* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Drugs for RA
Discovery and development of direct Xa inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Pharmacognosy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Psychopharmacology wikipedia , lookup
Discovery and development of direct thrombin inhibitors wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Prescription costs wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Drug interaction wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Discovery and development of cyclooxygenase 2 inhibitors wikipedia , lookup
Discovery and development of integrase inhibitors wikipedia , lookup
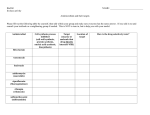
Class of Drugs Penicillin Drug Names - Narrow Spectrum - Antistaphyloccocal - Extended Spectrum Specific For - Narrow Spectrum: Gm (+) Cocci, spirochetes - Antistaphyloccocal: Staph - Extended Spectrum: Gm (-) bacilli Cephalosporin 1st Gen: - Cefazolin: IV - Cephalexin: Oral 2nd Gen - Cefurozime sodium: IV - Cefuroxime axetil: oral 3rd Gen: - Ceftazidime: against P. aeruginosa - Ceftriaxone: against Gonorrhea th 4 Gen: - Cefepime: P. aeruginosa 1st Gen: Gm (+) 4th Gen: Gm (-) Imipenam – cilastatin Ertapenem Doripenem Meropenem Broad Spectrum: Gm (+/-) and anaerobes Carbapenems (DIME) Special Things Adverse Effects Degraded to penicilloic acid which binds to antigens and forms an immune response - Hypersensitivy: urticaria or anaphylactic shock - serum sickness - interstitial nephritis - Non-allergic amoxicillin rash Platelet dysfunction and bleeding w/ cefotetan 5% Cross-sensitivity with penicillin - seizures w/ renal insufficiency - cross-sensitivity w/ pcns - Dose adjustments needed with renal insufficiency Monobactam Aztreonam Vancomycin – Glycopeptide antibiotic Gm (-) aerobes When there are multo-drug resistant strains of: Enterobacter, Citrobacter, Klebsiella, P. aeruginosa (PECK) Gm (+) Cocci and MRSA - hypersensitivity reactions Oral – Don’t use for systemic infections Beginning to experience VRE Concentration Dependent Killing Lipoglycopeptides – Dalbavancin interfere with bacterial Oritavancin Telavancin cell wall synthesis MRSA (DOT) Bacitracin – messes with dephosphorylation; inhibits transfer of peptidoglycan subunits Staph, Strep - Red Man Syndrome: hypotension, erythematous rash on face caused if infused too quickly - Oto and Nephrotoxicity - Fevers, chills, flushing and phlebitis - Dalbavancin – Red man Syndrome - Oritavancin – Itching and flushing - Telavancin – Red man Syndrome & CI for pregnant women (nephrotoxicity) - Nephrotxicity if not used topically Fosfomycin – stops formation of Nacetylmuramic acid -Aminoglycosides (30S) Amikacin Gentamicin Neomycin Streptomycin Tobramycin Tetracycline (30S) (GNATS) Doxycyline Minocycline Tetracycline Tigecycline Gram (+/-), UTI in Women Aerobic Gm (-) bacilli Bacteriocidal Nephro and Ototoxicity Aerobic Gram (+/-), rickettsia, mycoplasma, chlamydia, CA-MRSA Bacteriostatic Gm (+/-) bacteria Bacteriostatic - Bind to divalent cations, so [ ] goes down with milk and yogurt - Discoloration of teeth – avoid in pregnancy and children < 8 - Photosensitization - Esophageal ulcers (so swallow with a full glass of water) - Diarrhea - Cholestatic hepatits - Azithromycin & telithromycin: QT interval prolongation - CYP3A4 inhibitor (except for azithro) - Teli – contraindicated w/ myasthenia gravis (resp. (DOMInaTE TI) Macrolides (50S) Erythromycin Azithromycin Clarithromycin Telithromycin Gm (+) Cocci, Anaerobes, MRSA Gm (+) Cocci, meningococci, H. Influenza Static or cidal depending on [ ] Quinupristin Dalfopristin 30:70 mixture (Syndercid) Gm (+), VRE Static alone Linezolid Tedizolid Gm (+), MRSA VRE Clindamycin (50S) Chloramphenicol (50S) Streptogramins (50S) Oxazolidones (50S) Cidal in combination Static against enterococci & staph Cidal against strept Sulfonamides – inhibit ability to make folic acid Sulfamethoxide Trimethoprim Together: (TMP-SMX) Gm (-), MRSA Static separately Cidal – TMP-SMX failure) - Diarrhea - C. dif. - “Gray baby” syndrome: weakness, resp. depression, hypotension, shock & ashen gray cyanosis - Aplastic anemia - Arthralgia - Myalgia - Diarrhea - Nausea - Linezolid: thrombocytopenia - Serotonin syndrome: severe diarrhea, mental status changes, hyperthermia – common with other drugs that increase serotonin Warfarin: Serious bleeds Phenytoin: - Crystalluria - Kernicterus - Hyperkalemia (increase in potassium) - Hemolytic anemia with G6PD deficiency - Stevens-Johnson Fluoroquinolones – Inhibit 2 bacterial DNA topoisomerases Type II (DNA Gyrase) Type II – Gm (-) Type IV Ciprofloxacin Levofloxacin Moxifloxacin Ofloxacin Norfloxacin Type IV – Gm (+) Concentration dependent killing Cidal against Gm (+/-) Long PAE COLuMN Metronidazole & Tinidazole – creates reactive reduction products (nitroradicals), which has antimicrobial effects Nitrofurantoin – causes DNA damage Anaerobes: bacteroides, C. dif, H. Pylori, E. Histolytica, Giardia, Trichomonas vaginalis GET BitCH E. Coli, E. faecalis, K. Pneumonia, S. Saprophyticus USE WITH UTI’s Syndrome (Skin hypersensitivity) - Tendonitis & rupture - CI in pregnancy & pediatrics – Cartilage damage - hypo/hyperglycemia - phototoxicity - peripheral neuropathy - QT prolongation - Binds with Caffeine (CYP1A2 inhibitor) - Bind to divalent cations, so [ ] goes down with milk and yogurt - Anorexia - Metallic taste – so take w/ food - Disulfarim-like reaction w/ EtOH: nausea, vomiting, sweating, flushing, palpations, dyspnea - Nausea - Diarrhea, - Hemolytic anemia w/ G6PD deficiency - pulmonary fibrosis w/ prolonged use - CI: CrCL < 60ml/min = possible accumulation of toxic metabolites - CrCL < 40 mL/min = ineffective Daptomycin – Inserts a MRSA, VRE, VR S. aureus (VRSA)… lipophilic tail into the bacterial cell membrane messes with cell membrane causes K efflux leads to nucleic acid and protein synthesis arrest cell death 1. Against MRSA a. Inhibit Cell Wall Synthesis: i. Vancomycin ii. Lipoglycopeptides b. 30S inhibitor i. Tetracycline c. 50S inhibitor i. Clindamycin ii. Oxazolidones d. Folic Acid synthesis inhibitor i. Sulfonamides e. Nucleic and amino acid synthesis arrest by lipophilic tail insertion i. Daptomycin myopathy 2. Against VRE a. 50S inhibitor i. Streptogramins ii. Oxizoladones b. Nucleic and amino acid synthesis arrest i. Daptomycin 3. Leave Quin alone to ride his bicycle a. Tetracycline and Fluorquinalones bind to di and tri-valent cations like milk and yogurt 4. Nitro and his furious sulfur causes you to bleed a. Nitrofurantoin and Sulfonamides: Hemolytic anemia with G6PD deficiency 5. When Quin and Mac’s heart races when they do down the slide. a. Macrolides (Azithromycin and Telithromycin) and fluoroquinalones cause QT prolongation 6. Quin likes coffee and Mac likes drugs a. Fluoroquinalones inhibit 1A2 b. Macrolides (except azithromycin) inhibit 3A4 Systemic AntiFungal Drugs Drug Amphotericin B Mode of Action Clinical Uses Binds ergosterol and forms leaky Candida, pores on cell membranes C. neoformans, B. dermatitidis H. capsulatum S. shenkii C. immitis Paracoccidioides braziliensis Aspergillus Penicillium marneffei Mucormyces Adverse Effects Systemic AntiFungal Drugs Flucytosine Systemic AntiFungal Drugs Azoles – Imidazoles Ketoconazole Miconazole Clotrimazole Systemic AntiFungal Drugs MiCKey Azoles – Triazoles Itraconazole Fluconazole Voriconazole FIVe Forms the active metabolite 5fluorodeoxyuridine monophosphate (inhibits