* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download OCCG Core Policy 1 Infection Control Policy and Programme
Onchocerciasis wikipedia , lookup
Henipavirus wikipedia , lookup
Toxoplasmosis wikipedia , lookup
West Nile fever wikipedia , lookup
Herpes simplex wikipedia , lookup
Middle East respiratory syndrome wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Hookworm infection wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Anaerobic infection wikipedia , lookup
Marburg virus disease wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Trichinosis wikipedia , lookup
Sarcocystis wikipedia , lookup
Hepatitis C wikipedia , lookup
Dirofilaria immitis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Lymphocytic choriomeningitis wikipedia , lookup
Fasciolosis wikipedia , lookup
Hepatitis B wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Oesophagostomum wikipedia , lookup
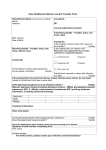
INSERT PRACTICE NAME HERE OCCG IPC Core Policy 1; Infection Prevention Policy and Programme Contents 1. Introduction 2. Statement from Practice Manager/Lead Doctor 3. Accountability and Responsibilities 3.1 Practice manager/Lead Doctor 3.2 Infection prevention lead 3.3 Decontamination lead 3.4 Individuals 3.5 Antimicrobial prescribing 3.6 Attached staff 3.7 Occupational health 4 Public Health England Centres 5 OCCG infection control team 6 Policies 7 Audit 8 Training and development 9 References 10 Appendix – example IPC Programme Date issued: August 2016 Date for review: August 2019 3 yearly or earlier if new guidance published Infection control programme 1 INSERT PRACTICE NAME HERE OCCG Core Policy 1 Infection Prevention and Control Policy and Programme 1. Introduction 1.1 All healthcare workers have a duty to minimise the risk of patients and staff acquiring infection. The management and organisation of Infection Prevention and Control of Health Care Associated Infections (HCAI) are set out in The Health and Social Care Act 2008: Code of Practice for the NHS on the Prevention and Control of Healthcare Associated Infections1. 1.2 This policy applies to all members of (name of practice). All staff, both clinical and non-clinical are required to adhere to the (name of practice) Infection Prevention and Control Policies and procedures and make every effort to maintain high standards of infection control at all times thereby reducing the burden of HCAI. This is an overarching policy and programme and is intended to outline how (name of practice) will deal with the complex issues with regard to infection prevention and control. It outlines the arrangements and responsibilities of all staff concerned in the provision of health care. 1.3 The prevention and control of infection is a key priority for the NHS and forms an important part of the (name of practice) Governance arrangements. The (name of practice) is monitored by adherence to standards by NHS England. 1.4 This policy sets out the commitment of the (name of practice) in its collective responsibility to minimise risks of infection and cross contamination within the practice. 1.5 An annual programme of infection prevention & control will be written and followed by the practice. 2 Statement by the Practice manager/lead doctor 2.1 Healthcare Associated Infections are not something that concerns only the infection prevention and control lead or indeed only the clinical staff. Everyone has a role to play in ensuring patient safety. 2.2 Prevention and Control of Infection is a core part of patient safety and our governance system. As a practice we will ensure compliance with legislation and national guidance for Infection Prevention and Control and cleanliness. 2.3 The practice will produce an infection prevention and control programme that will include: What infection prevention and control measures are needed in the practice What policies, procedures and guidance are required What induction and ongoing training is required for all staff The audit programme Infection control programme 2 INSERT PRACTICE NAME HERE 3 Responsibilities 3.1 Practice manager/lead doctor The Practice manager/lead doctor has the responsibility to ensure compliance with legislation and national guidance for Infection prevention and Control and for cleanliness1. This includes: Appoint an Infection Prevention and Control Lead (IPC Lead) Appoint a designated lead for cleaning and decontamination of the environment and equipment (nb this can be the IPC lead) Approval of an annual infection prevention and control programme Policy, procedure and guidance approval Appraise outcomes of action plans in relation to Infection Prevention and Control 3.2 3.3 Infection Prevention and Control Lead Advise the practice on the policies, procedures and guidance that are required and how they are to be disseminated and kept