* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Effect of exercise intensity on depressive symptoms in women
Child psychopathology wikipedia , lookup
Nazareth-Conferences wikipedia , lookup
Bipolar II disorder wikipedia , lookup
Postpartum depression wikipedia , lookup
Behavioral theories of depression wikipedia , lookup
Major depressive disorder wikipedia , lookup
Biology of depression wikipedia , lookup
Evolutionary approaches to depression wikipedia , lookup
Depression in childhood and adolescence wikipedia , lookup
Neurobiological effects of physical exercise wikipedia , lookup
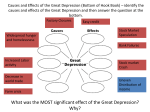
Mental Health and Physical Activity 2 (2009) 37–43 Contents lists available at ScienceDirect Mental Health and Physical Activity journal homepage: www.elsevier.com/locate/menpa Effect of exercise intensity on depressive symptoms in women I-Hua Chu a,1, Janet Buckworth b, *, Timothy E. Kirby c, 2, Charles F. Emery d, 3 a Department of Family and Preventive Medicine, University of California, San Diego, 9500 Gilman Drive, La Jolla, CA 92093, USA Health and Exercise Science, The Ohio State University, A44 PAES Building, 305 W. 17th Avenue, Columbus, OH 43210, USA c Health and Exercise Science, The Ohio State University, A54 PAES Building, 305 W. 17th Avenue, Columbus, OH 43210, USA d Department of Psychology, The Ohio State University, 145 Psychology Building, 1835 Neil Avenue, Columbus, OH 43210, USA b a r t i c l e i n f o a b s t r a c t Article history: Received 19 August 2008 Received in revised form 7 January 2009 Accepted 7 January 2009 Exercise has been shown to relieve depressive symptoms, yet optimal exercise intensity for treating depression has not been established. The mechanisms that explain the antidepressant effect of exercise also require investigation. The purpose of this study was to test (a) the effect of two different exercise intensities prescribed for aerobic training on depressive symptoms, and (b) a previously proposed psychological mechanism for this effect: self-efficacy. Sedentary women scoring 14 on the Beck Depression Inventory-II (BDI-II) were randomized to one of two aerobic training groups that differed on exercise intensity (high [65–75% MaxVO2 reserve] or low [40–55% MaxVO2 reserve]), or to a stretching control group for 10 weeks. Main outcome variables included depressive symptoms (BDI-II) and selfefficacy (exercise self-efficacy [ESE] and depression coping self-efficacy [DCSE]), which were measured at study entry, 5 and 10 weeks later. Participants in all groups (high, n ¼ 18; low, n ¼ 18; stretching, n ¼ 18) had significant reductions in depressive symptoms at Week 5 (p < .001) and Week 10 (p < .001). The BDIII change scores did not differ significantly among the groups (p ¼ .066). Follow-up analyses controlling for baseline BDI-II scores showed that the high intensity group had significantly fewer depressive symptoms than the low intensity and stretching control groups at weeks 5 and 10 (p < .05). There was no significant association between changes in aerobic capacity and changes in depressive symptoms (r ¼ .099, p ¼ .491). At 10 weeks, both ESE (p ¼ .013) and DCSE (p < .001) increased significantly for the whole sample, with no significant group difference (p ¼ .613 for ESE, p ¼ .277 for DCSE). Controlling for baseline scores, the increase remained significant for ESE (p ¼ .005) but not for DCSE (p ¼ .629). Partial correlations showed significant negative relationships between both types of self-efficacy and depressive symptoms at Week 5 and Week 10 (p < .02). We concluded that both high and low intensity aerobic exercise, as well as stretching exercise were associated with reductions in mild to moderate depressive symptoms in initially sedentary women. Changes in depression were associated with changes in ESE and DCSE. Published by Elsevier Ltd. Keywords: Women Depressive symptoms Exercise training Self-efficacy 1. Introduction Depression is a serious mental disorder throughout the world, and the fourth leading cause of disease burden, accounting for 4.4% of total disability adjusted life years (Global Burden of Disease: Ustun, Ayuso-Mateos, Chatterji, Mathers, & Murray, 2004). In the U.S., the estimated lifetime prevalence of major depressive disorder (MDD) is 16.2% (Kessler et al., 2003). In any given year, * Corresponding author. Tel.: þ1 614 292 0757; fax: þ1 614 688 3432. E-mail addresses: [email protected] (I.-H. Chu), [email protected] (J. Buckworth), [email protected] (T.E. Kirby), [email protected] (C.F. Emery). 1 Tel.: þ1 858 457 7296. 2 Tel.: þ1 614 292 0664. 3 Tel.: þ1 614 688 3061. 1755-2966/$ – see front matter Published by Elsevier Ltd. doi:10.1016/j.mhpa.2009.01.001 approximately 13.7 million U.S. adults suffer from a depressive disorder (Kessler et al., 2003). Women are twice as likely as men to suffer from depression. A national survey indicated that the lifetime prevalence for MDD is 12.6% among women and 6.3% among men (Riolo, Nguyen, Greden, & King, 2005). Despite the availability of effective pharmacological and psychotherapeutic treatments for depression, only 51.6% of adults suffering from MDD seek treatment, and only 21.7% are adequately treated (Kessler et al., 2003). Unlike traditional treatments, which can carry social stigma, exercise is socially acceptable, has fewer side effects, and has additional health benefits. Hence, exercise may be a more satisfactory treatment for some individuals with depression. Involvement in structured exercise has been shown to improve symptoms of depression (Craft & Perna, 2004; Paluska & Schwenk, 2000; Teychenne, Ball, & Salmon, 2008). Experimental and 38 I.