* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 6.1. Introduction and need for the study
Survey
Document related concepts
Transcript
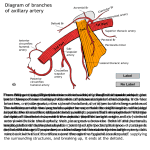
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA, BANGALORE. ANNEXURE-II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION DR. SAVITA KUMARI D/O RAMADHAR SINGH NAME OF THE CANDIDATE AND ADDRESS AT- BARKI DELHA, POONSAHAW GALI POST: GAYA R S, DISTRICT: GAYA BIHAR-823002 DR. SAVITA KUMARI (POST GRADUATE STUDENT) 1. DEPARTMENT OF ANATOMY, MANDYA INSTITUTE OF MEDICAL ADDRESS FOR CORRESPONDANCE SCIENCES, MANDYA-571 401 KARNATAKA. E-MAIL: [email protected] MOB: 9740621049 2. NAME OF THE MANDYA INSTITUTE OF MEDICAL INSTITUTION SCIENCES, MANDYA-571401 COURSE OF THE STUDY 3. 4. AND SUBJECT M.D. (ANATOMY) DATE OF ADMISSION TO THE COURSE 19-06-2012 “A STUDY OF BRANCHING PATTERN OF 5. TITLE OF THE TOPIC INTERNAL ILIAC ARTERY IN HUMAN CADAVERS” 6. Brief resume of intended work. 6.1. Introduction and need for the study: The internal iliac artery is the “artery of the pelvis”. Internal iliac artery is 4cm long begins at common iliac bifurcation at the level of lumbosacral intervertebal disc and anterior to the sacroiliac joint. It descends posteriorly to the superior margin of the greater sciatic foramen where it divides into an anterior trunk, which continues in the same line towards the ischial spine, and posterior trunk, which passes back to the greater sciatic foramen. Anterior to the artery is the ureter and, in females, the ovary and fimbriated end of the uterine tube. The internal iliac vein, lumbosacral trunk and sacroiliac joint are located posteriorly. Lateral boundary is formed by the external iliac vein seen between the artery and psoas major, and inferiorly to this is the obturater nerve. The parietal peritoneum is medial, separating it from the terminal ileum on the right and the sigmoid colon on the left .Tributaries of the internal iliac vein are also medial1. The anterior trunk branches of interal iliac artery are superior vesicle artery, inferior vesicle artery, middle rectal artery, obturator artery, vaginal artery, uterine artery, internal pudendal and inferior gluteal arteries. The branches of the posterior division are iliolumbar, lateral sacral and superior gluteal. Anterior& posterior divisions supply pelvic viscera, perineum, pelvic wall, gluteal region. Origin of terminal branches are subject to variation2. Variations in the branching pattern of internal iliac artery have long received attention of anatomists and surgeons. Knowledge of the anatomical variation is beneficial for the vascular surgeon & gynecologist for ligating the internal iliac artery or its branches during the pelvic surgery and also for the radiologists to perform and interpret angiograms of pelvic region. Hence the present study is being undertaken to present the anatomical knowledge (normal & variations) of internal iliac artery. 6.2. Review of literature: Internal iliac artery may be longer or shorter than usual its length varying from 2.5 cm to 7.5 cm. But it may be as short as 1.2 cm length of variation dependes on length of the common iliac; when they bifurcate higher than usual, the internal iliac is longer and may lie initially above the brim of the true pelvis. The length may also depend upon the internal iliac itself dividing higher or lower than usual into its branches. This division may occur anywhere between the brim of the pelvis and the upper border of the sacrociatic foramen. In some cases the branches arises without the artery dividing into an anterior and a posterior division or one more branches arise above the division. The internal iliac may give rise to the following: superior mesenteric vesicoprostatic prostatic, a common trunk for a superior vesical and a profunda penis, an independent arteria penis supplying the profunda penis arteries when the dorsal penis artery is a branch of the internal pundendal, and/or an inferior epigastric artery. Branches of the anterior and posterior divisions of the internal iliac may exchange origins3. Adachi classification Type I -The superior gluteal artery arises separately from the Internal iliac artery, the inferior gluteal and internal pudendal vessels are given off by a common trunk. Type II - The superior and inferior gluteal arteries arise by a common trunk and internal pudendal vessel separately. Type III - The three branches arise separately from the internal iliac artery. Type IV - The three arteries arise by a common trunk. The subtyping in this group is based on the sites of origin of the superior gluteal and the internal pudendal arteries from the parent stem. TypeV - The internal