* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Locomotor Effects of Acute and Repeated Threshold Doses of
Survey
Document related concepts
Drug design wikipedia , lookup
Drug discovery wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacognosy wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Theralizumab wikipedia , lookup
Neuropharmacology wikipedia , lookup
Transcript
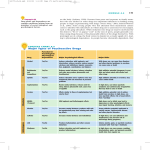
0022-3565/01/2963-876 –883$3.00 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS Copyright © 2001 by The American Society for Pharmacology and Experimental Therapeutics JPET 296:876–883, 2001 Vol. 296, No. 3 3300/887799 Printed in U.S.A. Locomotor Effects of Acute and Repeated Threshold Doses of Amphetamine and Methylphenidate: Relative Roles of Dopamine and Norepinephrine RONALD KUCZENSKI and DAVID S. SEGAL Department of Psychiatry, School of Medicine, University of California at San Diego, La Jolla, California Received September 6, 2000; accepted November 29, 2000 This paper is available online at http://jpet.aspetjournals.org Stimulant medications were first introduced in the treatment of children with attention deficit hyperactivity disorder (ADHD) in 1937. With the exception that methylphenidate (MP) has replaced amphetamine (AMPH) as the primary stimulant, the clinical use of these drugs has remained essentially unchanged. In recent years, however, the prescribed use of MP has risen dramatically, prompting heightened concerns of potential adverse long-term consequences arising from the prolonged exposure to this drug in children with ADHD. In this regard, one long-term consequence of the repeated administration of AMPH-like stimulants is an augmentation of some stimulant-induced behaviors in response to subsequent drug challenge (Robinson and Becker, 1986; Segal and Kuczenski, 1994). This augmentation, portions of which persist after prolonged periods of drug abstinence, has generally been referred to as behavioral sensitization, and it has been suggested that this process may be implicated in the development of stimulant addiction/abuse (Robinson and Berridge, 1993). Sensitization has been extensively documented following repeated administration of moderate-to-high doses of AMPH and This work was supported by U.S. Public Health Service Grant DA-01568. longed exposure to this drug, we examined whether changes in the locomotor response occurred with repeated administration of these stimulant doses. Threshold doses of methylphenidate (0.5–1.0 mg/kg) or amphetamine (0.1– 0.25 mg/kg) were administered twice daily, and then animals were tested in response to 2.5 mg/kg methylphenidate or 0.5 mg/kg amphetamine. Our results provide evidence that low-dose stimulant administration can result in the development of behavioral sensitization, which is evident in the subsequent behavioral response to the drug. The relevance of these data to the therapeutic uses of these drugs is discussed within the context of the many variables that can affect the behavioral and neurochemical responses to stimulants. cocaine (for reviews, see Robinson and Becker, 1986; Segal and Kuczenski, 1994; White and Kalivas, 1998). In contrast, fewer studies have characterized the effects of repeated MP, and results have been inconsistent. For example, some investigators have reported an increased locomotor response (Gaytan et al., 1997a; Sripada et al., 1998), whereas others have not (Crawford et al., 1998; Izenwasser et al., 1999). Likewise, an augmented stereotypy response has been observed by some (Browne and Segal, 1977; Crawford et al., 1998) but not others (McNamara et al., 1993; Izenwasser et al., 1999). Therefore, based on the available animal data it is not possible to conclude that repeated MP results in the same pattern of behavioral augmentation that has been well documented for the other amphetamine-like stimulants. Furthermore, in assessing the possible consequences of long-term MP treatment in children, it is important to note that a variety of factors, including drug dose, route, and pattern of administration, and chronicity can influence both the qualitative and quantitative features of the development and/or expression of chronic stimulant-induced behavioral and neurochemical alterations (for reviews, see Robinson and Becker, 1986; Segal and Kuczenski, 1994; White and Kalivas, ABBREVIATIONS: ADHD, attention deficit hyperactivity disorder; MP, methylphenidate; AMPH, amphetamine; DA, dopamine; NE, norepinephrine; 5HT, serotonin; AUC, area under the curve. 