-H. Chu et al. / Mental Health and Physical Activity 2 (2009) 37–43 meta-analytic studies also indicate that exercise training is as effective as antidepressant medication and psychotherapy (Blumenthal et al., 1999; Craft & Landers, 1998; North, McCullagh, & Tran, 1990). Recently, Dunn, Trivedi, Kampert, Clark, and Chambliss (2005) reported that aerobic exercise at a dose consistent with public health recommendations (17.5 kcal/kg/week) is an effective treatment for MDD of mild to moderate severity. Also, when controlling total energy expenditure, exercise frequency (3 or 5 days/week) did not moderate the effect of exercise on depression. While this study quantified the amount of exercise needed to reduce symptoms of MDD, the effect of exercise intensity during aerobic training was not examined. It is unknown whether exercise intensity played a role in the antidepressant effect of exercise. Exercise intensity is one of the essential components (i.e., intensity, duration, frequency, type) in exercise prescriptions. Previous studies have indicated that reductions in depression were not associated with differences in exercise duration, frequency, and type (Craft & Landers, 1998; Dunn et al., 2005; North et al., 1990). However, results from studies regarding exercise intensity and depression have been equivocal. While some studies suggested that both vigorous and moderate intensity exercise are equally effective in alleviating symptoms of depression (Craft & Landers, 1998; Craft & Perna, 2004), others reported an inverse relationship between exercise intensity and depressive symptoms (Lampinen, Heikkinen, & Ruoppila, 2000; Teychenne et al., 2008). In a review of studies on the association between physical activity and depression in young adult women, Azar, Ball, Salmon, and Cleland (2008) found that even low levels of physical activity had a positive effect on symptoms of depression. However, dose–response effects and the influence of exercise intensity were inconclusive because of limited research and weaknesses in methodology. To examine the effect of exercise intensity on depression, total energy expenditure must be controlled in consideration of evidence that total energy expenditure is an important variable in exercise programs for depression (e.g., Dunn et al., 2005) and to extend the majority of previous studies that did not monitor or control for total energy expenditure. Therefore, the purpose of this study was to examine the effect of two different exercise intensities (high vs. low) during aerobic training on depressive symptoms in initially sedentary depressed women while controlling for total energy expenditure. The mechanisms by which exercise exerts its antidepressant effect have not been studied extensively and are not well understood (Craft, 2005). A better understanding of the mechanisms would be helpful for future use of exercise as an adjunct or alternative treatment of depression and more studies are needed to examine the potential physiological and psychological mechanisms (Craft, 2005; Dunn, Trivedi, & O’Neil, 2001; Fox, 1999; Landers & Arent, 2001). One plausible psychological mechanism that is based on existing theories of depression and warrants further examination is self-efficacy (Craft, 2005). Self-efficacy is the degree to which an individual believes he or she can successfully engage in a specific behavior in a particular situation with known outcomes (Bandura, 1986). In the current study two types of self-efficacy were measured, including exercise self-efficacy and depression coping self-efficacy. Exercise self-efficacy measures one’s confidence to overcome barriers to exercise. Depression coping self-efficacy measures one’s confidence to engage in different activities to cope with depressive symptoms. Research shows that depressed individuals have low self-efficacy to cope with their depressive symptoms (deVries, Wiswell, Bulbulian, & Moritani, 1981) and mastery experience of a difficult skill can help increase a person’s self-confidence, self-efficacy, and ability to cope with personal problems (Bandura, 1997). Thus, it was hypothesized that for depressed individuals, engaging in regular exercise, which is usually perceived as a difficult task, is likely to result in increased self-efficacy and enhanced ability to cope with the symptoms of depression. While self-efficacy has been found to influence exercise adoption and adherence in various populations (e.g., Dishman et al., 2005; McAuley, Jerome, Elavsky, Marquez, & Ramsey, 2003; van Weert et al., 2008; Wilbur, Vassalo, Chandler, McDevitt, & Miller, 2005), the relationship between exercise and self-efficacy in depressed population has not been studied extensively and findings have been equivocal (Bodin & Martinsen, 2004; Craft, 2005; Singh et al., 2005). In addition, no studies were found that examined the role of self-efficacy in respect to training intensity in a depressed population. In contrast to a moderate exercise program, successfully completing a vigorous exercise program may lead to greater mastery experiences, more enhanced self-efficacy, and thus greater reductions in depression. Therefore, a secondary objective of this study was to examine the relationships between exercise intensity, self-efficacy, and depressive symptoms. 