* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download 2. Parenchymal Cells
Survey
Document related concepts
Transcript
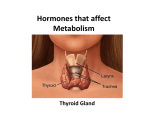
II. THYRIOD GLAND Anatomically consists from two lobes communicated by isthmus. 1. Capsule: the capsule of thyroid gland consists of a thin collagenous c.t. in all animals except in large ruminants and swine. their septa extend into the substance of the gland, subdividing it into lobules. 2. Parenchymal Cells: the parenchymal cells of the thyroid gland composed from Follicular Cells in stimulating phase are (simple cuboidal epithelium with microvilli) while in resting these epithelial cells are squamous & Parafollicular Cells (clear cells) located at the periphery of the follicles which are source of calcitonin. 3. Connective tissue: consists of interfollicuar connective tissue of well vascular . Dr.dhyaa 1 Histo-Physiology: The iodide from blood stream is actively transported into follicular cells at their basal aspect via iodide pumps. The iodide is oxidized by thyroid peroxidase on the apical cells membrane and bound to tyrosine producing of thymoglobulin(colloid)which rearranged to form tri iodothyronine (T3) and tetraiodothyronine or thyroxin (T4) which stimulated protiens synthesis. Release: the binding of TSH to receptors on the basal aspect of plasma membrane induce follicular cells to become tall cuboidal cells to form psedopods on their apical cell mem. That engulf and endocytose colloid –filling vesicle then T3&T4 are removed from thymoglobulin, liberate into the cytosol and release at the basal aspect of follicular cells into perifollicular capillaries. The enlargement of thyroid gland is referred to hyper plastic goiter. Dr.dhyaa 2 III. PARATHYROID GLAND This gland is presented adherent to thyroid gland. And separated from it by c.t. capsule •Capsule: consist from DICT as in thyroid gland in animals. •Parenchymal cells: 1. Chief Cells: are numerous small cells with large nuclei composed of two types of cells, dark and light acidophilic cytoplasmic that form cords these cells containing glycogen granules with lipid droplets. 2. Oxyphils: are large very light acidophilic and much fewer in numbers than chief cells. 3. Syncytial cells: are small and dark with dark nuclei with acidophilic cytoplasm. Dr.dhyaa 3 Histo-Physiology: the Parathyroid hormone (PTH) produce by chief cells is responsible maintaining proper calcium ion balance, a drop in blood calcium concentration activated a feed back mechanism that stimulated chief cell secretion PTH which stimulate osteioblast that released osteoclast stimulating factors which followed by bone resorption, in kidneys the PTH prevent urinary calcium loss, also control calcium uptake from intestine Dr.dhyaa 4