* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download reconstructive - Shifa International Hospitals
Survey
Document related concepts
Transcript
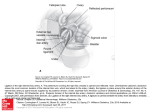
RECONSTRUCTIVE The Iliacus Muscle Flap: An Anatomical and Clinical Evaluation Daniel A. Medalie, M.D. Ramon Llull, M.D., Ph.D. Frederick Heckler, M.D. Cleveland, Ohio; Palma de Mallorca, Spain; and Pittsburgh, Pa. Background: The iliacus muscle is proposed as a new solution for coverage of small to medium defects where either a bulky flap or conspicuous donor sites are undesirable. Methods: Dissection and Microfil studies were performed on fresh cadavers to define the gross and microvascular anatomy of the muscle. Live evaluation of the muscle was performed in combination with multiple iliac crest free tissue transfer procedures. The muscle was then used as a free flap in four separate cases to cover difficult extremity wounds. It was used as a pedicled flap in conjunction with a free iliac crest in a fifth case to assist with a composite mandible and facial defect. Results: The iliacus originates from the inner aspect of the iliac crest and then fuses with the psoas at the level of the inguinal ligament. Its primary blood supply derives from a large branch off of the deep circumflex iliac artery. The isolated muscle resulted in a pancake-like flap measuring approximately 8 ⫻ 8 cm with a 6- to 8-cm pedicle (deep circumflex iliac artery). The muscle was then used clinically both as isolated free flaps and as a pedicled flap in conjunction with a free iliac crest. All flaps survived, resulting in healed wounds without complication. Conclusions: These results demonstrate that the iliacus is a new muscle that should be added to the microsurgeon’s choices for free tissue transfer. It is easily harvested, has a large and well-defined pedicle, and is less prone to donor-site complications than some other muscles typically used for free tissue transfer. (Plast. Reconstr. Surg. 127: 1553, 2011.) M icrosurgical transfer of muscle is now a routine procedure for the coverage of difficult wounds. Large wounds can be easily covered by the latissimus or rectus abdominis.1 Sometimes, however, smaller wounds still require free tissue transfer. The foot and ankle and the dorsum of the hand are places where free flaps might be desired for coverage of exposed bone and tendons. Intraoral defects with exposed bone are also candidates for free tissue transfer. Typically, fasciocutaneous flaps such as the radial forearm have been used in these instances because From Case Western Reserve Medical School and MetroHealth Medical Center; Stem Center, Clinica Palmaplanas; and Allegheny General Hospital. Received for publication September 3, 2010; revised October 26, 2010. Poster presented at the Annual Meeting of the Plastic Surgery Research Council, in Pittsburgh, Pennsylvania, May 21 through 25, 1999, and oral presentations given at the Pennsylvania Ivy Society, 1999, and the Spanish Society of Plastic Surgery, 2001. Copyright ©2011 by the American Society of Plastic Surgeons DOI: 10.1097/PRS.0b013e318208d30e they are less bulky.2 Unfortunately, they leave a rather conspicuous and sometimes debilitating donor site. The gracilis muscle is a smaller muscle with a more hidden donor site but tends to be long and narrow, with a finer pedicle.3 Temporoparietal fascia is an ideal flap for dorsal hand or distal ankle and foot coverage but is difficult to dissect and frequently has small venae comitantes.4 The purpose of this study is to propose the iliacus muscle as a new flap for microsurgical transfer that can cover small to medium defects where either a bulky flap or a conspicuous donor site is undesirable. The flap is based on a previously undescribed but consistent branch off of the deep circumflex iliac artery that we have named the “iliacus branch.” This vessel is distal and posterior to the well-described ascending branch that feeds the internal oblique muscle.5,6 In our clinical studies, the flap has proved to be reliable to date. Disclosure: The authors have no financial interest to declare in relation to the content of this article. www.PRSJournal.com 1553 Plastic and Reconstructive Surgery • April 2011 MATERIALS AND METHODS RESULTS Sixteen iliacus