2. Methods 2.1. Participants Women aged 18–43 years with mild to moderate depressive symptoms (a score of 14–28 on Beck Depression Inventory-II [BDI-II]) were recruited from a university community via physician referrals, posted flyers, classroom presentations, and word of mouth. If a volunteer’s score indicated she had severe depressive symptoms (a score above 28 on BDI-II), she could participate in this study only with written permission from a physician or other health care professional. To enroll in the study, participants also had to be sedentary, which was defined as exercising less than three times per week for less than 20 min per session, assessed using responses to the Godin Leisure-Time Exercise Questionnaire (Godin & Shephard, 1985). Other inclusion criteria were: having a regular menstrual cycle during the previous six months; not taking medication for depression or having taken current medication for at least three weeks (i.e., stabilized on current dose of medication); and not receiving any other treatment for depression (e.g., psychotherapy). Exclusion criteria were: suicidal ideation reported on the BDI-II; a body mass index (BMI) less than 18.5 (underweight) or over 35 (obese); current pregnancy or nursing or planned pregnancy during the following six months; and inability to exercise due to physical contraindications (e.g., orthopedic problems, heart disease). All participants completed informed consent in compliance with the Institutional Review Board of the university. 2.2. Study design The study had one between-subject factor (group assignment: 3 levels) and one within-subject factor (time: 3 levels). Participants were randomly assigned to one of two aerobic exercise groups (i.e., high intensity exercise or low intensity exercise), or to a stretching exercise contact control group. The randomization was accomplished by drawing participants’ group assignments from a bag. At study entry, participants performed maximal exercise testing using the Balke treadmill protocol (Pollock, 2001) to determine maximal oxygen uptake. After completing all the baseline assessments, participants were informed of their group assignment. All participants began their training program within two weeks of their baseline evaluation. A 10-week training program was selected based upon results from a meta-analysis by Craft and Landers (1998) that found exercise interventions lasting at least 9 weeks were most effective in alleviating symptoms of depression. Over the course of 10 weeks, each I.-H. Chu et al. / Mental Health and Physical Activity 2 (2009) 37–43 group met with the investigator once per week for supervised exercise sessions. Participants in the aerobic groups exercised on a treadmill for 30–40 min per supervised session, and those in the stretching control group performed 30 min of supervised stretching and flexibility exercise. Both aerobic groups began at an intensity of 40–55% of oxygen uptake reserve (VO2R) (Franklin, Whaley, Howley, Balady, & Grais, 2000). After three weeks of training, the intensity was increased to 65–75% of VO2R for the high intensity group (Franklin et al., 2000). To make exercise more convenient and reduce the burden and possible barrier of multiple weekly trips to the school training facility, the aerobic groups’ participants were asked to complete three to four exercise sessions each week on their own. During these unsupervised sessions, participants chose their preferred types of aerobic exercise, such as aerobic dancing, walking, or biking. Exercise intensity and duration were prescribed by the investigator based on the individual’s group assignment to meet an exercise energy expenditure goal of 1000 Kcal/wk. The Compendium of Physical Activities (Ainsworth et al., 2000) was referenced to assign the intensity for each type of exercise. Participants in the stretching control group were instructed to maintain their physical activity level. All participants were also given an activity diary to complete, and diaries were reviewed weekly during supervised sessions to monitor participants’ exercise intensity and weekly energy expenditure. Weekly energy expenditure was calculated from the recorded exercise intensity, duration, and frequency using formulae provided in the ACSM’s guidelines for exercise testing and prescription (Franklin et al., 2000). 2.3. Outcome measures 2.3.1. Depressive symptoms Depressive symptoms were measured at study entry, Week 5 and Week 10 using the Beck Depression Inventory-II (BDI-II) (Beck, Steer, & Brown, 1996). The BDI-II is a self-report inventory with 21 items assessing the behavioral and cognitive symptoms of depression. Each item consists of four statements numbered from ‘‘0’’ to ‘‘3,’’ with higher numbers indicating more severe depressive symptoms. Participants were asked to circle the statement that best described them during the prior week. The circled numbers were summed to obtain a total score (range ¼ 0–63). Scores of 0–13 indicate minimal depression,14–19 indicate mild depression, 20–28 indicate moderate depression, and 29–63 indicate severe depression. This inventory has demonstrated acceptable internal consistency with Cronbach’s alphas ranging from .92 to .93 (Beck et al., 1996). Psychometric analyses for both normal and psychiatric populations also have consistently indicated that the BDI-II is a reliable and valid measure of self-reported depression (Steer, Ball, Ranieri, & Beck, 1997). 2.3.2. Exercise self-efficacy The Exercise Self-efficacy Questionnaire (Garcia & King, 1991) was used to measure exercise self-efficacy (ESE) at study entry, Week 5 and Week 10. Participants rated their confidence from 0% (I cannot do it at all) to 100% (certain that I can do it) in their ability to exercise under 15 different conditions (e.g., when tired; during bad weather) over the next three months. The ratings for all items were summed and then divided by 15 to obtain a mean score. This scale has demonstrated acceptable internal consistency with Cronbach’s alpha ranging from .90 to .94 (Wilcox, Sharpe, Hutto, & Granner, 2005). Psychometric analyses in a diverse sample of men and women indicated that the ESE questionnaire is a valid and reliable measure for use with diverse populations (Wilcox et al., 2005). 