876 Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 ABSTRACT The prescribed use of methylphenidate (Ritalin) in the treatment of attention deficit hyperactivity disorder has risen dramatically in recent years. The relative roles of dopamine, norepinephrine, and serotonin in the therapeutic action of these drugs was assessed by comparing the responses of extracellular nucleus accumbens dopamine and serotonin and hippocampus norepinephrine to the acute administration of low methylphenidate and amphetamine doses. The comparative neurochemical profiles in response to methylphenidate and amphetamine suggest that the norepinephrine effects may play an important role in the therapeutic effects of low doses of psychostimulants. In addition, to assess possible long-term consequences of pro- Psychostimulant Threshold Doses: Behavior and Neurochemistry Experimental Procedures Subjects. Male Sprague-Dawley rats, weighing 325 to 350 g at the beginning of drug treatment, were housed for at least 1 week before experimental manipulation in groups of two or three in wire mesh cages, with ad libitum access to food and water, in a temperature- and humidity-controlled room, maintained on a 14-h light (5:00 AM–7:00 PM), 10-h dark cycle. Animals were obtained from Simonsen Labs (Gilroy, CA). All studies adhered to animal welfare guidelines (Principles of Laboratory Animal Care, National Institutes of Health Publication 85-23). Apparatus. Behavior was monitored in custom-designed activity chambers (Segal and Kuczenski, 1987). Briefly, each of the chambers was located in a sound-attenuated cabinet maintained on a 14-h/10-h light/dark cycle with constant temperature (20°C) and humidity (55 ⫾ 5%). Each chamber consisted of two compartments: an activity/ exploratory compartment (30 ⫻ 20 ⫻ 38 cm) and a smaller “home” compartment (14 ⫻ 14 ⫻ 10 cm) in which food and water were available ad libitum. Movements of the animal between quadrants within the activity/exploratory compartment (i.e., crossovers) and rearings against the wall, as well as eating and drinking and other vertical (e.g., contact with a hanging stimulus) and horizontal movements (e.g., intercompartment crossings) were monitored continuously by computer. In addition to the computer-monitored behaviors, representative animals (n values ⫽ 5–7) were simultaneously videotaped for 60 s at successive 5-min intervals throughout the response to assess the qualitative features of the response. The appearance of responses or behavior patterns, undetectable by our automated methods, was noted by the rater after each sampling interval. Drugs. Drugs were dissolved in saline. Methylphenidate HCl (National Institute on Drub Abuse, Rockville, MD) was administered i.p., and amphetamine SO4 (Sigma, St. Louis, MO) was administered s.c. Doses represent the free base. Methods (See Results for Specific Details). Three days before the beginning of drug treatment, animals were placed in individual experimental chambers where they remained for the duration of the experiment. For all experiments, n values ⫽ 9 to 11/group. To facilitate habituation to the chambers and procedures, animals were handled and injected with saline at least once a day. During the remainder of the day and night, animals were not disturbed and their behavior was continuously monitored. Throughout the remaining phases of each study, control animals were administered daily saline injections equivalent in number of injections to the experimental groups. For dialysis studies, animals were stereotaxically implanted with guide cannulae using procedures previously described in detail (Kuczenski and Segal, 1989). Guide cannulae extended 2.6 mm below the surface of the skull and were aimed at the dorsal hippocampus (3.8 mm posterior to bregma, 2.0 mm lateral, and 4.0 mm below dura) and the nucleus accumbens (2.2 mm anterior, 1.5 mm lateral, 7.8 mm below dura). Following surgery, animals were housed individually and allowed at least 1 week to recover before receiving any treatment. On the day before the experimental day (3:00 – 4:00 PM), each rat was placed in the dialysis chamber and the dialysis probes were inserted to allow for acclimation to the test environment and for adequate equilibration of the dialysis probes. The dialysis chambers were essentially identical to the behavioral chambers described above, with the exceptions that the home compartment and hanging stimulus were removed to prevent interferences introduced by the dialysis methodology. Concentric microdialysis probes were constructed of Spectra/Por hollow fiber (mol. wt. cut-off 6000, 250-m o.d.) according to the method of Robinson and Whishaw (1988) with modifications (Kuczenski and Segal, 1989). The length of the active probe membrane was 2 mm for hippocampus and 1.5 mm for nucleus accumbens. Probes were perfused with artificial cerebrospinal fluid (147 mM NaCl, 1.2 mM CaCl2, 0.9 mM MgCl2, 4.0 mM KCl) delivered by a microinfusion pump (1.5 l/min) via 50 cm of Micro-line ethyl Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 1998). In this regard, the daily doses of stimulants commonly used to treat children with ADHD, 0.5 mg/kg MP and 0.25 mg/kg AMPH (Patrick and Markowitz, 1997), typically administered orally twice daily, are near threshold for the induction of locomotor activation in rodents, and are substantially below conventional preclinical treatment doses used in studies of sensitization. Two published reports used stimulant doses within these clinical ranges: McNamara et al. (1993) (1 mg/kg MP) and West et al. (1999) (0.25 mg/kg AMPH) and both reported the absence of