muscles were dissected in eight fresh cadavers. Careful inspection of each muscle was performed to determine its anatomy and feeding blood vessels, and in eight of the dissections, 20 cc of Microfil (Flow Tech, Inc., Carver, Mass.) was injected into the deep circumflex iliac artery at its origin from the external iliac artery before the muscle dissection. The muscles were then removed and radiographed to define their microvascular anatomy. All muscles demonstrated excellent staining by the Microfil technique. Further anatomical analysis was performed in conjunction with 12 clinical procedures. Eight of these procedures were free flap procedures using iliac crest with and without muscle for various reconstructions. The other four were free flap procedures specifically using the iliacus muscle for reconstruction of complex wounds. At these operations, the iliacus muscle was identified and evaluated for blood supply and dimensions. A 25-gauge needle was inserted perpendicular to the muscle down to iliac crest, and the thickness of the muscle at resting length at different locations was determined by measuring the penetration of the needle. Anatomical Observations The iliacus is a flat muscle originating from the inner aspect of the iliac crest and then fusing with the psoas at the level of the inguinal ligament to form a conjoined muscle (Fig. 1). Its primary blood supply in seven of eight cadavers studied (14 dissections) derived from a large branch off of the deep circumflex iliac artery within 2 cm of the deep circumflex iliac artery crossing posterior to the anterior superior iliac spine. We have named this the iliacus branch (Figs. 2 and 3). This is not to be confused with the ascending branch of the deep circumflex iliac artery, which supplies the internal oblique muscle and usually takes off several centimeters proximal to the iliacus branch.5,6 A smaller blood supply, “the psoas branch,” was consistently observed coming from the external iliac artery, passing deep to the psoas and entering the iliacus muscle’s deep posterior aspect (Fig. 3). In one cadaver on both sides, multiple small branches were observed off of the deep circumflex iliac artery feeding into the iliacus distal to the anterior superior iliac spine. In several other ca- Fig. 1. The iliacus is a flat muscle originating from the inner aspect of the iliac crest and then fusing with the psoas at the level of the inguinal ligament (IL) to form a conjoined muscle. Its primary blood supply is the iliacus branch (IB) derived from a large branch off of the deep circumflex iliac artery (DCIA) and vein (DCIV) within 2 cm of the deep circumflex iliac artery crossing posterior to the anterior superior iliac spine (ASIS). The iliacus branch is a separate branch from the previously described ascending branch (AB) to the internal oblique muscle. Typically, the deep circumflex iliac branches originate from the external iliac vessels just superior to the inguinal ligament as they transition to the common femoral artery (CFA) and vein (CFV). The vessels travel over the femoral nerve (FN). 1554 Volume 127, Number 4 • Iliacus Muscle Flap The average size of muscle that could be harvested was 8 ⫻ 8 cm, and the thickness of the muscle ranged from 7 to 13 mm just adjacent to the deep circumflex iliac artery and 10 to 17 mm at the deeper portions of the muscle adjacent to the psoas. The nerve supply to the muscle was found to derive consistently from the femoral nerve as it traveled in the groove between the psoas and the iliacus. Fig. 2. The iliacus muscle is approximately 8 ⫻ 8 cm and is supplied by the deep circumflex iliac artery and veins (DCIA-V). Its main blood supply is the iliacus branch. Fig. 3. Radiograph of a cadaver iliacus muscle injected with Microfil to demonstrate the deep circumflex iliac vessels (DCIA-V) and iliacus branch. It is seen to anastomose with a deeper vessel originating from the external iliac vessels deep to the psoas (psoas branch). davers and in clinical subjects, occasional smaller branches off of the deep circumflex iliac artery distal to the iliacus branch were also observed. We believe that this places the muscle in the type II variant of the Mathes and Nahai classification of muscular vascular anatomy, namely, one dominant