2.3.3. Depression coping self-efficacy Depression coping self-efficacy (DCSE) was measured at study entry, Week 5 and Week 10 by the Depression Coping Self-Efficacy 39 Scale, a 24-item scale assessing coping self-efficacy of depressed patients (Perraud, 2000). Each item describes a coping response (e.g., get together with at least one very close person when I am feeling lonely; take a bath or do some other soothing activity before bedtime) and participants were asked to rate their confidence from 0% (not at all confident) to 100% (confident) in their ability to engage in the coping response. Ratings for all items were summed and divided by 24 to obtain a mean score. This scale has a test–retest reliability of .84 and has demonstrated acceptable internal consistency reliability with a Cronbach’s alpha of .93 (Perraud, 2000). The BDI-II was chosen as a test of concurrent validity for DCSE, and the validity analysis showed a significant negative correlation between DCSE and the BDI-II (r ¼ .73, p < .001) (Perraud, 2000). 2.4. Statistical analysis Sample size calculation was based on the average effect sizes reported in previous meta-analyses which indicated that exercise groups decreased depression scores at least 0.50 standard deviation more than comparison groups (e.g., control, leisure activity, or psychotherapy groups) (Craft & Landers, 1998; North et al., 1990). We estimated that we required 14 participants in each group (total sample size ¼ 42) at an alpha level of .05, a power of .80, and an effect size of 0.5. Sample sizes were inflated by 30% to allow for possible attrition. Descriptive statistics were performed for baseline characteristics of the participants. Intent-to-treat analysis of all randomized participants was conducted. Missing data were imputed by carrying forward the last recorded observation. Three separate repeated measures analyses of variance (ANOVAs) were performed to examine between group differences over time on depressive symptoms, exercise self-efficacy, and depression coping self-efficacy. Analysis of covariance (ANCOVA) and post hoc comparisons controlling for baseline scores were conducted to evaluate simple effects (i.e., whether HI, LO, or SC had higher mean scores) at Weeks 5 and 10. Within subjects repeated measures ANOVA was performed to determine at what time points the change of mean scores occurred (i.e., if change occurred from study entry to Week 5 or from Week 5 to Week 10). Preliminary analyses showed that BMI and antidepressant use did not differ across conditions, p ¼ .50, and did not predict BDI-II scores over 10 weeks, therefore, these variables were omitted from the model. Partial correlations were calculated to examine (a) the relationship between ESE and BDI-II and (b) the relationship between DCSE and BDI-II at Week 5 and Week 10 controlling for baseline values of ESE and DCSE at each time point. The significance level (a level) was set at .05 and partial Eta squared (h2) was used as an indicator of effect size. All data analyses were performed with the Statistical Package for the Social Sciences (SPSS), Version 14.0 (SPSS, Inc., Chicago, IL, 2004). 3. Results A total of 126 women were assessed for eligibility through telephone or e-mail prescreen (Fig. 1). The 93 eligible women were then scheduled for a screening visit to assess depressive symptoms, level of physical activity, BMI, and other inclusion and exclusion criteria. Fifty-four women met the study criteria and were enrolled in the study. The major reasons for ineligibility were having minimal depressive symptoms, currently receiving psychotherapy, and inability to make the time commitment. The 54 participants were randomized to one of the two treatment conditions: high intensity aerobic exercise (HI; n ¼ 18) vs. low intensity aerobic exercise (LO; n ¼ 18), or to the stretching exercise control (SC; n ¼ 18) group. 40 I.-H. Chu et al. / Mental Health and Physical Activity 2 (2009) 37–43 Assessed for eligibility N = 126 Phone/email screen - ineligible n = 33 Not meeting inclusion criteria (n = 16) Refused to participate (n = 7) Other (n = 10) Enrollment Phone/email screen - eligible n = 93 Screening visit - ineligible n = 39 Not meeting inclusion criteria (n = 25) Refused to participate (n = 6) Other (n = 8) Analysis Follow-up Allocation Screening visit - eligible n = 54 Randomized n = 54 HI n = 18 LO n = 18 SC n = 18 HI Lost to follow-up (n = 0) Never started (n = 0) Discontinued intervention (n = 3) Worsened (n = 0) Medical (n = 1) Other (n= 2) LO Lost to follow-up (n = 0) Never started (n = 0) Discontinued intervention (n = 7) Worsened (n = 1) Medical (n = 1) Other (n = 5) SC Lost to follow-up (n = 2) Never started (n = 2) Discontinued intervention (n = 2) Worsened (n = 0) Medical (n = 0) Other (n = 2) HI Intent to treat (n = 18) Excluded from analysis (n = 0) LO Intent to treat (n = 18) Excluded from analysis (n = 0) SC Intent to treat (n = 18) Excluded from analysis (n = 0) Fig. 1. Participant flow from enrollment to analysis. Baseline characteristics of the 54 participants are shown in Table 1. There were no significant group differences in baseline characteristics. Twenty-one participants (39%) had been taking medication (i.e., Effexor, Lexapro, Paxil, Wellbutrin, and Zoloft) for their depressive symptoms at study entry for more than three weeks (see Table 1). The percentage of antidepressant use was not significantly different among the groups (p ¼ .496). At study entry, the average BDI-II scores were above 20 (total