* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Neuroleptics (Anti-psychotic Drugs)
Survey
Document related concepts
Drug design wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Toxicodynamics wikipedia , lookup
Drug discovery wikipedia , lookup
Environmental impact of pharmaceuticals and personal care products wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Chlorpromazine wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Antipsychotic wikipedia , lookup
Transcript
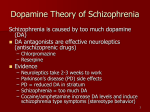
Neuroleptics (Anti-psychotic Drugs) Kaukab Azim, MBBS, PhD Drug List Typical Neuroleptics (First generation anti-psychotics) Phenothiazines Chlorpromazine Butyrophenones Haloperidol Thioridazine Atypical Neuroleptics (second Generation anitpsychotics Others Thiotixene Clozapine Molindone Olanzapine Fluphenazine Qietiapine Prochlorperazine* Risperidone Aripiprazole * Will be covered in another lecture Learning Outcomes By the end of the course the students will be able to ☛ Outline the dopamine hypothesis of schizophrenia. ☛ Explain the mechanism of action of each drug in each class. ☛ Describe the antipsychotic action of neuroleptics. ☛ List the main pharmacokinetic features of neuroleptics ☛ Outline the use of depot preparations of fluphenazine and haloperidol ☛ Describe the main adverse effects of neuroleptics ☛ List the main contraindications of neuroleptics ☛ Outline the main therapeutic uses of neuroleptics. Pharmacodynamics of Neuroleptics Mechanism of action ☛ Neuroleptics block many different receptors. ☛ The therapeutic effects of neuroleptics are though to result from competitive blockade of dopamine (mainly D2) and/or serotonin (mainly 5-HT2A) receptors. ☛ The adverse effects of neuroleptics seem to result from the blockade of D2 receptor in the substantia nigra as well as from blockade of a variety of receptors both in the central and autonomic nervous system Pharmacodynamics of Neuroleptics Neuroleptic can be broadly classified into the following groups: 1. Typical agents ☛ (which can be further subdivided in low potency and high potency agents) ☛ These drugs have high D2 antagonism and low 5-HT2A antagonism. 2. Atypical agents ☛ These drugs have low (clozapine) or moderate D2 antagonism and high 5-HT2A antagonism. Pharmacodynamics of Neuroleptics Pharmacological effects a.In normal individuals: ☛ Dysphoric effects are common (this can explain why this drugs have negligible abuse liability) b. In schizophrenic patients ☛ Positive schizophrenic symptoms(delusion,hallucinations & thought disorders) usually subside in 1-4 weeks and are about equally affected by typical and atypical agents. ☛ Negative schizophrenic symptoms(withdrawal,blunted emotions & reduce ability to relate to people) are minimally affected by typical neuroleptics but more so by atypical neuroleptics (the higher blockade of 5-HT2 receptors may contribute to this effect). Pharmacodynamics of Neuroleptics Other effects ☛ Inhibition of nausea and vomiting (due to blockade of D2 receptors mainly in the CTZ, but also in the stomach ☛ Inhibition of thermo-regulation (due to inhibition of the hypothalamic thermostat) Pharmacokinetics of Neuroleptics ☛ Variable oral bioavailability (0.25-0.70) ☛ Large Vd. ☛ Extensive metabolism by the liver. ☛ Long half-lives (12-55 hours) for most compounds . ☛ Administered PO, IM , IV. For some compounds depot preparations are available (i.e. fluphenazine decanoate, haloperidol decanoate)(depot:It is a special preparation of the medication, which is given by injection. The medication is slowly released into the body over a number of weeks) Receptor Affinity of Typical and Atypical Neuroleptics D2 D4 5-HT2A H1 M Alpha1 Typical agents (first generation