pudendal and the superior gluteal arteries arise from a common trunk and the inferior gluteal has a separate origin. In 1952 J. L Braithwaite studied on 169 specimen (108 male&61female) cadavers. Type I arrangement on Adachi's scale in 58% of cases, types III pattern being found in 22.5%, type II in 15.3%, type IV is least frequent 3.6%. Similar origin of vessels is noted on both sides in 52.7%. Obturater artery is more variable course4. In 1998, Yamaki conducted study on 645 pelvic halves of Japanese cadavers. The branching of the internal iliac artery was classified according to Adachi's classification (1928). Type I was predominant in accordance of with previous studies. During the course of this study, some branching forms were different from the types in Adachi's classification. Therefore, this classification was modified into 5 types and 19 groups. Type I-Group 1 was most frequently observed in the modified Adachi's classification; however, the frequency was less than 50% (46.8%). To clarify the basic branching pattern of the original internal iliac artery and to simplify the classification for medical purposes, a new classification system was designed. The superior gluteal, inferior gluteal and internal pudendal arteries were defined as the major branches of the internal iliac artery, and the umbilical artery excluded from this group. The branching of the internal iliac artery was classified into 4 groups. Almost 80% of the present specimens were included in Group A of the new classification , namely, the internal iliac artery dividing into two major branches, the superior gluteal artery and the common trunk of the inferior gluteal and internal pudendal arteries. This type of branching seemed to be the basic branching pattern for the original internal iliac artery5. In 2010, Tiago Bilhim studied imaging finding of the main branching patterns of the male internal iliac arteries, using different imaging modalities (angio MR, angio CT and digital angiography). Twentyone males (mean age 73.2 years) underwent imaging evaluation with MR angiography,CT angiography and digital substraction angiography to define the internal iliac artery anatomy before selective embolization of the pelvic arteries. Internal iliac arterie were classifed into four groups using the Yamaki classifcation(modifed from the Adachi’s classifcation). Twenty-six pelvic sides were classifed as Group A(61.9%), 13 as Group B (31%) and 3 as Group C (7.1%) with no cases of Group D found. Group A was the most frequent internal iliac artery branching pattern6. In 2010 Dr. Shivakumar AH studied on 40 adult cadaver pelvis. Type 1 is predominant in this study 89%, type II is 11%. Total absence of typeIII & typeIV of adachi classification. Average length was 2 cms to 6.2c.m. Origin of artery was variable in about 10 cases (34%).7 In 2011 Naveen studied on 60 human bisected pelvises irrespective of their side and sex. The branching patterns were studied and demonstrated as per the guidelines of Adachi. The origin of internal iliac artery was at the level of S1 vertebra in majority (58.3%) of the cases. The average length of internal iliac artery was 37 ± 4.62 mm (range, 13-54 mm). The type I pattern of the internal iliac artery was most common (83.5%) followed by types III and II. The type IV and V pattern of adachi were not observed8. In 2012 Ramakrishnan PK studied origin of the three large parietal branches of the internal iliac atery and were investigated in 50 cadaver specimens (40 male and 10 female). The origins of the major parietal branches conformed to a Type I arrangement on the Adachi scale in 60 % of cases, a Type III pattern being found in 30 % and a type II pattern in 8 %. Type IV is less frequent and occurs in 2 % of specimens. In 33.3 % of instances, a similar origin of branches is noted on both sides9. 6. 3. Objective of the study: 1. To describe the branching pattern of internal iliac artery by dissection method. 2. To describe the origins and course variations in the pattern of branches of internal iliac artery. 7. Materials and Methods: 7.1. Source of data: The present study will be carried on 50 bisected pelvises from embalmed cadavers of both gender from Department of Anatomy, Mandya Institute of Medical Sciences, Mandya. Study design: Descriptive study. Study area: Department of Anatomy Mandya Institute of Medical Sciences, Mandya. Sample size: 50 bisected Pelvises. 