pedicle with several lesser pedicles.7 Variations with the anatomy of the deep circumflex iliac artery and venae comitantes were consistent with previously described anatomical studies.8 –10 The average pedicle length for the iliacus was 6 to 8 cm. Surgical Technique The patient is placed supine with a slight bump under the buttock of the side to be dissected. The incision is planned approximately 2 cm above and parallel to the inguinal ligament and iliac crest. The initial dissection is designed to identify the deep circumflex iliac artery at its takeoff from the external iliac vessels. Once the vessel is identified proximally, it is traced distally toward the anterior superior iliac spine. The ascending branch to the internal oblique muscle is identified and ligated. The external oblique, internal oblique, and transversus abdominis are incised just superior to the iliac crest until the iliac crest is identified. On the inner aspect of the crest is the iliacus muscle covered by thin iliacus fascia. The deep circumflex iliac artery penetrates the fascia and travels superficial to the iliacus muscle. The muscle with its investing fascia can be bluntly freed from the preperitoneal fat on top of it until it is easily visible along with the psoas in the deep portion of the wound. The femoral nerve lies in the groove between the psoas and the iliacus, and the lateral femoral cutaneous nerve travels anterior to the iliacus, heading toward the anterior superior iliac spine. It can travel under or over the deep circumflex iliac artery in the region of the anterior superior iliac spine and can be inadvertently transected unless it is identified. The iliacus fascia is incised parallel to the deep circumflex iliac artery and reflected off of the muscle in a bloodless dissection. This exposes the entirety of the iliacus muscle and enables the surgeon to visualize the deep circumflex iliac artery, the iliacus branch, and any other vessels running to the iliacus, including the deep psoas branch. The periosteum of the inner aspect of the iliac crest is then incised and the muscle is elevated off of the crest in a subperiosteal plane. This is also a rapid and bloodless dissection. The dimensions of the muscle to be harvested are decided and the distal end of the deep circumflex iliac artery is clipped, as is the deep psoas branch. A scalpel (or Bovie) is then used to incise the distal and deep portions of the muscle, freeing it from the iliac crest and from its caudal attachments 1555 Plastic and Reconstructive Surgery • April 2011 to the psoas. This aspect of the dissection is somewhat bloody but can be performed in under 5 minutes, thus limiting overall blood loss. The isolated muscle is then allowed to perfuse for 20 minutes before division of the pedicle. For a more detailed description of the anatomy of the deep circumflex iliac artery, the venae comitantes, and the iliac crest region, the reader is referred to Ramasastry et al.,5 Taylor et al.,9 and Strauch et al.10 The muscle can be harvested in conjunction with the iliac crest and overlying skin to create a composite osteomusculocutaneous flap in a fashion very similar to the composite flap using the internal oblique muscle.5,11,12 In this case, the muscle can be taken with the iliac crest and allowed to remain attached to the bone to provide an extra muscular cuff for coverage of adjacent defects in the recipient site. Such uses for this would be in mandible reconstruction with an adjacent floor- of-mouth defect. The muscle can also be incised below the level of the deep circumflex iliac artery and isolated as an island on the iliacus branch, giving it a greater arc of rotation when transferred as part of a composite flap. Closure of the isolated muscle flap defect is quite simple and poses minimal risk for subsequent hernia formation. The transversus abdominis, internal oblique, and external oblique are sewn back to the muscular and periosteal cuff of the iliac crest and the inguinal incision is repaired in a layered fashion. Because there is no loss or denervation of muscle of the anterior abdominal wall, there is no greater risk of hernia than with any other groin incision. CASE REPORTS Case 1 A 19-year-old man sustained an accidental shotgun wound to the right foot. After several débridements, he had exposed Fig. 4. Case 1. (Above, left)A shotgun wound to the right foot, with exposed, damaged navicular and cuneiform-navicular joint space and an 8 ⫻ 5-cm soft-tissue defect. (Above, right) The patient’s right iliacus muscle was harvested in approximately 11⁄2 hours and allowed to perfuse on its pedicle. (Below, left) It was then anastomosed to his dorsalis pedis vessels successfully and covered by a split-thickness skin graft. (Below, right) Four months later, he demonstrated a completely healed wound with no contour abnormality. 