sample BDI-II baseline range 15–37), suggesting that on average the participants in each group were experiencing moderate depressive symptoms (BDI-II scores 20–28). Of the 54 participants, 16 (30%) did not finish the 10-weeks training program [three from HI (17%), seven from LO (39%), and six from SC (33%)]. Drop-out rate was not significantly different among the groups (p ¼ .315). The major reasons for drop-out were lack of time for exercise and low compliance with assigned exercise intensity and energy expenditure. Participants who dropped out of the study were not significantly different from those who completed the intervention in all baseline characteristics except for antidepressant use. Significantly more participants in the drop-out group were taking antidepressants at study entry (p ¼ .021). ranged from 80% to 100%, with no significant group difference (HI ¼ 97.3%; LO ¼ 99.1%; SC ¼ 99.2%, p ¼ .475). The average intensity of training, including supervised and unsupervised sessions, was 72 12.9% of VO2R in HI, 45 7.1% of VO2R in LO, and 25 6.0% of VO2R in SC, indicating successful maintenance of the intended training intensity in the three groups. The average energy expenditure (EE) from exercise was significantly higher for HI (1007.3 kcal/ week) and LO (905.2 kcal/week) as compared to SC (215.8 kcal/week) (p < .001). The average EE did not differ significantly between HI and LO (p ¼ .166). The average exercise frequency (EF) was significantly higher for HI (3.7 sessions/week) and LO (4.9 sessions/week) as compared to SC (2.1 sessions/week) (p < .001). LO also had significantly higher EF than HI (p ¼ .002). During unsupervised sessions, the majority of participants in both HI and LO engaged in walking, jogging, bicycling, or exercising on an elliptical trainer. After 10 weeks of exercise training, participants in HI exhibited a significant 7% increase in maximal VO2 (from 32.3 to 34.6 ml/kg/min, F ¼ 11.692, p ¼ .004, h2 ¼ .455). There was no change in maximal VO2 for LO or SC. 3.1. Exercise training As shown in Table 2, the intent-to-treat analysis for the whole sample (N ¼ 54) revealed a significant improvement over time in BDI-II scores across all groups (F ¼ 75.48, p < .001, h2 ¼ .597), with no significant group by time interaction (F ¼ 2.58, p ¼ .066, h2 ¼ .092). The main effect for group was significant (F ¼ 4.13, p ¼ .022, h2 ¼ .139). These findings suggest that, regardless of group, all participants had decreased depressive symptoms. Overall the The average attendance rate for the supervised sessions ranged from 0% to 100% for the whole sample (N ¼ 54), with no significant difference among the groups (HI ¼ 87.2%; LO ¼ 77.2%; SC ¼ 76.1%, p ¼ .504). For the 38 participants who completed the 10-week training program, average attendance rate for supervised sessions 3.2. Depressive symptoms I.-H. Chu et al. / Mental Health and Physical Activity 2 (2009) 37–43 41 Table 1 Baseline characteristics. Characteristic HI (n ¼ 18) Age, y (range 18–43) BMI, kg/m2 VO2max, ml/kg/min BDI-II ESE, % DCSE, % Antidepressants, n LO (n ¼ 18) SC (n ¼ 18) Group difference M SD M SD M SD p 26.4 25.0 33.1 21.6 68.2 69.4 6 7.3 4.1 5.6 6.1 15.3 9.0 26.6 23.5 34.1 22.4 58.2 70.7 9 6.3 3.7 5.5 4.9 20.7 11.9 24.6 23.8 33.6 23.4 60.2 66.8 6 4.8 4.0 6.4 4.7 19.5 13.5 .56 .50 .86 .60 .24 .59 .50 Note. BMI ¼ Body Mass Index; BDI-II ¼ Beck Depression Inventory-II; ESE ¼ Exercise Self-efficacy; DCSE ¼ Depression Coping Self-efficacy. average BDI-II score decreased significantly from 22.5 (moderate depressive symptoms) to 13.9 (mild depressive symptoms) at 5 weeks and continued to decrease significantly to 11.3 (minimal depressive symptoms) at 10 weeks. Because group means appeared different and low statistical power (0.58) was suspected for the non-significant group by time interaction, further analyses were conducted. Follow-up ANCOVA and post hoc comparisons controlling for baseline BDI-II scores showed that HI had significantly fewer depressive symptoms than LO and SC at both Week 5 (HI 9.7 vs. LO 15.9, p ¼ .022; HI 9.7 vs. SC 15.9, p ¼ .037) and Week 10 (HI 6.4 vs. LO 12.7, p ¼ .034; HI 6.4 vs. SC 14.6, p ¼ .009). BDI-II scores were not significantly different between LO and SC at either Week 5 (p ¼ .841) or Week 10 (p ¼ .583). There was no significant association between changes in aerobic capacity and changes in depressive symptoms (r ¼ .099, p ¼ .491). We analyzed the BDI-II data using the criteria for a clinically significant reduction in depression according to Seggar, Lambert, and Hansen (2002). Results showed that 13 participants (72%) in HI, 9 (50%) in LO, and 6 (33%) in SC met the criteria for a clinically significant reduction in depression. These group differences did not reach statistical significance (p ¼ .064). Participants who were taking antidepressants at study entry did not change the type and amount of their medication during the course of this study, and the improvements in BDI-II over time were similar between those who took antidepressants and those who did not (p > .15). Thus, the effects of the medication should not have affected the study results. using ANCOVA to control for baseline ESE scores, with a significant improvement from Week 5 to 10 (F ¼ 8.750, p ¼ .005, h2 ¼ .149) and no significant group by time interaction (F ¼ 1.825, p ¼ .668, h2 ¼ .068) or group effect (F ¼ 0.407, p ¼ .668, h2 ¼ .016). These findings suggest that, regardless of group, all participants experienced increased exercise self-efficacy across time. Overall the average ESE score increased significantly from 62.2% to 68.1% after the 10-week training program. 