycystic ovary syndrome wikipedia , lookup
Endocrine disruptor wikipedia , lookup
Mammary gland wikipedia , lookup
Breast development wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Glycemic index wikipedia , lookup
Hyperthyroidism wikipedia , lookup
Hypothalamus wikipedia , lookup
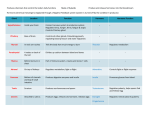
Endocrine System I’m hot, I’m cold, I’m fast, I’m slow. EMT-Paramedic Program The System Itself • The other regulating system of the body – Closely linked to nervous system • Uses glands and tissues • Via hormones, the system regulates: – – – – – – growth the use of foods for energy pH of body fluids fluid balance reproduction provides resistance to stress Hormones • Chemical messengers to either: – Body organs – Tissues – Or Both • Binding depends on: – Quantity – Quality of receptor sites • They may be divided into three groups: – Amines • Tyrosine, epi, norepi – Proteins • amino acids; insulin, GH, calcitonin, ADH, oxytocin – Steroids • cholesterol; cortisol, aldosterone, estrogen, progesterone, and testosterone Hormone Secretion • Negative feedback mechanism • Endocrine glands respond to blood level changes or other hormones present • Secretion of hormone until stimulus is negated or changed Pituitary “Master Gland” • Posterior holds hypothalamus hormones ADH and oxytocin • Anterior produces GH, TSH, ACTH, prolactin, FSH, LH Specific Hormones • ADH – maintains BP by reabsorption of water by kidney tubules and vasoconstriction • Oxytocin – stimulates contraction of uterus and release of milk Thyroid Stimulating Hormone Specific Hormones Growth Hormone Anterior Pituitary Adrenocorticotropic Hormone Thyroid Gland • Produces: – T4 - Thyroxine – T3 – Triiodothyronine • Contain Iodine • Regulate energy production & growth – Calcitonin – • Regulates calcium • Maintains strong bones… – Also feeds back through pituitary Parathyroid Glands • “Pair-a-thyroids?” • Produces parathyroid hormone – Also involved in calcium & blood phosphate levels Disorders Associated with Thyroid Gland • Issues directly associated with gland – Tumor • Pituitary malfunction indirectly affecting • Hypothyroidism (Myxedema) • Hyperthyroidism (Grave’s Disease) – Thyrotoxicosis – Thyrotoxic Crisis (Thyroid Storm) Disorders of the Thyroid Gland • Thyroid Storm – Severe Tachycardia, Dysrhythmias – Heart Failure – Shock – Hyperthermia – Restlessness, Agitation & Paranoia – Abdominal pain – Delirium, Coma • What else does this look like? • What could help you distinguish? • Danger in becoming a cynic? Adrenal Glands Each adrenal has: Medulla -Epinephrine Norepinephrin e Cortex -Aldosterone -Cortisol Trouble Associated with Adrenal Gland Cushing’s Syndrome – ACTH Levels too high • Enlarges adrenal gland – May be associated with pituitary tumor Disorders Associated with Adrenal Glands Addison’s Disease – Deficiency of cortisol & aldosterone – Slow, gradual onset – Progressive • Fluid volume deficit • Hyperpigmentation (bronze) Adrenal Gland Disorders Addisonian Crisis – Acute episode preceded by: • Physical or emotional stress – Surgery – Alcohol intoxication – Trauma – Infection – Hypoglycemia – Adrenal cortex cannot comply with body’s increased demand Ovaries Secrete – Estrogen – Progesterone progesterone Testes Secrete – Testosterone – Inhibin Pancreas • U R&L Q • Islets of Langerhans – Produce Glucagon & Insulin Pancreatic Hormones • Glucagon – Alpha Cells – stimulates liver to change glycogen to glucose – raises blood glucose levels • Insulin – Beta Cells – lowers blood glucose levels by increasing transport of glucose into the cells Glucose/Dextrose (D-glucose) • An intermediate in metabolism of carbohydrates • The most important carbohydrate, and is formed during digestion; absorbed