1556 Volume 127, Number 4 • Iliacus Muscle Flap damaged navicular and cuneiform-navicular joint space and an 8 ⫻ 5-cm soft-tissue defect (Fig. 4). It was felt that a free flap would be the best reconstructive option for him, and he consented to iliacus muscle transfer to the foot. The muscle was harvested in 1½ hours without complication and anastomosed to his dorsalis pedis vessels successfully. It was then covered by a split-thickness skin graft. Four months later, he demonstrated a completely healed wound with no contour abnormality. He also demonstrated normal ambulation. His donor site healed uneventfully and the scar was completely hidden by his underwear. Case 2 A 40-year-old man sustained a distal tibia fracture secondary to a tractor injury. The wound broke down and the patient was referred to plastic surgery for soft-tissue coverage (Fig. 5). An 8 ⫻ 6-cm iliacus muscle flap was designed and then transferred microsurgically to the patient’s ankle wound. The deep circumflex iliac artery was anastomosed end-to-side to the posterior tibial artery. A meshed skin graft was applied to the flap. Three months later, the patient was walking and demonstrated a well-healed wound with only a mild contour deformity. Case 3 A 19-year-old woman sustained a soft-tissue traumatic injury with exposed patella and patellar tendon (Fig. 6). A 6 ⫻ 6-cm iliacus muscle flap was harvested and then transferred microsurgically to the patient’s lower knee wound with a meshed skin graft. The deep circumflex iliac artery was sewn in end-to-side fashion to the anterior tibial vessel. One year later, the patient was completely active and demonstrated a well-healed wound with minimal contour deformity. Case 4 A 59-year-old woman was diagnosed with an invasive parotid tumor adjacent to the body of her right mandible. After resection was complete, she had a 6-cm bone defect and an accompanying loss of parotid and overlying skin (Fig. 7). It was decided to use a free iliac crest to reconstruct the bone defect and then use an accompanying pedicled iliacus muscle and skin graft to reconstruct the soft-tissue defect. During the operation, the deep circumflex iliac artery was traced to the iliac crest and then identified along with the iliacus branch on the surface of the iliacus muscle. The planned limit of bone resection was marked and the distal pedicle was then ligated. The iliacus was then incised laterally and deeply and raised in a subperiosteal plane from deep to superficial, stopping just beneath the deep circumflex iliac artery as it traveled over the muscle along the inner lip of the iliac crest. The bone cuts were completed and the bone and muscle were completely isolated on the pedicle. Fig. 5. Case 2. (Above, left) A distal tibia fracture with soft-tissue necrosis. An iliacus muscle was harvested from his right side. (Above, right) Shown is the deep circumflex iliac artery and vein (white arrows), the lateral femoral cutaneous nerve (black arrow) traveling near the anterior superior iliac spine (ASIS), and the iliacus muscle in situ. An 8 ⫻ 6-cm piece of iliacus was harvested (below, left) and then transferred microsurgically to the patient’s ankle wound with a meshed skin graft (not shown). (Below, right) Three months later, the patient demonstrated a well-healed wound. 