3.3.2. Depression coping self-efficacy The intent-to-treat analysis showed that there was a significant improvement in DCSE over time (F ¼ 14.296, p < .001, h2 ¼ .219). Overall, the average DCSE score increased significantly from 69.0% to 75.7% after the 10-weeks training program. There was no significant group by time interaction (F ¼ 1.304, p ¼ .277, h2 ¼ .049) (Table 2) or main effect for group (F ¼ .880, p ¼ .421, h2 ¼ .033). When using ANCOVA to control for baseline DCSE scores, there was also no significant improvement from Week 5 to 10 (F ¼ 0.236, p ¼ .629, h2 ¼ .005) and no significant group by time interaction (F ¼ 0.502, p ¼ .020, h2 ¼ .068) or group effect (F ¼ 1.818, p ¼ .173, h2 ¼ .068). 3.4. Correlation analysis After controlling for baseline values, partial correlations revealed significant negative correlations between exercise selfefficacy and depressive symptoms at Week 5 (r ¼ .348, p ¼ .011) and Week 10 (r ¼ .492, p < .001). Partial correlations also revealed significant negative correlations between depression coping selfefficacy and depressive symptoms at Week 5 (r ¼ .487, p < .001) and Week 10 (r ¼ .652, p < .001). 3.3. Self-efficacy 3.3.1. Exercise self-efficacy The intent-to-treat analysis showed that there was a significant improvement in ESE over time (F ¼ 5.062, p ¼ .013, h2 ¼ .090) but no significant group by time interaction (F ¼ .622, p ¼ .613, h2 ¼ .024) (Table 2). The main effect for group was also not significant (F ¼ 1.383, p ¼ .260, h2 ¼ .051). Similar results were found 4. Discussion A number of exercise intervention studies have demonstrated a reduction in depressive symptoms following exercise programs of various modes and durations (Blumenthal et al., 1999; Craft, 2005; Table 2 Mean psychological values by group at study entry, Week 5, and Week 10. Measure BDI-II pre BDI-II w5 BDI-II w10 ESE pre ESE w5 ESE w10 DCSE pre DCSE w5 DCSE w10 HI (n ¼ 18) LO (n ¼ 18) SC (n ¼ 18) Time M SD M SD M SD 21.6 9.7 6.4 68.2 67.2 74.4 69.4 74.7 79.7 6.1 4.4 4.0 15.3 17.3 15.2 9.0 10.6 10.4 22.4 15.9 12.7 58.2 62.7 66.3 70.7 70.9 74.7 4.9 9.8 10.4 20.7 20.1 21.5 11.9 14.1 16.5 23.4 15.9 14.6 60.2 61.3 63.5 66.8 70.2 72.7 4.7 8.0 9.2 19.5 18.3 16.7 13.5 9.9 9.5 Group time F p F p 75.47 <.001 2.58 .07 .62 .61 1.30 .28 5.06 .01 14.29 <.001 Note. BDI-II ¼ Beck Depression Inventory-II; ESE ¼ Exercise Self-efficacy; DCSE ¼ Depression Coping Self-efficacy. F ratio and p values from repeated measures analysis of variance model. 42 I.-H. Chu et al. / Mental Health and Physical Activity 2 (2009) 37–43 Dimeo, Bauer, Varahram, Proest, & Halter, 2001; Dunn et al., 2005). In our study, we found that both high and low intensity aerobic exercise groups and stretching control group had significant improvements in depressive symptoms at both 5 weeks and 10 weeks. All participants began the study with moderate depressive symptoms, and after 10-weeks of aerobic exercise training or stretching, their BDI-II scores indicated only minimal depressive symptoms. There was no significant difference in the reduction in BDI-II scores among the groups. These results suggest that both high and low intensity aerobic exercise, as well as stretching exercise were associated with reductions in mild to moderate depressive symptoms. However, when comparing BDI-II scores between groups at each time point, participants in HI reported significantly fewer depressive symptoms than those in LO and SC at both weeks 5 and 10 (p < .05). The LO and SC, on the other hand, did not differ significantly at either time point. These results suggest that a high intensity (65–75% of VO2R) aerobic exercise program may be more effective in reducing symptoms of depression. Yet, since the overall reductions in depression did not differ significantly among the groups, whether high intensity exercise is necessary for improving symptoms of depression requires further investigation. We found that changes in aerobic capacity were not significantly associated with changes in depressive symptoms. This finding mirrors results of previous studies suggesting that fitness gain is not required for reductions in depression (Craft & Landers, 1998; North et al., 1990; Veale et al., 1992). The reductions in depression found in this study may have been a result of placebo effects since the SC group also showed significant improvements. In other words, participant’s expectation, social contact, and personal attention given by the investigator may have partially contributed to the improved depressive symptoms for all participants after exercise training. Furthermore, stretching exercise, although used as a placebo control, may actually be an effective activity treatment for depressive symptoms. In our study, we introduced a yoga-based stretching exercise. Recently, research conducted on yoga and depression has suggested that yoga practice can be an effective treatment for depressive symptoms (Elavsky & McAuley, 2007; John, Sharma, Sharma, & Kankane, 2007; Lavey et al., 2005). The beneficial effect of yoga on depression may explain the significant improvement in depressive symptoms seen in our stretching control group. This may help explain the absence of a difference in BDI-II change scores between the aerobic groups and SC. For future randomized control trials, we would recommend a different type of activity (e.g., lecture meetings) or a wait-list control rather than stretching exercise for the control condition to examine the effects of training intensity and mediating variables on symptoms of depression. Regardless of group assignment, all participants had significantly increased exercise self-efficacy after 10 weeks of training, but no change in depression coping self-efficacy when controlling for baseline scores. However, we