7.2. Method of collection of data: Formalin-fixed pelvis specimens will be dissected. Finer dissection of internal iliac artery and its branches will be carried out. The observation will be recoded and photographed. Inclusion Criteria: Pelvis from cadavers, irrespective of age, sex will be included in this study. Exclusion Criteria: Pelvis with degenerative or pathological deformities or injuries will be excluded from this study. Statistical Analysis: The collected data will be entered in excel sheet and analysed using Epi-info/SPSS software and the descriptive statistics, ‘chi-square’ test, t’ test and other applicable statistical tests will be applied for analysing the data as applicable. . 7.3. Does the study require any investigations or interventions to be conducted on patients or other humans or animals? NO 7.4. Has ethical clearance been obtained from your institution? Yes - Submitted 8. List of references. 1. Standring S. Gray’s Anatomy the anatomical basis of clinical practice. 40th ed. New York: Elsevier Churchill Livingstone; 2008.p.1086-87. 2. Snell RS. Clinical anatomy by regions . 8th ed. Philadelphia: Lippincott, William & Wilkins; 2008. p. 328-29. 3. Bergman RA, Thompson SA, Afifi AK and Saaden FA. Compendium of human anatomic variation. Baltimore- Monich: Urban and Schwarzenberg; 1988.p.84-85. 4. Braithwaite JL. Variations in origin of the parietal branches of the internal iliac artery. J Anat .1952;86:423-430. 5. Yamaki K, Saga T, Doi Y, Aida K, Yoshizuka M. A statistical study of the branching of the human internal iliac artery. Kurume Med J. 1998;45:333-340. 6. .Tiago Bilhim ,Diogo casal,Andrea Furtado,Diogo Pais,Joao Erse Goyri O’Neill,Joya Martins Pisco. Branching patterns of the male internal iliac artery imaging findings Anatomic bases of medical, radiological and surgical techniques .2010. 7. Shivakumar AH, Raju GM, Sathymurthy B, Vijayanath V. Internal iliac artery& its variation. Anatomica Karnataka. 2010; 4(1): 10. 8. Naveen NS, Murlimanju BV, Kumar V, Jayanthi KS, Rao K, Pulakunta T. Morphological Analysis of the Human Internal Iliac Artery in South Indian Population. Online J Health Allied Scs. 2011; 10(1): 11. 9. Ramakrishnan PK, Elezy MA. Variations in the branching pattern of internal iliac artery. Anatomica Karnataka. 2012; 6 (1): 12. 9 SIGNATURE OF THE CANDIDATE THE STUDY IS BEING CARRIED OUT FOR UNDERSTANDING CLINICAL RELEVANCE THE OF THE ARTERIAL SUPPLY TO STRUCTURES OF PELVIS AND PROVIDE SUPPORTIVE EVIDENCE FOR THE EXISTING DATA AND REPORT THE 10 REMARKS OF THE GUIDE NEWER FINDINGS FOR THE BENEFIT OF SURGEONS GYNAECOLOGIST AND DURING SURGERIES IN PELVIC REGION AND RADIOLOGISTS PERFORMING ARTERIAL DIAGNOSTIC STUDY AND THERAPEUTIC INTERVENTIONS USING INTERNAL ILIAC ARTERY. 11 NAME AND DESIGNATION OF: DR. M.S. TRINESH GOWDA PROFESSOR & HOD, 11.1 GUIDE DEPARTMENT OF ANATOMY, MANDYA INSTITUTE OF MEDICAL SCIENCES, MANDYA-571401. 11.2 SIGNATURE 11.3 CO-GUIDE 11.4 SIGNATURE DR. M.S. TRINESH GOWDA 11.5 HEAD OF THE DEPARTMENT PROFESSOR & HOD, DEPARTMENT OF ANATOMY, MANDYA INSTITUTE OF MEDICAL SCIENCES, MANDYA-571401. MOB: 9901253179 EMAIL: [email protected] 11.6 SIGNATURE 12 12.1 REMARKS OF DEAN AND PRINCIPAL DR. DR. B. DEVANAD DIRECTOR, MANDYA INSTITUTE OF MEDICAL SCIENCES, MANDYA-571 401. 12.2 SIGNATURE Date: 05. 11. 2012 Mandya From Dr. Savita Kumari Post Graduate Student Department of Anatomy MIMS, Mandya To The Director / Chairman, Institutional Scientific Committee, MIMS, Mandya. Through: Professor & HOD of Anatomy, MIMS, Mandya. Respected Sir, Sub: Submission of synopsis of my research study entitled “A STUDY OF BRANCHING PATTERN OF INTERNAL ILIAC ARTERY IN HUMAN CADAVERS”. - Reg. --With reference to the above subject, I am herewith submitting the copy of synopsis of my research study entitled “A STUDY OF BRANCHING PATTERN OF INTERNAL ILIAC ARTERY IN HUMAN CADAVERS”. (4 Copy enclosed) for your kind perusal and needful action (to be forwarded to RGUHS). Kindly oblige and do the needful. Thanking you, Yours faithfully, (DR. SAVITA KUMARI) Post Graduate Student (2012 batch), Department of Anatomy MIMS, Mandya Date: 2. 11. 2012 Mandya From Dr. Savita Kumari Post Graduate Student Department of Anatomy MIMS, Mandya To The Chairman, Institutional Ethical clearance Committee, MIMS, Mandya. Through: Professor & HOD of Anatomy, MIMS, Mandya. Respected Sir, Sub: Submission of synopsis of my research study entitled “STUDY OF INTERNAL ILIAC ARTERY COURSE AND ITS BRANCHING PATTERN IN HUMAN CADAVER”. For ethical clearance -Reg. --With reference to the above subject, I am herewith submitting the copy of synopsis of my research study entitled “STUDY OF INTERNAL ILIAC ARTERY COURSE AND ITS BRANCHING PATTERN IN HUMAN CADAVER” (Copy enclosed) for ethical clearance. This is for your kind perusal and needful action. Kindly oblige and do the needful. Thanking you, Yours faithfully, (DR. SAVITA KUMARI) 1 year Post Graduate Student (2012 batch), Department of Anatomy MIMS, Mandya st