1557 Plastic and Reconstructive Surgery • April 2011 Fig. 6. Case 3. (Above, left) A soft-tissue traumatic injury with exposed patella and patellar tendon. A 6 ⫻ 6-cm iliacus muscle flap was harvested (above, right) and then transferred microsurgically to the patient’s lower knee wound with a meshed skin graft (below, left). One year later, the patient was walking and demonstrated a wellhealed wound with minimal contour deformity (below, right). The deep portion of the muscle was then cut from the bone and isolated on the iliacus branch so that the majority of the muscle was freely mobile in relation to the bone. The flap was then harvested and the flap vessels were anastomosed end-to-side to the external carotid and internal jugular veins. The iliacus was used to fill the defect left by the missing parotid and overlying skin and then covered by a split-thickness skin graft. The donor site was closed in the fashion recommended for iliac crest harvest with drill holes placed in the bone to anchor sutures from the abdominal musculature to the remaining crest. The patient tolerated the procedure well and recovered uneventfully. The flap survived and the skin graft demonstrated excellent take on the iliacus muscle despite aggressive postoperative irradiation. DISCUSSION These anatomical and clinical studies demonstrate that the iliacus muscle is an excellent alternative for the reconstruction of complex small to medium upper and lower extremity defects. It also has uses for head and neck and extremity recon- 1558 struction in conjunction with the iliac crest.13 It is a thin (approximately 1 to 1.5 cm thick), broad muscle with a consistent blood supply and a welldescribed pedicle (deep circumflex iliac artery and vein). Because it is the lesser contribution of musculature to the conjoined iliopsoas muscle, its loss results in a minimal deficit, and the donor-site scar remains hidden. The average size of flap that was evaluated was roughly 8 ⫻ 8 cm; thus, the flap is ideal for relatively small defects. Although it can, of course, be tapered down to any size, it is not recommended for defects larger than the dorsum of the typical patient’s hand. The iliacus is thinner than most other described muscle flaps and thus is suited for reconstructing defects of the hand, foot, or ankle where excessive bulk can be a significant functional problem for the patient. Wu et al. in 2009 Volume 127, Number 4 • Iliacus Muscle Flap Fig. 7. Case 4. A patient with a right lateral mandible and parotid and skin defect (above, left) underwent reconstruction with a composite free iliac crest and iliacus muscle. The deep portion of the muscle was cut from the bone and isolated on the iliacus branch so that the majority of the muscle was freely mobile in relation to the bone. The flap is shown still attached to its pedicle, with the bone (#) and the iliacus muscle (*) freely mobile in relation to each other (below). The bone was inset and the muscle transposed on top to fill in the parotid and skin defect. A skin graft was applied to the muscle and is shown reflected back to reveal the muscle underneath (above, center). The patient is shown after 6 months of healing and radiation therapy (above, right). described seven consecutive patients treated with vascularized iliac osteomuscular free flaps for bone and soft-tissue defects. They had 100 percent survival of the flaps with acceptable contour.13 As demonstrated in our first cases, the flap, like all muscle flaps, over time loses a great deal of its mass and flattens out significantly, resulting in an even contour over the defect. Another advantage of the flap is that its dissection is routinely started at the takeoff of the circumflex iliac vessels from the external iliac. Therefore, a relatively small incision can be used at first to determine whether the vascular anatomy of the deep circumflex iliac artery and vein is normal. If the pedicle cannot be identified, the incision can be extended medially to enable the surgeon to harvest rectus abdominis muscle in- stead. If the pedicle is identified, subsequent incisions to harvest the pedicle and muscle travel very close to the inguinal ligament and avoid injuring the iliohypogastric and ilioinguinal nerves.6 This is in contradistinction to the internal oblique muscle flap, which is based on the ascending branch of the deep circumflex iliac artery and vein.5,6 Dissection of the oblique puts at risk the aforementioned nerves and the lower thoracic nerves.6 The iliacus muscle is not part of the abdominal wall musculature; it is a thigh flexor in combination with its larger partner, the psoas. Harvest of the muscle therefore does not have