neuroleptics) Chlorpromazine +++ 0 ++ ++ +++ +++ Thioridazine +++ 0 ++ + +++ +++ Fluphenazine +++ 0 + 0 0 + Haloperidol +++ 0 + 0 0 + Atypical agents (second generation neuroleptics) Clozapine ++ ++ +++ + +++ +++ Aripiprazole +++ 0 ++ + 0 ++ Quitiapine + + ++ + + ++ Olanzapine ++ + +++ ++ +++ ++ Risperidone +++ + +++ + 0 +++ Relative incidence of Adverse Effects of Neuroleptics Extra Pyramidal Symptoms Prolactin Elevation Sedation Anticholinergic Effects Postural Hypertension Medium Present High High High Thioridazine Low Present High High High Fluphenazine High Present Low Low Low Haloperidol High Present Low Low Low Clozapine Very Low None High High High Quetiapine Very Low None Medium Low Medium Olanzapine Very Low None Medium High Medium Risperidone Medium Present Medium Low Medium Aripiprazole Very Low None Low Low Medium Drug Chlorpromazine Extrapyramidal Adverse Effects of Neuroleptics Syndrome Features Proposed mechanism Treatment Acute dystonia Spasms of muscles of tongue, face, and neck Unknown Anti-Parkinson Drugs Akathisia Motor restlessness Unknown Anti-Parkinson Drugs Benzodiazepines Propranolol Parkinsonism Bradykinesia, rigidity, tremor Dopamine Antagonism Anti-Parkinson Drugs Tardive dyskinesia Oral-facial, dyskinesia, choreoathetosis, Dystonias Up-regulation of D2 receptors Prevention. Treatment is unsatisfactory Etiology Tardive Dyskinesia Long term treatment with typical neuroleptics endowed with strong extrapyramidal effects (the risk of the syndrome is much lower with atypical neuroleptic) Symptoms and signs ☛ Tardive dyskinesia is characterized by: a. The buccal-lingual masticatory syndrome (grimacing(foul smell), chewing, tongue protrusion, lip smacking(make a noise with the lip), puckering(gather into a small wrinkles) b. Choreiform(jerky involantary movement), athetoid(Twist) or rhythmic movements of neck and trunk (torsion and torticollis) arms and legs (pill rolling, toe tapping and writhing(Twist) Tardive Dyskinesia Clinical course and prognosis ☛ Early signs of tardive dyskinesia can be reversible ☛ If the disease is not detected or allowed to persist, it can become irreversible even with drug discontinuation. Therapy ☛ Prevention is important ☛ No drug treatment is satisfactory. ☛ Switching to an atypical neuroleptic (clozapine) is the favored first-line therapeutic strategy. CNS Adverse Effects of Neuroleptics ☛ Sedative effects, usually perceived unpleasant by normal individuals (dysphoria, dizziness). ☛ Extrapyramidal effects. ☛ Seizures,(neuroleptics lower the convulsive threshold).The risk is substantial with clozapine (2-5%). ☛ Neuroleptic malignant syndrome (catatonia(person become mute or stuporous), stupor(a condition of near unconsciousness), fever, unstable blood pressure, myoglobinuria). It can be fatal. Dantrolene is the drug of choice, bromocriptine may help. Gastrointestinal system ☛ Xerostomia, constipation. ☛ Cholestatic jaundice (mainly with chlorpromazine) ☛ Sialorrhea (with clozapine. Up to 70 %) Adverse Effects of Neuroleptics Genitourinary system ☛ Urinary retention, urinary incontinence. ☛ Sexual dysfunction (erectile dysfunction, ejaculatory abnormalities). Metabolic/Endocrine system ☛ Hyperprolactinemia (can lead to amenorrhea, galactorrhea, anovulation in women, gynecomastia and azoospermia in men) ☛ Weight gain (mainly with clozapine and olanzapine) ☛ Hyperglycemia, diabetes (mainly with clozapine and olanzapine) ☛ Poikilothermia (with high doses) Adverse Effects of Neuroleptics Cardiovascular system ☛ Orthostatic hypotension (manly with lower potency drugs) ☛ Cardiac arrhythmias (mainly with thioridazine) [patients with long Q-T intervals are at greater risk] ☛ Myocarditis (with clozapine. The disease can be lethal) Other adverse