DNA synthesis) & Forms fluorouridine triphosphate (inhibits RNA synthesis) Inhibit fungal cytochrome p450 and reduce ergosterol synthesis - C. neoformans - Some Candida - Some dermatiaceous molds that cause chromoblastomycosis Inhibit fungal cytochrome p450 and reduce ergosterol synthesis Fluconazole: - Used to treat mucocutaneous candidiasis More selective for fungal p450 than imidazoles Fluconazole: - Water soluble and good body fluid distribution (CSF) - High bioavailability and has least effects - Best cytotoxicity to fungals Voriconazole: - Good absorption, high Intestinal flora converts drug to fluorouracil (an anti-neoplastic drug) gives: - bone marrow toxicity - anemia - leukopenia - thrombocytopenia Systemic Anti-Fungal Drugs Echinocandins Caspofungin Micafungin Anidulafungin MAC is a fun-gi-n bioavailability and less plasma protein binding than Itraconazole - Oral and I.V. forms available - Undergoes hepatic metabolism, less human P450 induction Destroys fungal cell wall by inhibiting Beta-glycan synthesis Caspofungin: - mucocutaneous candida infections - antifungal during febrile neutropenia - For aspergillosis as a back up when amphotericin B fails. Micafungin: - mucocutaneous candidiasis - Prophylaxis of candida in bone marrow transplant Anidulafungin: - esophageal candidiasis - invasive candidiasis septicemia Oral Drug for Mucocutaneous Infection Griseofulvin Binds to microtubules and disrupts mitosis. Systemic treatment of dermatophytosis ONLY USE TOPICALL It also binds to keratin in the skin and protects form new fungal infections Oral Drug for Mucocutaneous Infection Terbinafine Viral Nucleic acid Synthesis inhibitor - They are nucleosides that are phosphorylated to their nucleotide analog and then act as a substrate for viral enzyme Interferes with ergosterol biosynthesis (like azoles) Dermatophytes – especially Onchomycosis No action on P-450 Inhibits fungal squalene epoxidase accumulation of sterol squalene which is toxic to fungi Drug Mechanism of Action Acyclovir (AntiPhosphorylated by viral herpetic) thymidine kinase (TK) – this increases it’s selectivity Clinical Uses HSV EBV VZV Adverse Effects Resistance to acyclovir can develop in HSV or VZV due to alteration in either viral TK or viral polymerase Viral Nucleic acid Synthesis inhibitor Famciclovir (Antiherpetic) Undergoes first-pass metabolism to penciclovir (PCV) after oral administration – happens in intestinal wall and liver For management of acute herpes zoster For suppression of recurrent genital herpes Reaches maximum serum levels in less than an hour if taken while fasting Viral Nucleic acid Synthesis inhibitor Ganciclovir (AntiCMV) Guanine Viral Nucleic acid Synthesis inhibitor Cytosine Cidofovir (Anti-CMV) MOA similar to Acyclovir Guanosine analog that’s Inhibits DNA phosphorylated by virus polymerase of CMV protein kinase UL97 and then by cellular kinases Cytosine analog that’s Broad Spectrum in activated by intracellular vitro activity of: enzymes to form an - CMV inhibitor of DNA - HSV-1 polymerases - HSV-3 - VZV 1000-fold more effective - EBV against DNA - HHV-6 polymerases of viruses - Adenovirus instead of DNA - HPV polymerases of host cell - Approved for treatment of CMV retinitis in AIDS patients Viral Nucleic acid Synthesis inhibitor Foscarnet (AntiCMV) Inorganic pyrophosphate compound Inhibits viral DNA polymerase, RNA polymerase, HIV RT, and DOES NOT require activation of phosphorylation Topical for mucocutaneous herpes infections HSV VZV CMV EBV HHV-6 HBV HIV Parathyroid and Osteoporosis Type Osteoporosis Drug Teriparatide MOA PTH analog Clinical Use -Increase bone mass in men with primary or hypogonadal osteoporosis - Use for postmenopausal osteoporosis AE Oral