sensitization when the test and pretreatment doses were identical. However, the dose of drug used to test for the expression of a sensitized response might be a significant factor, and neuronal adaptations to repeated low-dose pretreatment may become evident in the response to a higher challenge dose. Within the context of a sensitization model for addiction, augmentation of higher dose effects would still be consistent with an increase in the incentive value of the stimulant (Robinson and Berridge, 1993), thus perhaps increasing the likelihood of stimulant abuse. With regard to underlying mechanisms, most evidence implicates the effects of psychostimulants on dopamine (DA) pathways in the treatment of ADHD (Pliszka et al., 1996). In addition, stimulant-induced effects on both norepinephrine (Florin et al., 1994) and serotonin (Segal, 1976; Jacobs and Fornal, 1997) have been implicated in the expression of stimulant-induced behaviors, and some evidence suggests possible roles for both these transmitters in the therapeutic efficacy of stimulants in the treatment of ADHD (Biederman and Spencer, 1999). One approach to assessing the possible role of the various stimulant-induced neurochemical changes is to compare and contrast the effects of AMPH and MP at therapeutically relevant doses. In this regard, our previous comparisons of the behavioral and neurochemical responses to moderate doses of AMPH and MP indicated that both drugs promoted profound effects on DA and NE systems (Florin et al., 1994; Kuczenski and Segal, 1997), although differential drug-specific dose-response relationships for the two transmitters were observed. In contrast, although we showed that moderate-to-high doses of AMPH can affect regional extracellular serotonin (5HT) (Kuczenski and Segal, 1989), no acute or chronic dose of MP altered extracellular concentrations of this transmitter (Kuczenski and Segal, 1997; Segal and Kuczenski, 1999), consistent with the relatively low affinity of MP for the 5HT transporter (Gatley et al., 1996). To gain insight into the relative roles of DA and NE in the therapeutic action of these drugs, we compared the nucleus accumbens DA and hippocampus NE responses to the acute administration of threshold MP and AMPH doses. In addition, studies were designed to further assess possible changes in behavioral response associated with repeated exposure to more therapeutically relevant stimulant doses and administration patterns: threshold doses of MP (0.5–1.0 mg/kg) or AMPH (0.1– 0.25 mg/kg) were administered i.p. or s.c. twice daily, and then animals were tested in response to 2.5 mg/kg MP or 0.5 mg/kg AMPH. Our results suggest that stimulantinduced effects on NE transmission may play a critical role in the therapeutic actions of MP and AMPH, and, in addition, provide evidence for low-dose stimulant-induced sensitization. 877 878 Kuczenski and Segal Results AMPH Pretreatment/AMPH Challenge. In the initial study, groups of animals received saline or AMPH (0.1 or 0.25 mg/kg) twice daily (10:00 AM and 2:00 PM) for 5 days. Four days after the last treatment, animals were challenged with AMPH (0.5 mg/kg). The pattern of locomotor activity produced by the AMPH challenge is summarized in Fig. 1. This response exhibited a graded increase [ANOVA, F(2,27) ⫽ 3.42, p ⬍ 0.05] as a function of the pretreatment dose, but only the behavior of the higher dose group achieved statistical significance. MP Pretreatment/AMPH Challenge. To determine whether repeated exposure to MP would also result in an altered response to subsequent AMPH challenge (cross-sensitization), groups of animals received twice daily injections of saline or MP (0.5 or 1.0 mg/kg), and 4 days after the last pretreatment were challenged with AMPH (0.5 mg/kg). The locomotor response profiles to the challenge injection are summarized in Fig. 2. As with AMPH pretreatment, there was a graded response [ANOVA, F(2,27) ⫽ 3.48, p ⬍ 0.05] dependent on the pretreatment dose, but only the higher pretreatment dose resulted in a significant cross-sensitization to AMPH. MP Pretreatment/MP Challenge. Because the locomotor response following MP pretreatment was only marginally increased, we sought to determine whether a longer MP pretreatment would result in a more robust increase in locomotion. In this study, animals were pretreated with saline or MP (1.0 mg/kg) twice daily for 11 days, and 4 days later, were challenged with 2.5 mg/kg MP (Fig. 3). The locomotor response was significantly elevated in the MP-pretreated group. Extracellular DA in Nucleus Accumbens and NE in Hippocampus in Response to Threshold Doses of MP and AMPH. Our previous results comparing the extracellular DA and NE responses to MP (Kuczenski and Segal, 1997) were consistent with some data in the literature that MP exhibits a higher affinity for the NE compared with the DA transporter (Ferris et al., 1972; Andersen, 1987). To determine whether a similar relationship could be observed at more clinically relevant threshold doses, the nucleus accum- Fig. 1. Effects of AMPH pretreatment on the temporal pattern of horizontal locomotion in response to an AMPH (0.5 mg/kg) challenge. Groups of animals were administered saline or AMPH (0.1 or 0.25 mg/kg) twice daily for 5 days. Four days after the last pretreatment injection, animals were challenged with AMPH (0.5 mg/kg). Values represent the mean ⫾ S.E.M. Bar graphs represent the cumulated response during the initial 120 min following drug administration. ANOVA revealed a significant effect of pretreatment [F(2,27) ⫽ 3.42; p ⬍ 0.05]. *p ⬍ 0.05 compared with saline pretreated group (t ⫽ 2.54, df ⫽ 27). Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 vinyl acetate tubing connected to a fluid swivel. Dialysate was collected through glass capillary tubing into vials containing 20 l of 25% methanol, 0.2 M sodium citrate, pH 3.8. Under these conditions, dialysate NE, DA, and 5HT and metabolites were stable throughout the collection and analysis interval. Samples were collected outside the experimental chamber to avoid disturbing the animal. Individual probe recoveries were estimated by sampling a standard DA solution in vitro. Preliminary studies indicated that individual probe recoveries for DA and NE were similar. At the end of the experiment, each animal was perfused with formalin for histological verification of probe placements. Dialysate samples were collected every 20 min. Nucleus accumbens samples were assayed for DA, 3,4-dihydroxyphenylacetic acid, homovanillic acid, 3-methoxytyramine, 5-hydroxyindoleacetic acid, and 5HT. In all experiments, solutions of standards revealed a clean separation between 3-methoxytyramine and 5HT. The high pressure liquid chromatography-electrochemical detector consisted of a 100 ⫻ 4.6 mm ODS-C18 3-m column (Regis, Morton Grove, IL) maintained at 40°C. Mobile phase (0.05 M citric acid, 7% methanol, 0.1 mM Na2EDTA, and 0.2 mM octane sulfonate adjusted to pH 4.0 – 4.5) was delivered at 0.6 to 0.8 ml/min by a Waters model 510 pump. In hippocampus samples, NE was separated using a similar mobile phase containing 4% methanol and 1.5 mM octane sulfonate. Amines were detected with a Waters 460 detector with a glassy carbon electrode maintained at ⫹0.65 V relative to a Ag/AgCl reference electrode. Concentrations were estimated from peak heights using a Waters Maxima 820 data station. Substances in the dialysates were corrected for individual probe recoveries to account for this source of variability, and, although the exact relationship between dialysate concentration and actual extracellular transmitter content is not clear, values are presented as dialysate concentration to allow for meaningful comparisons to other data in the literature. Data Analysis. Behavioral and neurochemical data were statistically analyzed using repeated measures ANOVA and t tests with Bonferroni corrections for specific group/time comparisons. Psychostimulant Threshold Doses: Behavior and Neurochemistry 879 Fig. 3. Effects of MP (1.0 mg/kg) pretreatment on the temporal pattern of horizontal locomotion in response to a MP (2.5 mg/kg) challenge. Groups of animals were administered saline or MP twice daily for 11 days. Four days after the last pretreatment injection, animals were challenged with MP (2.5 mg/kg). Values represent the mean ⫾ S.E.M. The bar graph represents the cumulated response during the 90-min interval following drug administration. *p ⬍ 0.05 compared with saline-pretreated group (t ⫽ 2.15, df ⫽ 18). bens DA and hippocampus NE responses were characterized at various MP doses (0.5–2.5 mg/kg), and compared with a low dose of AMPH (0.25 mg/kg). All of these doses are within the therapeutic range, at least on a milligram per kilogram basis. The results are summarized in Figs. 4 and 5. MP produced a dose-dependent increase in extracellular DA, both in peak and AUC, although the lowest dose (0.5 mg/kg) failed to significantly increase extracellular DA concentrations. However, the magnitude of the highest MP-induced DA response was significantly less than for AMPH (Fig. 4). In contrast, in the same animals, all the doses of MP increased extracellular concentrations of NE, and unlike the relative effects of the two drugs on DA, the two highest MP doses increased NE significantly more than did AMPH (Fig. 5). Concomitant evaluation of extracellular 5HT concentrations in nucleus accumbens revealed no significant effects in response to any of the doses tested (data not shown). To determine whether a significant accumbens DA response to 0.5 mg/kg MP would emerge with repeated MP pretreatment, animals received twice daily injections of sa- Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 Fig. 2. Effects of MP pretreatment on the temporal pattern of horizontal locomotion in response to an AMPH (0.5 mg/kg) challenge. Groups of animals were administered saline or MP (0.5 or 1.0 mg/kg) twice daily for 5 days. Four days after the last pretreatment injection, animals were challenged with AMPH (0.5 mg/kg). Values represent the mean ⫾ S.E.M. Bar graphs represent the cumulated response during the indicated interval following drug administration. ANOVA revealed a significant effect of pretreatment [F(2,27) ⫽ 3.48; p ⬍ 0.05]. *p ⬍ 0.05 compared with saline pretreated group (t ⫽ 2.38, df ⫽ 13). 