up to date Working with the practice manager to establish and facilitate the training requirements of all staff in relation to infection control. Prepare an annual statement and plan Keep up to date on developments in infection control Designated Decontamination lead Prepare policies and procedures for decontamination of the environment, equipment and reusable medical equipment Set out the type of products are used for successful cleaning and decontamination Training required to achieve the above 3.4 Individuals All staff have a responsibility to ensure they comply with local infection control policies and procedures. They should demonstrate patient safety and well-being as a priority within day to day activities. In particular: Staff must wash their hands or use alcohol gel between each patient contact Staff members have a duty to attend infection control training provided for them. 3.5 Antimicrobial Prescribing All prescribers should adhere to; The Oxfordshire CCG Prescribing Guidelines for the use of Antimicrobial Agents in Primary Care9.2 The Oxfordshire CCG Antimicrobial Guidelines Policy Statement. Document an indication and duration for each antimicrobial prescribed in the patients notes. Infection control programme 3 INSERT PRACTICE NAME HERE Adhere to recommendations as described in the DoH UK 5 year antimicrobial resistance strategy 9.3 Utilise toolkits such as the TARGET toolkit as recommended by RCGP9.4 These guidelines are based on evidence and local resistance patterns and so their prudent use will help to reduce the risk of infections from MRSA, Clostridium difficile and other resistant bacteria. Where sensitivities show a choice of antimicrobials, the one with the least risk to predispose patients to infection with Clostridium difficile or MRSA should be used. 3.6 Attached staff All staff attached to the practice have responsibility to ensure they comply with local infection control policies and procedures. They should demonstrate patient safety and well-being as a priority within day to day activities. In particular: Staff must wash their hands or use alcohol gel on entry and between each patient contact Staff members have a duty to attend mandatory infection control training provided for them by either the practice or their employer. 3.7 Staff Health Any significant injury or infection acquired at work must be reported to the Practice Manager and reported according to the practice incident reporting policy. Sharps injuries involving bodily fluids must be reported to the practice manager and the sharps injuries protocol must be followed. 4 Public Health England Centres (PHEC) The Health Protection Teams lead the Public Health England response to health protection related incidents. The team is comprised of Consultants in Communicable Disease Control (CCDC), Consultants Health Protection (CHP) and Health Protection Practitioners (HPPs and other supporting staff. Outbreaks and incidents of infection in the community will be monitored and investigated by the team and they will initiate and co-ordinate any necessary action to limit further spread. 5 OCCG Infection Control advice The OCCG infection control team is based at Jubilee House. Lead for Infection Prevention and Control 01865 336856 6 Policies Infection control programme 4 INSERT PRACTICE NAME HERE Policies relating to Infection prevention and control will be monitored for compliance through the annual audit. Policies will remain current for 3 years unless guidance changes. The practice manager / IPC lead will be responsible for reviewing the currency of policies. 7 Audit An annual audit of infection control should take place. This can be a selfassessment or an invited team. 8 Training and Development 8.1 The practice will ensure provision of training to clinical staff to enable them to carry out their duties and responsibilities relating to infection control this will include hand hygiene and infection control processes and procedures. This should occur on a 2 yearly basis. 8.2 The practice will ensure provision of training to non- clinical staff to enable them to carry out their duties and responsibilities relating to infection control. This should occur on a 2 yearly basis 8.3 9 Infection control will be included in new staff induction training. References Infection control programme 5 INSERT PRACTICE NAME HERE 9.1 Department of Health (2015) The Health Act 2008; Code of Practice for the Prevention and Control of Healthcare Associated Infections. Department of Health. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicy AndGuidance/DH_122604 9.2 OCCG Prescribing Guidelines for the use of Antimicrobial Agents in Primary Care http://occg.oxnet.nhs.uk/GeneralPractice/ClinicalGuidelines/Infectious%20Diseas es/Antimicrobials/Oxfordshire%20Antimicrobial%20ADULT%20Guidelines%20Pri mary%20Care%20January%202016%20v2.3.pdf 9.3 DoH (2015) UK 5 year antimicrobial resistance strategy https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/244 058/20130902_UK_5_year_AMR_strategy.pdf 9.4 TARGET toolkit http://www.rcgp.org.uk/TARGETantibiotics/ 9.5 Department of Health (2003), Winning Ways, Working together to reduce Healthcare Associated Infection in England. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/publicationsandsta tistics/publications/publicationspolicyandguidance/dh_4064682 9.6 NICE (2012) Healthcare associated infections; prevention and control in primary and community care https://www.nice.org.uk/guidance/cg139/chapter/1-guidance Infection control programme 6 INSERT PRACTICE NAME HERE 10 Appendix Example IPC Programme Practice annual infection control programme April (add year) –March (add year) Patient safety is a key objective of the practice philosophy and preventing infections is integral to this. The practice principle, medical, nursing and healthcare staff and all attached staff will work together to ensure an environment that is safe and clean and patients are protected from identifiable risks of acquiring infections. Objective Action Lead Reporting Outcome frequency There are systems to manage There is an infection prevention PM and monitor the prevention At practice programme in place and control of infection. governance An annual audit will take place PM/ meeting There is a nominated lead for infection Practice prevention and control. IPC lead There are the appropriate polices procedures and guidance in place to Annual review provide a clean, safe environment An annual statement will be presented Practice Annually (dateto the practice (date) IPC lead after April each year) There is a training programme in place Infection control programme All new staff will have infection prevention training as part of their induction All new staff will have hand hygiene training All clinical staff will have two yearly infection prevention training which will include hand hygiene training Practice IPC lead and Practice manager 7 A record of training will be kept and reviewed every 6 months. INSERT PRACTICE NAME HERE The practice will provide a safe, clean environment that prevents and controls infection. There is a system in place that keeps service users informed of the practice approach to infection prevention and control The practice will ensure that information is shared between healthcare providers on any infection that a service users may have (MRSA- C.diff etc) Staff will be protected from exposure to blood borne viruses through immunisation, safe management of exposure Infection control programme All non-clinical staff will have infection prevention training every two years There is a designated lead for cleaning and environmental decontamination There are documented cleaning programmes that are accessible and kept up to date There is a record of staff trained to carry out cleaning programmes A monitoring programme is in place for environmental cleaning There is an annual audit of decontamination processes The PPG/PLG is kept up to date with the approach the practice is taking to keep them informed. There is information available to patients on infections and risks of transmission (good hand hygiene, catch it - bin it - kill it) Ensuring confidentiality, any letters or referrals to other organisations will have relevant infection information included. A policy is in place for staff to follow There are posters in place for staff to follow in the event of a sharps injury so staff know what to do. PM Minimum annual audit; bi-annually preferable Decontami nation lead Practice IPC lead and PM Annual report Clinical and medical staff PM and Practice IPC lead 8 Annual audit of sharps and related injuries and outcome of INSERT PRACTICE NAME HERE and safe use and disposal of sharps and There is a local policy in place for antimicrobial prescribing and a system of audit is in place. Waste is managed and complies with the National Waste Guidance Environment. NOTE : Any information in relation to improving the practice environment to comply with the Code of Practice can be put in here. This could be refurbishment, rebuild, new equipment etc. and how the Infection control is factored into the build. Infection control programme This above will be checked as part of the infection control audit cycle All prescribers have access to the local prescribing guidelines An audit plan is in place. The practice reviews prescribing patterns and quarterly details sent by PCT. All waste is appropriately labelled Staff are trained to comply with waste systems A waste audit carried out Development of risk register for practice Replacement programme for damaged equipment response. Detail in the annual report Prescribing lead PM PM and Practice IPC lead 9