Phosphate Binder Oral Phosphate Binder Vitamin D Analogue Calcimimetic Calcium carbonate Calcium acetate Sevelamer Calcitriol Paricalcitol Cincalcet Bisphosphonates Pamidronate Alendronate Drugs for Risedronate osteoporosis Ibandronate & Zolendronate Paget Disease Etidronate Binds to dietary phosphates and inhibits their absorption A non-absorbable cationic ion exchange resin that binds intestinal phosphates Calcitriol – D3 analogue Paricalcitol – D2 analogue Binds to the transmembrane portion of the calcium-sensing receptor in the parathyroid and increases sensitivity to calcium So, the parathyroid thinks it’s seeing more calcium than is really present, and then it won’t release PTH Substitute for pyrophosphate Hyperphosphatemia in chronic kidney disease - also 2ndary hyperparathyroidism Hyperphosphatemia in chronic kidney disease - also 2ndary hyperparathyroidism Low vitamin-D due to 2ndary hyperparathyroidism Don’t use Calcitriol until hyperphosphatemia is controlled – because it will increase calcium, but it will just bind to the excess phosphates 2ndary hyperparathyroidism Hypercalcemia associated with parathyroid carcinoma USED FOR OSTEOPOROSIS Induce apoptosis of osteoclasts Results: - Increases BMD - Decreases vertebral fractures Alendronate & Risedronate – prevent treatment of Poor GI absorption Long half-lives CI: Pregnancy Esophageal ulcers Esophageal stricture Dyspepsia Dysphagia Acid regurgitation postmenopausal and glucocorticoid-induced osteoporosis Ibandronate – treatment and prevention of postmenopausal osteoporosis - Can be used prophylactically Drug for Paget Disease Drug for Osteoporosis Calcitonin Estrogen - Raloxifene Physiologic antagonist of PTH Inhibits osteoclast action Increases BMD and decreases vertebral fracture - Stabilizes bone remodeling - Increases GI calcium absorption - Promotes Calcitonin synthesis - Increases the # of Vit. D receptors on osteoblasts - Increases BMD and decreases fractures - Increases HDL and triglycerides Abdominal pain Nausea Diarrhea MSK Pain Osteomalacia with long-term use of etidronate For Paget Disease Can use for osteoporosis in women who are at > 5 years postmenopausal Administration: SC or IM of 50-100 Used to treat osteoporosis in post-menopausal women Raloxifene – DOES NOT stimulate endometrium, so decreased risk of endometrial cancer Increased risk of breast cancer and endometrial cancer - Weight gain, fluid retention - Vaginal bleeding and spotting - Increased risk of thrombosis Breast enlargement and tenderness NSAIDS Type Acetylsalicylic Acid Drug Aspirin - Non-Selective, Irreversible COX Inhibitor MOA Anti-inflammatory – Decreases prostaglandins Analgesic – decreases PGE2 Antipyretic – decreases PGE2 Blood thinner (anti-platelet) Clinical Use 60-80 mg/d - Antithrombotic effect (Prophylaxis for MI & stroke) AE 3-4 g – Salicylism – tinnitus, hearing loss, dizziness, confusion, headache CI: Children with a viral infection = Reye’s Syndrome – hepatitis & cerebral edema which is fatal Zero-order kinetics @ high doses - Propionic Acid Derivatives Non-selective, reversible COX Ibuprofen** Naproxen** Ketoprofen Flurbiprofen Oxaprozin Use for pain/inflammation caused by: - Trauma - Infection GI – Epigastric distress, ulceration, hemorrhage (Due to decreased prostaglandins) Platelets – inhibits COX-1 inhibits TxA2 results in decreased platelet aggregation Kidneys – Inhibits COX decreases PGE2 & PGI2 which inhibits renal function, thus increasing salt/water retention GI disturbances, peptic ulcers, liver/kidney injury inhibitor Acetic Acid Derivatives Non-selective, reversible COX inhibitor Oxicam Derivatives Selective COX-2 Inhibitor Ketones Selective COX-2 Inhibitor - Autoimmunity - Neoplasms - Joint degeneration - arthritis Use for severe acute inflammatory conditions Indomethacin** Sulindac Etodolac Diclofenac Ketorolac** Piroxicam Meloxicam**a Indomethacin – one of the most potent inhibitors of COX - Strong GI and CNS AE’s Treatment for patients with patent ductus arteriosus in infants Meloxicam - Highest selectivity for COX-2 Lower GI risk Piroxicam – long half-life – so just need a single daily dose Nabumetone Celecoxib Anti-inflammatory Antipyretic Analgesic - No anti-platelet action – so chance of GI bleeding is only 20% - RA OA Acute pain in adults Dysmenorrhea - Renal effects **Cardiovascular risk** - PGI2 provides cardiovascular protection. Prolonged decrease in PGI2 produces these adverse cardiovascular effects DI: CYP2C9 inhibition, so you don’t metabolize fluconazole (A trizole) and fluvastatin GENERAL NSAIDS Gastroprotective Drugs to take with NSAIDs Gastroprotective Drugs to take with NSAIDs 1. Use COX-1 over COX-2 when trying to avoid cardiovascular risk 2. Consider Tylenol for pain first 3. Try Naproxen first since it has the lowest cardiovascular risk 4. If taking aspirin in combination with other NSAIDs, take first so it can do it’s blood thinning effect Misoprostol - reduces risk of gastric problems by 40% Proton pump inhibitors - decreases risk of NSAID-related bleeding (NNT-11) Fever Mild/moderate pain from: - Headache - Sports injury - Dysmenorrhea - OA - RA - Bone Cancer 1. GI bleed risk with all NSAIDs increases 4x 2. Major Risk Factors - males, history of peptic ulcers, dyspepsia, CV disease, age > 60 3. Risk increases when taking NSAIDs with aspirin, corticosteroids, or anticoagulants like warfarin 4. NSAIDS decrease risk of diuretics 5. NSAIDs decrease elimination of lithium and methotrexate = toxicity 6. Taking with warfarin = bleeding a lot - Diarrhea and cramping Topical NSAID Diclofenac Local inhibition of COX-2 Use when first-line agents fail Pruritus, burning, pain, rash ACETAMINOPHEN Type Drug Acetaminophen MOA Inhibits prostaglandin synthesis in the CNS by blocking central COX Clinical Use Fever, pain from OA F = 60-98% Biotransformation via conjugation w/ sulfate or glucuronide – Nhydroxylation via a CYP So NSAIDs block COX after it’s been made Acetaminophen blocks the production of COX altogether Metabolites are renally excreted AE Hepatotoxicity - Don’t take more than 4 g/day - Chronic use - Taking with EtOH - Taking with Isoniazid DI - Increases action of warfarin - Izoniazid = heptatotoxicity Topical Analgesic Type created from hot peppers Drug Capsaicin MOA Depletes substance P from nociceptor nerve fibers Clinical Use MSK pain AE Burning, stinging, erythema WASH HANDS AFTER USE Glucocorticoids Type Endogenous Glucocorticoids Drug Cortisol Corticosterone Cortisone MOA Asthma – inflammatory response is mediated by thromboxanes, prostaglandins, and leukotrienes --> increased platelet aggregation, vascular permeability, and vasoconstriction - GC’s block this process Clinical Use - Addison’s - RA, Asthma - Depress Immune response – for cancer or transplantation AE Long-term GC’s inhibit ACTH from pituitary – so taper drug as removing to avoid adrenal insufficiency - Iatrogenic Cushing’s syndrome caused by prolonged use of synthetic glucocorticoids - Osteoporosis occurs due to GCs inhibiting vitamin-D mediated calcium absorption so that secondary hyperparathyroidism develops. GCs also inhibit osteoblast function. - Impaired wound healing Peptic ulcers, psycosis (with large doses), salt retention and its complications(cortisone, hydrocortisone) Multiple disorders for energy storage and possible development of type II diabetes mellitus; als redistribution of fat from periphery to trunk Protein break down free aa. glucogenesis. This