880 Kuczenski and Segal Fig. 5. Left, temporal profile of the hippocampus extracellular NE response to an acute injection of AMPH (0.25 mg/kg) or MP (0.5, 1.0, 2.5 mg/ kg). *p ⬍ 0.05 compared with the sample collected immediately before drug administration. Right, bar graphs represent the peak response and AUC during the 120-min interval following drug administration. Peak response ANOVA: F(3,40) ⫽ 7.83, p ⬍ 0.0001; ⫹⫹ p ⬍ 0.01 compared with response to 0.25 mg/kg AMPH (t ⫽ 2.64, df ⫽ 8.9). AUC ANOVA: F(3,40) ⫽ 7.83, p ⬍ 0.0001; ⫹p ⬍ 0.05, ⫹⫹⫹p ⬍ 0.001 compared with 0.25 mg/kg AMPH; *p ⬍ 0.05 compared with 0.5 mg/kg MP response (all t values ⬎2.36). line or MP (0.5 mg/kg) for 5 days, and, 48 h after the last pretreatment injection, were challenged with MP (0.5 mg/ kg). Repeated MP pretreatment did not alter the hippocampus NE response (Fig. 6, left), nor was a significant nucleus accumbens DA response produced (Fig. 6, right). Discussion The results of these studies indicate that the repeated administration of MP and AMPH at doses near threshold for locomotor activation, and within the therapeutic range for ADHD treatment, at least on a milligram per kilogram basis, can produce sensitization-like effects on the locomotor response to a subsequent stimulant exposure. That we observed an increased locomotor response to stimulant challenge following repeated MP treatment is consistent with some (Gaytan et al., 1997a; Sripada et al., 1998) but not other data in the literature (Crawford et al., 1998; Izenwasser et al., 1999). Although a variety of experimental variables likely account for these divergent observations, at least two characteristics of the treatment protocols may be responsible for this discrepancy. First, an apparent sensitization to MP was observed only in experiments in which the home cage served as the test chamber (present results; Gaytan et al., 1997a; Sripada et al., 1998). This observation suggests that contextdependent conditioning might play an important role in the development/expression of an augmented locomotor response to these low-dose MP treatments. However, in the present study although we observed a brief augmented response to the first saline injection after drug pretreatment, this effect was not apparent in response to the last saline injection Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 Fig. 4. Left, temporal profile of the nucleus accumbens extracellular DA response to an acute injection of AMPH (0.25 mg/kg) or MP (0.5, 1.0, 2.5 mg/kg). Values represent the mean ⫾ S.E.M. Baseline values are the median of the three samples collected immediately before drug administration. *p ⬍ 0.05 compared with the sample collected immediately before drug administration. Right, bar graphs represent the peak response and AUC during the 120-min interval following drug administration. Peak response ANOVA: F(3,36) ⫽ 7.92, p ⬍ 0.001; ⫹p ⬍ 0.05; ⫹⫹⫹p ⬍ 0.001 compared with response to 0.25 mg/kg AMPH (all t values ⬎2.37). AUC ANOVA: F(3,36) ⫽ 13.14, p ⬍ 0.0001; ⫹ p ⬍ 0.05, ⫹⫹⫹p ⬍ 0.001 compared with 0.25 mg/kg AMPH response; *p ⬍ 0.05 compared with 0.5 mg/kg MP response (all t values ⬎2.23). Psychostimulant Threshold Doses: Behavior and Neurochemistry 881 Fig. 6. Left, temporal profile of the hippocampus extracellular NE. Right, nucleus accumbens extracellular DA responses to 0.5 mg/kg MP in groups of animals pretreated with repeated saline or MP (0.5 mg/kg b.i.d.). Values represent the mean ⫾ S.E.M. Baseline values are the median of the three samples collected immediately before drug administration. Inset, bar graph represents the AUC during the initial 60 min following drug administration. There was no significant effect of MP pretreatment (t ⫽ 1.05, df ⫽ 15, p ⬎ 0.3). 1983; Patrick et al., 1984; Cho et al., 1999; Thai et al., 1999) compared with 15 to 30 min following the oral route (Wargin et al., 1983; Patrick et al., 1984); and in ADHD subjects, peak plasma concentrations [as well as therapeutic efficacy (Swanson et al., 1978)] of these drugs are not achieved until 90 to 180 min after oral administration (Wargin et al., 1983). Rate of drug accumulation is an important variable that has been significantly linked to abuse liability (Balster and Schuster, 1973). Furthermore, in rats peak plasma concentrations are 2- to 6-fold higher after intraperitoneal compared with oral administration (Wargin et al., 1983; Patrick et al., 1984). A similar relationship is evident in corresponding behavioral measures (Foltin, 1982). Thus, the doses we used in our studies would likely have produced smaller behavioral and neurochemical responses following oral/intragastric administration. Other important variables that impact on the interpretation of our results include species differences in rate and pattern of drug metabolism, age differences, and time of day at which drug was administered. For example, AMPH exhibits a half-life of 6 to 8 h in humans (Brown et