* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download For Examiner Only
Survey
Document related concepts
Transcript
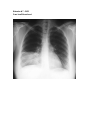
For Examiner Only Case Thyrotoxicosis Author: Tom Morrissey, MD Tom Morrissey Reviewer: Rob Blankenship, MD Approved: 12/6/05 ORAL CASE SUMMARY CONTENT AREA Endocrine Emergencies SYNOPSIS OF CASE 50 yo white female presents with 3 days of nonspecific viral symptoms (productive cough, chills, some diarrhea). She becomes weak tired and confused as the infection unmasks hyperthyroidism and thyrotoxicosis, which progresses to thyroid storm if not recognized and appropriately treated. SYNOPSIS OF HISTORY 10 days the patient began to have diarrhea / loose stools (no blood or mucous) and weight loss and has noted a swelling in her throat. She saw her doctor about this a few days ago to have lab tests run, but they are not back yet. 3 days ago began to have URI symptoms including dry cough, mild sore throat and chills. The cough began to produce sputum “feeling similar to her bouts of bronchitis in the past”. By evening she was feeling very run-down and weak. This morning she was “not acting right” so her husband brought her in to the ED. “She is agitated, short fused, forgetful and not acting like herself” reports her husband. SYNOPSIS OF PHYSICAL Medium-thin white female perturbed about being in the ER but no acute distress. HR 130 irregular RR 16 BP 180/70 Temp 97.5 O2 sat 94% Neuro: Normal except 3+ DTRs and mild tremulousness (both at rest and with intention). Skin: warm to touch, no rash, no diaphoresis Head/neck: Hair grey thin and limp, eyes mild proptosis and lid lag, neck with palpable thyroid with tendernodules , otherwise normal Cor: hyperdynamic, S1S2, irregularly irregular Pulmonary: Mild crackles in right base, no work of breathing. Tachypneic with a rate of 16. Abdomen: Normal Rectal: Rectal watery brown stool, heme negative. Genito-urinary: Normal Extremeties: Paucity of hair, strong otherwise normal CRITICAL ACTIONS 1) 2) 3) 4) Recognize thyrotoxicosis / thyroid storm Start empiric treatment of thyrotoxicosis Look for and treat eliciting events (infection, drugs, iodine ingestion, etc) Recognize and treat pneumonia SCORING GUIDELINES (Critical Action No.) Need to give PTU for thyrotoxicosis but after iodine or risk worsening symptoms FOR EXAMINER ONLY For Examiner Only PLAY OF CASE GUIDELINES (Critical Action No.) 1) Patient presents for mild mental status change with thyrotoxicosis as cause. Physical exam reveals irregular tachycardia, fever, tender thyroid as clues. If not recognized and addressed early, patient continues to decompensate: 1) mental status gets worse and patient develops seizures 2) high output heart failure develops and cardiovascular collapse ensues. 2) Begin empiric treatment of thyrotoxicosis/storm. If condition not recognized and treatment begun empirically, TSH is only lab clue to return (all other TFTs are delayed). Acceptable treatment options are -- beta blocker-preferable propranolol (1mg/min till effect or 10mg total) (guanethedine or reserpine are alternatives, but may not be readily available to candidate) -- PTU (90-1200mg po) or methimazole (90-120mg po). (PTU more rapid and inhibits peripheral conversion of t4 to t3 -- Iodide administration (Na-iodide or K-iodide). Must be given after PTU/methimazole or patient worsens because of release stimulation. 3) Hunt for inciting events --Infectious sources (CXR, UA, skin eval) --Ask about medication changes and compliance, and sources of dietary iodine --DKA --Physical or emotional stresses 4) Recognize and treat pneumonia. Pt will complain of cough and chest pain. CXR will reveal RLL PNA. Evaluation for PE will be negative or indeterminate (she doesn’t have one). --If PNA not recognized and treated, patient will continue with pulmonary deterioration, hypoxia and need for intubation. If still not recognized she will progress to septic shock and cardiovascular collapse. --Treatment for community acquired PNA is acceptable (cephalosporin+macrolide or flouroquinolone is acceptable). FOR EXAMINER ONLY For Examiner Only Critical Actions 1. Recognize thyrotoxicosis/thyroid storm This critical action is met by the candidate Cueing Guideline: tender enlarged thyroid, low TSH. Patient will not improve until appropriate treatment started. Will progress to worsening storm, seizures, high output heart failure, cardiovascular collapse. 2. Empirically treat thyrotoxicosis/thyroid storm This critical action is met by the candidate Cueing Guideline: TSH is the only thyroid function test to return until appropriate treatment is begun. 3. Search for eliciting cause of decompensation (infection, drugs, iodine ingestion, etc) This critical action is met by the candidate Cueing Guideline: Nurse asks if you want other tests. Consultant asks why she is in thyroid storm. 