results in weight gain, visceral fat deposit, myopathy and muscle waisting Adrenal suppression may occur if glucocorticoids are administered for more than two weeks Exogenous Glucocorticoids Fludrocortisone Dexamethasone Betamethasone Glucocorticoid Hydrocortisone Dexamethasone – Binds to glucocorticoid receptors in the anterior pituitary which supplies a negative feedback mechanism to lower the release of ACTH. - Adrenoinsu ffiiciency: Addison’s Acute Adrenoinsu ffiiciency Addison’s Supplement with an aldosterone analogue to account for salt loss – Like fludrocortisone Acute – large does initially, then taper does down before adding an aldosterone analogue Glucocorticoid Inhibitors Mineralocorticoid Mitotane Metyrapone Ketoconazole Mifepristone (RU-586) Fludrocortisone Deoxycorticosterone Aldosterone Top 3 = Enzyme inhibitors Mifepristone – Blocks GC intracellular receptor Aldosterone – Excessive Aldosterone causes hypokalemia, metabolic alkalosis, and increase plasma Fludrocortisone – Most common salt-retaining hormone prescribed – It has glucocorticoid and mineralocorticoid activity. - Undergoes first-pass metabolism much slower than aldosterone does. - Be sure to monitor blood pressure and serum potassium Deoxycorticosterone – endogenous precursor of aldosterone – controlled only by ACTH (unline aldosterone) Mineralocorticoid Spironolactone Aldosterone – mineralcorticoid – regulated by ACTH and renin-angiotensin pathways Activation of aldosterone receptor cause increase expression of the Na+/K+ ATPase and the epithelial sodium channel (ENaC) Mineralocorticoid receptor Aldosteronism antagonist Inhibits androgen and volume - hypertension progesterone receptors so that it can cause gynecomastia in men Mineralocorticoid Eplerenome More selective mineralocorticoid receptor antagonist Heart failure Be sure to monitor blood potassium levels Treating Gout and Osteoarthritis Type/Purpose Osteoarthritis Drug Acetaminophen MOA Inhibits prostaglandin synthesis in the CNS by blocking central COX Clinical Use Knee and hip OA AE / Dosing regimen 2.6 – 4 g/day = Ibuprofen 1.2 – 2.4 g/day = naproxen 0.75 g/day Take Acetaminophen every 6-8 hours Osteoarthritis Topical Analgesic Osteoarthritis Topical NSAIDs Osteoarthritis Capsaicin - Depletes substance P from nociceptor nerve fibers Hand OA Burning, stinging, erythema Diclofenac Local inhibition of COX-2 Knee OA if Acetaminophen fails Pruritus, burning, pain, rash Glucosamine Chondroitin Stimulate proteoglycan synthesis from cartilage Ameliorative effect in patients with OA of the knee, but NIH couldn’t prove that Gas, bloating, cramps WASH HANDS AFTER USE DI: Increases bleeding when taken Osteoarthritis Osteoarthritis Corticosteroid Injection Hyaluronic Acid Synovial Fluid constituent Reconstitutes synovial fluid & decreases symptoms Knee/Hip pain relief (4-8 weeks) Decrease OA Evidence of this is poopy with warfarin Osteonecrosis, tendon rupture, skin atrophy Acute joint swelling Effusion Stiffness Rash Ecchymoses Pruritus ALSO VERY EXPENSIVE Acute Gout Acute Gout Acute Gout NSAIDs Indomethacin Corticosteroids – equivalent to NSAIDs Prednisone Colchecine Use when NSAIDs are contraindicated (like renal insufficicency) Antimitotic agent – disrupts microtubules and inhibits leukocyte migration and phagocytosis Pharmacokinetics – Rapidly absorbed Partly metabolized in the liver Excreted via bile and urine Prednisone PO 30-60 mg 3-5 days – taper over 10-14 days in 5 mg increments Avoid with renal insufficiency Has the lowest benefit to toxicity ratio - Diarrhea - Bone marrow suppression – agranulocytosis & aplastic anemia w/ long-term or high dose use DI – P-glycoproteins and CYP3A4 inhibitors – they decrease biliary excretion of