al., 1979), compared with about 60 min in rats (Melega et al., 1995). MP is also more slowly metabolized in humans compared with rats (2.5 versus 1 h, respectively) (Wargin et al., 1983; Srinivas et al., 1992). Species differences in exposure time to these drugs may be very important, especially with respect to repeated, long-term administration. Likewise, evidence suggests that the response of adults may differ from that of younger subjects (Roffman and Raskin, 1997), a potentially important distinction for animal models of ADHD treatment. Furthermore, our injection of drug during the light phase, i.e., the period of normal inactivity/sleep for the rat, may also have significantly influenced the response to these stimulants (Gaytan et al., 1997b, 1999). Thus, caution is appropriate in extrapolating from the conditions used in our studies to human exposure patterns. Although these concerns apply equally to interpretation of our neurochemical data, comparison of the pattern of neurotransmitter responses promoted by the acute administration Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 before challenge (data not shown). Thus, it seems unlikely that context-dependent factors alone can account for the augmented challenge response in our studies. Another variable distinguishing the divergent sets of data is the MP dose. An augmented locomotor response to stimulant challenge was previously reported when both the pretreatment and challenge doses were ⱕ2.5 mg/kg MP (present results; Gaytan et al., 1997a; Sripada et al., 1998), but not when either dose was ⱖ5 mg/kg MP (Gaytan et al., 1997a; Crawford et al., 1998; Izenwasser et al., 1999). One interpretation for this observation is that higher MP doses introduce effects that inhibit and/or obscure increases in the locomotor response to subsequent drug exposure. In this regard, an altered responsivity may be expressed in other behaviors that are not readily detected using automated measures. We have previously observed that significant stereotypy can emerge with repeated administration of stimulant doses that acutely produce predominantly locomotor activation (Segal and Kuczenski, 1987). Clearly, additional studies, including detailed observations of the animals, will be necessary to further elucidate the consequences of repeated low-dose MP. Several important factors, in addition to dose, impact on the potential relevance of the sensitization data to the therapeutic use of stimulants. For one, a variety of pharmacokinetic variables must be considered. Although, on a milligram per kilogram basis, we used doses of MP and AMPH within the therapeutic range, route of administration and species differences in drug metabolism also significantly affect plasma and brain levels of the drug, and correspondingly the qualitative and quantitative features of the behavioral response. In this regard, it is important to note that whereas we injected AMPH and MP s.c. or i.p., as in most animal studies, the clinical use of psychostimulants typically involves oral administration. These differences in route of administration affect both the rate of accumulation of the drug in plasma/brain as well as the peak drug concentrations that are achieved. Thus, for example, in rats, peak stimulant concentrations are achieved within 10 min following intraperitoneal or subcutaneous administration (Wargin et al., 882 Kuczenski and Segal of the drug in plasma/brain and peak drug concentrations that are achieved, both of which play critical roles in the qualitative and quantitative features of the behavioral response. In fact, the interpretation of previous animal studies is limited to the degree that these studies fail to simulate the treatment conditions associated with long-term stimulant use in humans. Therefore, further research incorporating those factors that more closely approximate the therapeutic conditions will be required before more definitive conclusions can be reached regarding the effects of stimulant treatment in children with ADHD. References Andersen PH (1987) Biochemical and pharmacological characterization of [3H]GBR12935 binding in vitro to rat striatal membranes: Labeling of the dopamine uptake carrier. J Neurochem 48:1887–1896. Balster RL and Schuster CR (1973) Fixed-interval schedule of cocaine reinforcement: Effect of dose and infusion duration. J Exp Anal Behav 20:119 –129. Biederman J and Spencer T (1999) Attention-deficit/hyperactivity disorder (ADHD) as a noradrenergic disorder. Biol Psychiatry 46:1234 –1242. Brown GL, Hunt RD, Ebert MH, Bunney WE and Kopin IJ (1979) Plasma levels of d-amphetamine in hyperactive children. Psychopharmacology 62:133–140. Browne RG and Segal DS (1977) Metabolic and experiential factors in the behavioral response to repeated amphetamine. Pharmacol Biochem Behav 6:545–552. Cho AK, Melega WP, Kuczenski R, Segal DS and Schmitz DA (1999) Caudateputamen dopamine and stereotypy response profiles after intravenous and subcutaneous amphetamine. Synapse 31:125–133. Crawford CA, McDougall SA, Meier TL, Collins RL and Watson JB (1998) Repeated