found significant negative relationships between both types of self-efficacy and depressive symptoms at Weeks 5 and 10, indicating that higher levels of selfefficacy were associated with lower levels of depression. These results were similar to findings in previous studies on self-efficacy mechanisms (Bodin & Martinsen, 2004; Craft, 2005). Although this was not evidence of self-efficacy mediating the beneficial effects of exercise on depression, these results provide some support for further exploring both exercise self-efficacy and depression coping self-efficacy as potential mechanisms for the antidepressant effects of exercise. Future research should further examine these mechanisms using mediation analyses. In addition, an exercise self-efficacy instrument that addresses intensity, duration, and frequency would provide greater insight into the relationship between different training programs and changes in depression than the general exercise self-efficacy questionnaire applied in this study. There were several limitations to the study. First, participants in the aerobic groups had one supervised exercise session and two to four unsupervised sessions. We did not use a heart rate monitor or a step counter to monitor physical activity outside of supervised sessions and had to rely on self-report to measure the participants’ exercise behaviors and estimate the weekly energy expenditure using their activity diaries. It was possible for participants to overestimate the intensity and duration of exercise, or record extra exercise sessions. However, the significant increase in maximal VO2 in HI suggests that participants in HI indeed exercised at their recorded exercise intensity, duration, and frequency. In addition, participants were instructed to record their exercise session in detail (e.g., speed and time on treadmill, distance and time if walking outdoors) and not to count any breaks during their exercise sessions. These instructions reduced the likelihood of overestimation of exercise intensity and duration, and helped estimate participants’ weekly energy expenditure. In addition, participants were not required to have a diagnosis of depression to enroll in this study. Therefore, findings in this study may not reflect responses in women with clinical depression, although research conducted with clinically depressed populations resulted in similar reductions in BDI-II scores following involvement in an exercise program (Blumenthal et al., 1999; Craft, 2005). Also, the sample is relatively small compared to many exercise intervention studies, resulting in low statistical power, which may explain the finding of non-significant interaction effect for BDI-II scores. Based on the results of current study, we would have needed 72 participants (i.e., 24 participants per group) for adequate power to detect an interaction effect for BDI-II scores. Therefore, it is important for future research to replicate this study with larger samples to further test the relationship between exercise intensity and depression. In summary, both high and low intensity aerobic exercise, as well as yoga-based stretching exercise were associated with reductions in depressive symptoms after 10 weeks of training in sedentary depressed women. The reductions in depression did not differ significantly among the groups. A high intensity (65–75% of VO2R) aerobic exercise program appeared to be more effective in reducing symptoms of depression based on between group comparisons at Week 5 and Week 10, although there was no significant association between changes in aerobic capacity and changes in depressive symptoms. Further, exercise self-efficacy and depression coping self-efficacy were inversely associated with depressive symptoms at repeated assessments. These results suggest the importance of evaluating self-efficacy as a mediator of the relationship between exercise and depressive symptoms in future research utilizing a larger sample. References Ainsworth, B. E., Haskell, W. L., Whitt, M. C., Irwin, M. L., Swartz, A. M., Strath, S. J., et al. (2000). Compendium of physical activities: an update of activity codes and MET intensities. Medicine and Science in Sports and Exercise, 32(9 Suppl.), S498–S504. Azar, D., Ball, K., Salmon, J., & Cleland, V. J. (2008). The association between physical activity and depressive symptoms in young women: a review. Mental Health & Physical Activity, 1, 82–88. Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall. Bandura, A. (1997). Self-efficacy: The exercise of control. New York: W.H. Freeman. Beck, A. T., Steer, R. A., & Brown, K. (1996). Beck Depression Inventory (2nd ed.). San Antonio, TX: Harcourt Brace. Blumenthal, J. A., Babyak, M. A., Moore, K. A., Craighead, W. E., Herman, S., Khatri, P., et al. (1999). Effects of exercise training on older patients with major depression. Archives of Internal Medicine, 159, 2349–2356. Bodin, T., & Martinsen, E. W. (2004). Mood and self-efficacy during acute exercise in clinical depression. A randomized, controlled study. Journal of Sport & Exercise Psychology, 26, 623–633. Craft, L. L. (2005). Exercise and clinical depression: examining two psychological mechanisms. Psychology of Sport and Exercise, 6, 151–171. I.