the theoretical disadvantage of weakening the abdominal wall as significantly as harvest of other nearby muscles such as the rectus or internal oblique.6 It is nev- 1559 Plastic and Reconstructive Surgery • April 2011 ertheless recognized that any incision through abdominal wall musculature can lead to weakness and possible herniation. We have not seen this complication, but our clinical cases are few. Other potential disadvantages of the flap are as follows: (1) the anatomy is initially difficult for surgeons unfamiliar with iliac crest harvest and (2) the lateral femoral cutaneous nerve runs over or under the pedicle around the anterior superior iliac spine and may be damaged by an inexperienced dissector. Injuries to the nerve may result in paresthesias and chronic pain. We feel that, overall, the dissection can be carried out by an experienced microvascular surgeon by perusing the multiple texts describing the dissection of the iliac crest, even if the surgeon has no prior knowledge of the region. Once the inner aspect of the iliac crest is exposed, removal of the iliacus becomes a selfevident procedure. The vascular supply is easily visible, as are the important surrounding structures. CONCLUSIONS The iliacus muscle based on the iliacus branch of the deep circumflex iliac artery appears to be an expendable and readily harvested muscle. Its uses and advantages are significant and its limitations minor. A new muscle flap based on a previously undescribed branch of the deep circumflex iliac artery is outlined. Fresh cadaver dissections and live surgery were used to study the flap extensively. In each clinical use of the iliacus, the muscle demonstrated 100 percent survival. The advantages of this flap include its thin, flat nature; its consistent large pedicle; and its hidden donor site. Its disadvantages relate to the relative unfamiliarity of most surgeons with the region, damage to the lateral femoral cutaneous nerve, and possible weakening of the abdominal wall. We therefore recommend the flap as an excellent alternative for coverage of small to medium defects in the upper 1560 and lower extremities and in conjunction with iliac crest for the reconstruction of intraoral defects. Daniel A. Medalie, M.D. MetroHealth Medical Center 2500 MetroHealth Drive Cleveland, Ohio 44109 [email protected] REFERENCES 1. Asko-Selijavaara S, Lähteenmäki T, Waris T, Sundell B. Comparison of latissimus dorsi and rectus abdominis free flaps. Br J Plast Surg. 1987;40:620–628. 2. Chang TS, Wang W, Hsu CY. The free forearm flap: A report of 25 cases. Ann Acad Med Singapore 1982;11:236–240. 3. Heckler FG. Gracilis myocutaneous and muscle flaps. Clin Plast Surg. 1980;7:27–44. 4. Brent B, Upton J, Acland R, et al. Experience with the temporoparietal fascial free flap. Plast Reconstr Surg. 1985;76: 177–188. 5. Ramasastry SS, Tucker JB, Swartz WM, Hurwitz DJ. The internal oblique muscle flap: An anatomic and clinical study. Plast Reconstr Surg. 1984;73:721–733. 6. Taylor GI. The internal oblique muscle flap: An anatomic and clinical study (Discussion). Plast Reconstr Surg. 1984;73: 731–733. 7. Mathes SJ, Nahai F. Classification of the vascular anatomy of muscles: Experimental and clinical correlation. Plast Reconstr Surg. 1981;76:177–187. 8. Mathes SJ, Nahai F, Vasconez LO. Myocutaneous free-flap transfer: Anatomical and experimental considerations. Plast Reconstr Surg. 1978;62:162–166. 9. Taylor GI, Townsend P, Corlett R. Superiority of the deep circumflex iliac vessels as the supply for free groin flaps. Plast Reconstr Surg. 1979;64:595–604. 10. Strauch B, Yu H-L, Chen Z-W, Liebling R. In: Atlas of Microvascular Surgery: Anatomy and Operative Techniques. New York: Thieme; 1993:142–165. 11. Shenaq SM. Reconstruction of complex cranial and craniofacial defects utilizing iliac crest-internal oblique microsurgical free flap. Microsurgery 1988;9:154–158. 12. Urken ML, Weinberg H, Vickery C, Buchbinder D, Lawson W, Biller HF. The internal oblique-iliac crest free flap in composite defects of the oral cavity involving bone, skin, and mucosa. Laryngoscope 1991;101:257–270. 13. Wu K, Ren D, Hou S, et al. Vascularized iliac osteomuscular free flaps for composite soft tissue and bone defects of the lower extremity. Ann Plast Surg. 2009;63:53–58.