methylphenidate treatment induces behavioral sensitization and decreases protein kinase A and dopamine-stimulated adenylyl cyclase activity in the dorsal striatum. Psychopharmacology 136:34 – 43. Ferris RM, Tang FLM and Maxwell RA (1972) A comparison of the capacities of isomers of amphetamine, deoxypipradol and methylphenidate to inhibit the uptake of tritiated catecholamines into rat cerebral cortex slices, synaptosomal preparations of rat cerebral cortex, hypothalamus and striatum and into adrenergic nerves of rabbit aorta. J Pharmacol Exp Ther 181:407– 416. Florin SM, Kuczenski R and Segal DS (1994) Regional extracellular norepinephrine responses to amphetamine and cocaine and effects of clonidine pretreatment. Brain Res 654:53– 62. Foltin RW (1982) Intragastric methylphenidate does have effects on the behavior of rats. Pharmacol Biochem Behav 17:1089 –1090. Gainetdinov RR, Wetsel WC, Jones SR, Levin ED, Jaber M and Caron MG (1999) Role of serotonin in the paradoxical calming effect of psychostimulants on hyperactivity. Science (Wash DC) 283:397– 401. Gatley SJ, Pan DF, Chen RY, Chaturvedi G and Ding YS (1996) Affinities of methylphenidate derivatives for dopamine, norepinephrine and serotonin transporters. Life Sci 58:PL231–PL239. Gaytan O, Al-Rahim S, Swann A and Dafny N (1997a) Sensitization to locomotor effects of methylphenidate in the rat. Life Sci 61:PL101–PL107. Gaytan O, Ghelani D, Martin D, Swann A and Dafny N (1997b) Methylphenidate: Diurnal effects on locomotor and stereotypic behavior in the rat. Brain Res 777: 1–12. Gaytan O, Lewis C, Swann A and Dafny N (1999) Diurnal differences in amphetamine sensitization. Eur J Pharmacol 374:1–9. Izenwasser S, Coy AE, Ladenheim B, Loeloff RJ, Cadet JL and French D (1999) Chronic methylphenidate alters locomotor activity and dopamine transporters differently from cocaine. Eur J Pharmacol 373:187–193. Jacobs BL and Fornal CA (1997) Serotonin and motor activity. Curr Opin Neurobiol 7:820 – 825. Kuczenski R and Segal DS (1989) Concomitant characterization of behavioral and striatal neurotransmitter response to amphetamine using in vivo microdialysis. J Neurosci 9:2051–2065. Kuczenski R and Segal DS (1997) Effects of methylphenidate on extracellular dopamine, serotonin, and norepinephrine: Comparison to amphetamine. J Neurochem 68:2032–2037. McNamara CG, Davidson ES and Schenk S (1993) A comparison of the motoractivating effects of acute and chronic exposure to amphetamine and methylphenidate. Pharmacol Biochem Behav 45:729 –732. Melega WP, Williams AE, Schmitz DA, DiStefano EW and Cho AK (1995) Pharmacokinetic and pharmacodynamic analysis of the actions of D-amphetamine and D-methamphetamine on the dopamine terminal. J Pharmacol Exp Ther 274:90 – 96. Patrick KS, Ellington KR and Breese GR (1984) Distribution of methylphenidate and p-hydroxymethylphenidate in rats. J Pharmacol Exp Ther 231:61– 65. Patrick KS and Markowitz JS (1997) Pharmacology of methylphenidate, amphetamine enantiomers and pemoline in attention-deficit hyperactivity disorder. Hum Psychopharmacol 12:527–546. Pliszka SR, McCracken JT and Maas JW (1996) Catecholamines in attention-deficit hyperactivity disorder: Current perspectives. J Am Acad Child Adolescent Psychiatry 35:264 –272. Robinson TE and Becker JB (1986) Enduring changes in brain and behavior produced by chronic amphetamine administration: A review and evaluation of animal models of amphetamine psychosis. Brain Res Rev 11:157–198. Robinson TE and Berridge KC (1993) The neural basis of drug craving: An incentivesensitization theory of addiction. Brain Res Rev 18:247–291. Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017 of AMPH and MP within the context of the generality of behavioral effects, can provide insight into the relevance of specific neurochemical changes. For example, the doses of AMPH and MP most relevant to therapeutic efficacy, 0.25 mg/kg AMPH and 0.5 mg/kg MP, produced markedly divergent DA responses. These DA effects are consistent with our previous higher dose comparisons between psychostimulants with different mechanisms of interaction, i.e., DA releasers like AMPH typically promote severalfold higher extracellular DA responses than behaviorally similar doses of DA uptake blockers such as MP. In contrast to the divergent DA responses, we observed similar NE effects to the low doses of AMPH (0.25 mg/kg) and MP (0.5 mg/kg). In fact, in contrast to its effect on NE, this dose of MP did not affect accumbens DA even after repeated administration. Although our results do not take into account possible regional differences in neurotransmitter responsivity, they are consistent with a potentially important role for NE in the behavioral effects of low doses of psychostimulants. Within this same context, we did not observe an effect of these doses of AMPH and MP on extracellular 5HT in nucleus accumbens. We have previously shown that moderate doses of AMPH (⬃2 mg/kg) can increase extracellular serotonin levels in a variety of brain regions (Kuczenski and Segal, 1989; Segal and Kuczenski, 1997). In