colchecine Prophylaxis of Gout Allopurinol Lowers serum urate levels in a dose-dependent manner Works for overproducers and underexcreters Xanthine Oxidase Inhibitors - Skin rash - Leukopenia - Headache - Hypersensitivity Syndrome – severe rash, hepatitis, interstitial nephritis, and eosinophilia - Reduce dose for renal insufficiency - Start with low does and titrate up DI – metabolized to oxypurinol in the liver Inhibits metabolism of warfarin Prophylaxis of Gout Febuxostat - Xanthine Oxidase Inhibitor - Nausea Arthralgias Increases risk of thromboembolism EXPENSIVE No dose reduction for ClCr > 30 mL/min DI – metabolized in inactive metabolites Prophylaxis of Gout Uricosuric Agents Probenecid Increase uric acid excretion Only works for underexcreters CI – azathioprine and mercaptopurine GI irritation Rash Aplastic anemia CI – CrCl < 50 mL/min DI – prolongs duration of many medications, so you can use with penicillin to prolong effects Gout Gout Gout Fenofribate Losartan Pegloticase Increase clearance of ypoxanthine and xanthine Management of hypertriglyceride Decreases serum urate by 20-30% Angiotensin receptor-II antagonist for HTN and HF Hypertension and heart failure Inhibits tubular reabsorption of uric acid & increases urinary excretion IV recombinant uricase – Chronic gout in adults catalyzes the oxidation of uric acid to allantoin, thereby Used as a uric acid “debulker” lowerin serum uric acid Anaphylaxis and infusion reactions – so premedicate with antihistamines and corticosteroids Gout flares CI – G6PD deficiency – run the risk of hemolysis and methmoglobinemia Drugs for RA Type Drug RA drug – most Methotrexate famous because it has the greatest positive to negative side effect ratio RA Drug Luflunomide Immunosuppressant drug (Also anticancer) Abatacept Non-TNF-directed mab MOA Low doses – Inhibits AICAR transofrmylase and thymidylate synthetase – thus it inhibits immune cell proliferation and stimulates apoptosis - Inhibits proinflammatory cytokines Active metabolite – A77-1726 – inhibits dihydroorotate dehydrogenase arrests cells in G1 phase and inhibits cell proliferation and B cell antibodies Binds to CD80/86 on APC Clinical Use -RA - Juvenile chronic arthritis - psoriasis - Ankylosing spondylitis - polymyositis - Systemic lupus - erythematous Vasculitis AE Always give a large 100 mg Loading dose for 3 days then drop to 20 mg/day after that - IV Diarrhea (25%) Elevated liver enzymes (ALT and AST) Weight gain Increased blood pressure Immunosuppressant drug (Also anticancer) Rituximab Targets CD20 on B lymphocytes Use with Methotrexate Non-TNF-directed mab Immunosuppressant drug (Also anticancer) Non-TNF-directed mab TNF-Directed TNF-Directed TNF-directed RA that is refractory to antiTNF agents Alefacept LFA-3 which binds to CD2 on T-Cells Adalimumab Complexes with TNF-a itself, preventing macrophage activation and interrupting T-cell function Infliximab Etanercept Decreases the rate of formation of new lesions Complex with TNF-a Complexes with TNF-a Give in 2 IV infusions 2 weeks apart Plaque psoriasis RA AS Psoriatic arthritis Works like Adalimumab Use for Crohn’s Disease Works better combined with methotrexate Juvenile chronic arthritis Psoriasis Reduces T cells in plaques – so monitor T cell levels. STOP if CD24 drops below 250 cells/microliter Apremilast Glucocorticoids Selective phosphodiesterase Type 4 inhibitor (PDE4) It’s expressed in immune cells and it’s involved in breaking down cAMP Resolve RA promptly and dramatically Inhibit phospholipase A2 so no arachidonic acid Inhibits COX2 Suicidal ideation and behavior found in psoriatic arthritis Prednisone – Don’t exceed 7.5 mg/day Insomnia Hypomania Peptic ulcers Adrenal suppression with longterm use