4. Recognize and treat pneumonia This critical action is met by the candidate Cueing Guideline: Nurse asks if you want any other medications. Respiratory status worsens, pt becomes hypoxic and needs intubation of pneumonia not recognized and treatment begun. For Examiner Only History Data Panel 50 year old white female Onset of Symptoms: 3 days, worsening since yesterday. Description of Complaint: 10 days the patient began to have diarrhea / loose stools (no blood or mucous) and weight loss and has noted a swelling in her throat. She saw her doctor about this a few days ago to have lab tests run, but they are not back yet. 3 days ago began to have URI symptoms including dry cough, mild sore throat and chills. The cough began to produce sputum “feeling similar to her bouts of bronchitis in the past”. By evening she was feeling very run-down and weak. This morning she was “not acting right” so her husband brought her in to the ED. “She is agitated, short fused, forgetful and not acting like herself” reports her husband. Past Medical History Surgical: vaginal hysterectomy Medical: mild childhood asthma Injuries: none Allergies: none Habits Smoking: cigatettes ( 1 ppd x 25 years) Drugs: none Alcohol: none Family Medical History Father: none Mother: thyroid surgery Siblings: sister died of breast cancer in her 40s Social History Married: 30 years Children: 2 healthy (29 and 27yo) Employed: ER nurse Education: RN For Examiner Only Physical Data Panel Patient: Ima Bitconfused 50 year old female General Appearance: irritated and nervous, but no respiratory distress Vital Signs: BP : 180/70 P : 130 irregular R : 16 T : 102.9 Head: thin limp grey hair Eyes: mild proptosis, mild lid-lag Ears: normal Mouth: normal Neck: no JVD, no bruits, palpable thyroid with small tender nodules Skin: warm to touch, no rash, no diaphoresis Chest: few crackles heard in right base, otherwise normal Heart: hyperdynamic PMI, S1S2 audible, tachycardic, irregularly irregular, Abdomen: normal Extremities: paucity of hair, otherwise normal Rectal: watery brown stool, no blood or mucus, heme-occult negative Pelvic: normal Neurological: Alert and oriented times 3, but agitated. Mild tremor both at rest and with intended movement. Normal gait. CN 2-12 intact and symmetric. Normal symmetric motor exam without pronator drift. Normal sensory exam without extinction. DRTs symmetric and 3+. No dysmetias or past-pointing. Mental Status: Agitated with short attention span. For Examiner Only Lab Data Panel Stimulus #2 - CBC Complete Blood Count WBC 13,000 /mm3 Hgb 11 g/dL Hct 35 % Platelets 350,000 /mm3 Differential Segs 79 % Bands 3 % Lymphs 16 % Monos 1 % Eos 1 % Stimulus #3 - Chem-7 Na+ 144 K+ 4.5 CO2 35 Cl98 mEq/L mEq/L mEq/L mEq/L Glucose 100 BUN 15 Creatinine 1.0 mg/dL mg/dL mg/dL Stimulus #4 - Urinalysis Color Sp gravity Glucose Protein Ketone Leuk. Est. Nitrite WBC RBC Yellow 1.020 neg neg neg neg neg 0-5 0-5 Stimulus #5 - Arterial Blood Gases pH 7.32 pCO2 pO2 O2 Sat 28 90 95% mm Hg mm Hg % Stimulus #6 - TSH undetectable Stimulus #7 – CXR RLL infiltrate (see below) Stimulus #8 – EKG a-fib. No ischemic chg. (see below) Stimulus #9 -- Full Thyroid Function Tests (sendout) VERBAL REPORTS For Examiner Only Stimulus Inventory #1 Emergency Admitting Form #2 CBC #3 Chem-7 #4 Urinalysis #5 Arterial Blood Gases #6 TSH #7 CXR #8 EKG #9 Thyroid Function Tests #10 FOR EXAMINER ONLY Stimulus #1 ABEM General Hospital Emergency Admitting Form Name : Ima Bitconfused Age : 50 Sex : Female Method of Transportation : Husband in car Person giving information : Patient and Husband Presenting complaint : Not eating right, recent bronchitis and diarrhea Background: Pt with Hx of bronchitis. Having typical attack after cold symptoms. Today became more confused and agitated Vital Signs: BP : 180/70 P : 130 irregular R : 16 T : 100.5.F Stimulus # 2 - CBC Case Ima Bitconfused Complete Blood Count WBC 13,000 /mm3 Hgb 11 g/dL Hct 35 % Platelets 350,000 /mm3 Differential Segs 79 Bands 3 Lymphs 16 Monos 1 Eos 1 % % % % % Stimulus # 3 – Chem - 7 Case Ima Bitconfused Na+ K+ CO2 Cl- 144 4.5 35 98 Glucose 100 BUN 15 Creatinine 1.0 mEq/L mEq/L mEq/L mEq/L mg/dL mg/dL mg/dL Stimulus # 4 - Urinalysis Case Ima Bitconfused Color Sp gravity Glucose Protein Ketone Leuk. Est. Nitrite WBC RBC Yellow 1.020 neg neg neg neg neg 0-5 0-5 Stimulus # 5 – Arterial Blood Gases Case Ima Bitconfused pH 7.32 pCO2 pO2 O2 Sat 28 mm Hg 90 mm Hg 95% % Stimulus # 6 - TSH Case Ima Bitconfused TSH undetectable Stimulus # 7 - CXR Case Ima Bitconfused Stimulus # 8 - EKG Case Ima Bitconfused Stimulus # 9 – Thyroid Function Tests Case Ima Bitconfused Labs were sent out Mock Oral Feedback Form Date: Examiner: Examinee: Data acquisition Worst 1 NOTES 2 3 4 5 6 7 8 Best Problem solving Worst 1 NOTES 2 3 4 5 6 7 8 Best Patient management Worst 1 2 NOTES 3 4 5 6 7 8 Best Resource utilization Worst 1 2 NOTES 3 4 5 6 7 8 Best Health care provided Worst 1 2 NOTES 3 4 5 6 7 8 Best 4 5 6 7 8 Best Comprehension of path physiology Worst 1 2 3 4 NOTES 5 6 7 8 Best Clinical competence (overall) Worst 1 2 3 NOTES 5 6 7 8 Best Patient Interpersonal relations Worst 1 2 3 NOTES 4 Critical Actions Dangerous actions Recognize thyrotoxicosis / thyroid storm and omissions Start empiric treatment of thyrotoxicosis Look for and treat eliciting events (infection, drugs, iodine ingestion, etc) Recognize and treat pneumonia