-H. Chu et al. / Mental Health and Physical Activity 2 (2009) 37–43 Craft, L. L., & Landers, D. M. (1998). The effect of exercise on clinical depression and depression resulting from mental illness: a meta-analysis. Journal of Sport & Exercise Psychology, 20, 339–357. Craft, L. L., & Perna, F. M. (2004). The benefits of exercise for the clinically depressed. Primary Care Companion to The Journal of Clinical Psychiatry, 6, 104–111. Dimeo, F., Bauer, M., Varahram, I., Proest, G., & Halter, U. (2001). Benefits from aerobic exercise in patients with major depression: a pilot study. British Journal of Sports Medicine, 35, 114–117. Dishman, R. K., Motl, R. W., Sallis, J. F., Dunn, A. L., Birnbaum, A. S., Welk, G. J., et al. (2005). Self-management strategies mediate self-efficacy and physical activity. American Journal of Preventive Medicine, 29, 10–18. Dunn, A. L., Trivedi, M. H., Kampert, J. B., Clark, C. G., & Chambliss, H. O. (2005). Exercise treatment for depression: efficacy and dose–response. American Journal of Preventive Medicine, 28, 1–8. Dunn, A. L., Trivedi, M. H., & O’Neil, H. A. (2001). Physical activity dose–response effects on outcomes of depression and anxiety. Medicine and Science in Sports and Exercise, 33, s587–s597. Elavsky, S., & McAuley, E. (2007). Physical activity and mental health outcomes during menopause: a randomized controlled trial. Annals of Behavioral Medicine, 33, 132–142. Fox, K. R. (1999). The influence of physical activity on mental well-being. Public Health Nutrition, 2, 411–418. Franklin, B. A., Whaley, M. H., Howley, E. T., Balady, G. J., & Grais, I. M. (Eds.). (2000). ACSM’s guidelines for exercise testing and prescription (6th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. Garcia, A. W., & King, A. C. (1991). Predicting long-term adherence to aerobic exercise: a comparison of two models. Journal of Sport and Exercise Psychology, 13, 394–410. Godin, G., & Shephard, R. J. (1985). A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Sciences, 10, 141–146. John, P. J., Sharma, N., Sharma, C. M., & Kankane, A. (2007). Effectiveness of yoga therapy in the treatment of migraine without aura: a randomized controlled trial. Headache: The Journal of Head and Face Pain, 47, 654–661. Kessler, R. C., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K. R., et al. (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). Journal of the American Medical Association, 289, 3095–3105. Lampinen, P., Heikkinen, R.-L., & Ruoppila, I. (2000). Changes in intensity of physical exercise as predictors of depressive symptoms among older adults: an eightyear follow-up. Preventive Medicine, 30, 371–380. Landers, D. M., & Arent, S. M. (2001). Physical activity and mental health. In R. N. Singer, H. A. Hausenblaus, & C. M. Janelle (Eds.), Handbook of sport psychology (2nd ed.). New York, NY: John Wiley and Sons. Lavey, R., Sherman, T., Mueser, K. T., Osborne, D. D., Currier, M., & Wolfe, R. (2005). The effects of yoga on mood in psychiatric inpatients. Psychiatric Rehabilitation Journal, 28, 399–402. 43 McAuley, E., Jerome, G. J., Elavsky, S., Marquez, D. X., & Ramsey, S. N. (2003). Predicting long-term maintenance of physical activity in older adults. Preventive Medicine, 37, 110–118. North, T. C., McCullagh, P., & Tran, Z. V. (1990). Effect of exercise on depression. Exercise and Sport Sciences Reviews, 18, 379–415. Paluska, S. A., & Schwenk, T. L. (2000). Physical activity and mental health: current concepts. Sports Medicine (Auckland, N.Z.), 29, 167–180. Perraud, S. (2000). Development of the Depression Coping Self-Efficacy Scale (DCSES). Archives of Psychiatric Nursing, 14, 276–284. Pollock, K. M. (2001). Exercise in treating depression: broadening the psychotherapist’s role. [Special issue]. Psychotherapy in Practice, 57, 1289–1300. Riolo, S. A., Nguyen, T. A., Greden, J. F., & King, C. A. (2005). Prevalence of depression by race/ethnicity: findings from the National Health and Nutrition Examination Survey III. American Journal of Public Health, 95, 998–1000. Seggar, L. B., Lambert, M. J., & Hansen, N. B. (2002). Assessing clinical significance: application to the Beck Depression Inventory. Behavior Therapy, 33, 253–269. Singh, N. A., Stavrinos, T. M., Scarbek, Y., Galambos, G., Liber, C., & Fiatarone Singh, M. A. (2005). A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences, 60, 768–776. Steer, R. A., Ball, R., Ranieri, W. F., & Beck, A. T. (1997). Further evidence for the construct validity of the Beck Depression Inventory-II with psychiatric outpatients. Psychological Reports, 80, 443–446. Teychenne, M., Ball, K., & Salmon, J. (2008). Associations between physical activity and depressive symptoms in women. International Journal of Behavioral Nutrition and Physical Activity, 5, 27. Ustun, T. B., Ayuso-Mateos, J. L., Chatterji, S., Mathers, C., & Murray, C. J. L. (2004). Global burden of depressive disorders in the year 2000. The British Journal of Psychiatry: the Journal of Mental Science, 184, 386–392. Veale, D., LeFevre, K., Pantelis, C., deSouza, V., Mann, A., & Sargent, A. (1992). Aerobic exercise in the adjunctive treatment of depression: a randomized controlled trial. Journal of the Royal Society of Medicine, 85, 541–544. deVries, H. A., Wiswell, R. A., Bulbulian, R., & Moritani, T. (1981). Tranquilizer effect of exercise. Acute effects of moderate aerobic exercise on spinal reflex activation level. American Journal of Physical Medicine, 60, 57–66. van Weert, E., Hoekstra-Weebers, J. E., May, A. M., Korstjens, I., Ros, W. J., & van der Schans, C. P. (2008). The development of an evidence-based physical selfmanagement rehabilitation programme for cancer survivors. Patient Education and Counseling, 71, 169–190. Wilbur, J., Vassalo, A., Chandler, P., McDevitt, J., & Miller, A. M. (2005). Midlife women’s adherence to home-based walking during maintenance. Nursing Research, 54, 33–40. Wilcox, S., Sharpe, P. A., Hutto, B., & Granner, M. L. (2005). Psychometric properties of the self-efficacy for exercise questionnaire in a diverse sample of men and women. Journal of Physical Activity and Health, 3, 285–297.