from intestines into blood of portal vein; in passage through liver, is converted into glycogen Glucose • May be: – Used immediately – Stored in muscles – Stored in fat • Brain cannot store it’s food – Requires continuous circulating volume – Reason neuro s/s develop quickly Disorders Associated with Pancreatic Dysfunction Diabetes Mellitus – Hyperglycemia – Hypoglycemia – DKA – HHNK Diabetes Mellitus • 16 million in North America. & rising • 3 diagnostic types: – IDDM Type I – NIDDM Type II – Other (Secondary) DM Diabetes Mellitus • IDDM type 1 • Most commonly occurs in children and young adults – Genetic predisposition; Immune mediated destruction of insulin-producing cells Diabetes Mellitus • NIDDM type II – Usually occurs after age 30. – A strong genetic predisposition is evident but pathogenesis is different. – Most individuals obese – Resistance to insulin action is present. – Exogenous insulin not required. Promotion of Hyperglycemia • Increased dietary intake (esp. carbohydrates) • Limitation of physical activity • Reduction of hypoglycemic therapy • Limitation of endogenous insulin production – Pancreatic diseases – Drug treatment – Electrolyte disorders Diabetes Mellitus • Other (secondary) DM – Associates hyperglycemia to another cause including: • Pancreatic disease/Pancreatectomy • Drugs or chemical agents • Others too • Gestational diabetes – Develops during pregnancy and resolves with birth but increased risk of DM later. Development of Insulin Resistance • • • • • • • • Infection Inflammation Myocardial ischemia or infarction Trauma Surgery Emotional stress Pregnancy Drug treatment S/S of Hyperglycemia/Insulin Insufficiency or Resistance • • • • • • Polyuria Polydipsia Nocturia Weight Loss Fatigue Blurred vision Control • Oral • Transplant – Islet cells – Pancreas Oral Hypoglycemic Drugs Generic name Initial dosage Glyburide 1.25-5.0 mg PO qd Duration of activity (hr) 24-60 Glipizide 2.5-5.0 mg PO qd 12-24 Chlorpropamide 100-250 mg PO qd 48-90 Tolazamide 100-250 mg PO qd 10-24 Acetohexamide 250-500 mg PO qd 12-24 Tolbutamide 250-500 mg PO bid 6-12 Metformin 500-1000 mg PO tid Avandia 4 mg PO qd Insulin Insulin Route Onset Peak Duration Novolog Aspart SQ 15 min 1-3 hr 3-5 hr Humalog Lispro SQ 15 min 30-90 min 3-5 hr Regular IV 10-30 min 15-30 min 30-60 min Humulin Regular SQ 30-60 min 2-4 hr 5-7 hr NPH SQ 3-4 hr 6-12 hr 18-24 hr Lantus Glargine SQ 1.1 hr None 24 hr 70/30 NPH/regular SQ 30 min 4-8 hr 24 hr Diabetic Ketoacidosis • A result of severe insulin insufficiency and an excess of glucagon. Type I • Common causes: – Interruption of insulin therapy – Stress, infection – Non-compliance frequently a factor • Onset slow, from 12-24 hours. Diabetic Ketoacidosis • Transition from glucose to lipid metabolism – Forms ketones & increase to toxic levels (diuresed) – Metabolic Acidosis • Symptoms • Causes severe osmotic diuresis and severe dehydration • Tx: Requires close monitoring – Draw red-top – Give IV fluids (Typically 3-5 L Low) – Consider thiamine • All vitamins & Electrolytes grossly deranged Non-Ketotic Hyperglycemic Hyperosmolar Coma (HHNK) • Complication of Type II – Typically preceded by infection &/or diuretics – Hyperglycemic state causes hyperosmolar diuresis – Pronounced volume loss (Towards 10L) • CBG (PG) levels 1000 & higher • Only mild metabolic acidosis – Non-Ketotic – Many electrolytes within normal levels Hypoglycemia • Common causes – Excessive insulin – Stress – Overexertion – Infection – Under eating • Symptoms • Treatment – O2, IV, CBG (Red Top), 50% dextrose IV Endocrine Summary • A VERY complicated system • A specialty of it’s own • Much of EMS treatment is symptom oriented • Much of care is cause oriented – Important distinction