contrast, even chronic administration of high doses of MP (up to 30 mg/kg) failed to affect extracellular 5HT levels (Segal and Kuczenski, 1999), consistent with the relatively low affinity of this stimulant for the 5HT transporter (Gatley et al., 1996). Taken together with the present data, our results suggest that, in contrast to recent speculations (Gainetdinov et al., 1999), a stimulant-induced increase in extracellular 5HT likely does not play a significant role in the therapeutic effects of low doses of these drugs. Finally, the present neurochemical and behavioral results may also provide some insight with regard to mechanisms contributing to low-dose stimulant-induced sensitization. Our data showed that repeated administration of the lowest dose of MP we used (0.5 mg/kg) failed to result in the development of an augmented behavioral response to subsequent stimulant challenge. This treatment also had no effect on extracellular DA in nucleus accumbens, an effect that appears to be important to the development of stimulant abuse. In this regard it is also important to recognize that the oral administration of the doses we used in these studies would be expected to produce significantly lesser effects than we observed following intraperitoneal and subcutaneous administration. Thus, the absence of a significant DA response may have important implications for the abuse liability of lowdose, long-term MP treatment. In summary, the comparative neurochemical profiles in response to MP and AMPH suggest that the NE effects may play an important role in the therapeutic effects of these drugs. In addition, repeated administration of AMPH and MP in the milligram per kilogram therapeutic dose range for treatment of ADHD can result in the development of behavioral sensitization, which is evident in the response to subsequent stimulant challenge. However, even with doses that appear to be relevant to clinical usage, interpretation of our results is limited because of other factors that significantly influence drug exposure effects. In particular, route of administration will significantly affect the rate of accumulation Psychostimulant Threshold Doses: Behavior and Neurochemistry Robinson TE and Whishaw IQ (1988) Normalization of extracellular dopamine in striatum following recovery from a partial unilateral 6-OHDA lesion of the substantia nigra: A microdialysis study in freely moving rats. Brain Res 450:209 –224. Roffman JL and Raskin LA (1997) Stereotyped behavior: Effects of d-amphetamine and methylphenidate in the young rat. Pharmacol Biochem Behav 58:1095–1102. Segal DS (1976) Differential effects of para-chlorophenylalanine on amphetamineinduced locomotion and stereotypy. Brain Res 116:267–276. Segal DS and Kuczenski R (1987) Individual differences in responsiveness to single and repeated amphetamine administration: Behavioral characteristics and neurochemical correlates. J Pharmacol Exp Ther 242:917–926. Segal DS and Kuczenski R (1994) Behavioral pharmacology of amphetamine, in Amphetamine and Its Analogues: Psychopharmacology, Toxicology and Abuse (Cho AK and Segal DS eds) pp 115–150, Academic Press, San Diego, CA. Segal DS and Kuczenski R (1997) Repeated binge exposure to amphetamine and methamphetamine: Behavioral and neurochemical characterization. J Pharmacol Exp Ther 282:561–573. Segal DS and Kuczenski R (1999) Escalating dose-binge treatment with methylphenidate: Role of serotonin in the emergent behavioral profile. J Pharmacol Exp Ther 291:19 –30. Srinivas NR, Hubbard JW, Quinn D and Midha KK (1992) Enantioselective pharmacokinetics and pharmacodynamics of dl-threo-methylphenidate in children with attention deficit hyperactivity disorder. Clin Pharmacol Ther 52:561–568. 883 Sripada S, Gaytan O, Al-Rahim S, Swann A and Dafny N (1998) Dose-related effects of MK-801 on acute and chronic methylphenidate administration. Brain Res 814: 78 – 85. Swanson JM, Kinsbourne M, Roberts W and Zucker K (1978) A time-response analysis of the effect of stimulant medication on the learning ability of children referred for hyperactivity. Pediatrics 61:21–29. Thai DL, Yurasits LN, Rudolph GR and Perel JM (1999) Comparative pharmacokinetics and tissue distribution of the d-enantiomers of para-substituted methylphenidate analogs. Drug Metab Dispos 27:645– 650. Wargin W, Kilts PC, Gualtieri CT, Ellington KR, Mueller RA, Kraemer G and Breese GR (1983) Pharmacokinetics of methylphenidate in man, rat and monkey. J Pharmacol Exp Ther 226:382–386. West CHK, Bonsall RW, Emery MS and Weiss JM (1999) Rats selectively bred for high and low swim-test activity show differential responses to dopaminergic drugs. Psychopharmacology 146:241–251. White FJ and Kalivas PW (1998) Neuroadaptations involved in amphetamine and cocaine addiction. Drug Alcohol Depend 51:141–153. Send reprint requests to: Ronald Kuczenski, Ph.D., Psychiatry Department (0603), University of California San Diego School of Medicine, 9500 Gilman Dr., La Jolla, CA 92093. E-mail: [email protected] Downloaded from jpet.aspetjournals.org at ASPET Journals on May 3, 2017