effects ☛ Cornea, lens and retinal deposits (mainly with thioridazine) ☛ Blurred vision ☛ Urticaria, skin rash (phenothiazines, 1-5%). ☛ Photosensitivity (phenothiazines) ☛ Agranulocytosis (with clozapine. About 1%) Neuroleptic Drug Interactions of Clinical Importance Neuroleptic Interacting drug Effect of the interaction ☛ All Class 1 and class 3 anti-arrhythmics ☛ Quinolones Life threatening arrhythmias Low potency typical and most atypicals Anti-cholinergics Increased anti-muscarinic effects Phenothiazines SSRIs Inhibition of phenothiazine metabolism Haloperidol Azoles Inhibition of haloperidol metabolism Haloperidol Lithium Extrapyrimidal effects and/or lithium toxicity are increased Clozapine Caffeine Inhibition of clozapine metabolism Clozapine SSRIs Inhibition of clozapine metabolism Clozapine Ritonavir Strong inhibition of clozapine metabolism Risperidone SSRIs Inhibition of risperidone metabolism Summary of Adverse Effects of Neuroleptics Typical neuroleptics ☛ Low potency drugs (most phenothiazines and thioxanthenes) have low extrapyramidal effects and high or intermediate sedative, antimuscarinic and hypotensive effects. ☛ High potency drugs (fluphenazine, prochlorperazine, butyrophenones) have high extrapyramidal effects and low sedative, antimuscarinic and hypotensive effects. ☛ All drugs increase serum prolactin levels. ☛ All drugs, but thioridazine, have good antiemetic effects. ☛ All drug can cause cardiac arrhythmias, due to an increase in QT intervals. Summary of Adverse Effects of Neuroleptics Atypical neuroleptics ☛ All drugs have low or negligible extrapyramidal effects ☛ All drugs have negligible effects on serum prolactin levels. ☛ All drugs can cause cardiac arrhythmias, due to an increase in QT intervals ☛ Most drugs have significant sedative, antimuscarinic and hypotensive effects. Contraindications and Precautions of Neuroleptics Contraindications / Precautions Explanations States of CNS depression Addictive effects Parkinson’s disease Blockade of D2 receptors can worsen the disease Seizure disorders Neuroleptic lower the seizure threshold Catatonia The risk of neuroleptic malignant is increased Long Q-T intervals, cardiac arrhythmias The risk of polymorphic ventricular tachycardia is increased Glaucoma Several neuroleptics have pronounced antimuscarinic effects Catatonia is a state of neurogenic motor immobility, and behavioral abnormality manifested by stupor. Contraindications and Precautions of Neuroleptics Contraindications / Precautions Explanations Bone Marrow suppression (clozapine) The risk of clozapine induced agranulocytosis is increased Hypovolemia, hypotension Several neuroleptics have alpha1 blocking activity Prostatic hypertrophy Several neuroleptics have pronounced antimuscarinic effects History of breast cancer Some breast cancers are prolactin-dependent Elderly Sensitivity to anti-cholinergic effects is increased. Therapeutic Uses of Neuroleptics Psychiatric indications ☛ Acute psychosis (manic phase of bipolar disorder, etc.) ☛ Agitation, delirium (in mentally retarded or demented patients) ☛ Irritability, in autistic children and adolescents (risperidone) ☛ Schizophrenia, schizoaffective disorders ☛ Tourette’s syndrome ☛ Huntington’s disease ☛ Alcoholic hallucinosis Therapeutic Uses of Neuroleptics Nonpsychiatric indications ☛ Nausea and vomiting (some phenothiazines) ☛ Neuroleptanalgesia (droperidol & fentanyl) ☛ Pruritus (promethazine) Notes ☞ Atypical neuroleptics seem to have higher efficacy, particularly for negative symptoms, cognition and mood. However the issue is still controversial. ☞ Only clozapine has shown superiority over other neuroleptics in randomized clinical trials for the management of treatment resistant schizophrenia.