* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Antipsychotic drugs
Orphan drug wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Drug discovery wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription costs wikipedia , lookup
Drug interaction wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Neuropharmacology wikipedia , lookup
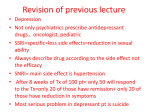
Psychopharmacology Ms.Viji Prasad.C Asst.Professor Department of Psychiatric Nursing • Antipsychotics ( typical and atypical) • Antidepressants (cyclic, SSRIs, MAOIs) • Mood stabilizers/ antimanic • antianxiety (hypnotics , sedatives ) • Antiepileptics • Antiparkinsonean agents • Drugs for alcoholism and drug dependence Contd… • Miscellaneous ( Ca channel blockers , drugs used in sleeping disorder, eating disorders , addiction and vitamins Antipsychotic drugs Tyrosine Tyrosine L-DOPA DA Dopamine Synapse Introduction • Antipsychotic drugs = “major tranquilizers”, “neuroleptic”. • Anti-schizophrenic drugs • Dopamine receptor antagonists • There are two broad categories of antipsychotic drugs: a. 1st generation or traditional (phenothiazines & butyrophenomes) b. 2nd generation or atypical (dual action drugs) • Drugs currently used in the prevention of psychosis. • They have also been termed neuroleptics, because they suppress motor activity and emotionality. ** These drugs are not a cure ** Pharmacokinetics • readily but incompletely absorbed • first pass metabolism • highly lipid soluble protein bound • completely metabolized • little excreted unchanged • t ½ is 10 -24 hours Mechanism Of Action • Dopamine receptor-blocking activity in the brain • Serotonin receptor-blocking activity in the brain • Block cholinergic, adrenergic & histaminergic receptors DOPAMINERGIC SYSTEM • The dopamine pathways are central to psychosis, the drug treatment of psychosis. dopamine pathways • Mesocortical pathway, extends from the ventral tegmental region of the mid-brain to the frontal cortex. One theory of schizophrenia poses that under activity in this pathway causes an early event in the development of schizophrenia: difficulties with executive and other cognitive functions. • (Behaviour ) • It is possible that under activity of this pathway may be involved in the negative symptoms of schizophrenia. • The side-effect of antipsychotics known as the “secondary” negative symptoms may arise in large part through further disruption of transmission in this pathway. • Mesolimbic pathway : extends from the ventral tegmentum to the nucleus accumbens, a limbic system structure. • Impulses then pass on to other components of the limbic system and temporal lobe structures (including the auditory cortex). Contd…. • In schizophrenia , when cognitive tasks are performed less efficiently, there is a compensatory increased activity in the mesolimbic pathway, and this produces the positive symptoms of hallucinations and delusions. • As the limbic system is also involved in pleasurable sensations, this pathway may also be involved in negative symptoms. • Nigrostriatal pathway: extends from the substantia nigra of the midbrain to the basal ganglia. (The basal ganglia are predominantly involved with movement, but some structures, such as the ventral striatum, also have limbic system functions.)….. VOLUNTARY MOVEMENT • Tuberoinfundibular pathway :extends from the hypothalamus to the portal system which serves the anterior pituitary. • In the healthy individual, tonic release of dopamine into this system inhibits the release of prolactin. • Unintentional disruption of this system leads to elevation of serum prolactin and the side-effects of gynecomastia, galactorrhea and sexual dysfunction. Dopamine pathways 1. Mesocortical pathway • Difficulties with executive and other cognitive functions. • Disturbnce in behaviour and negative symptoms 2.Mesolimbic pathway• Positive symptoms of hallucinations and delusions, and negative symptoms. 3. Nigrostriatal pathway- disturbance in voluntary movement 4. Tuberoinfundibular pathway- • Elevation of serum prolactin • Side-effects of gynecomastia, galactorrhea and sexual dysfunction. Mechanism of action • Exact mechanism is unknown • Antidopaminergic activity • Block D2 receptors which are mainly present in meso cortical- mesolimbic system (mesolimbic- emotional reactions), nigro-striatal system and tuberoinfundibular system) Antipsychotic Medications Block Dopamine Dopamine Speaking Brain Cell Listening Brain Cell Antipsychotic Medication Blocks Receptor Site Indications • Organic psychiatric disorders Delirium (haloperidol, risperidone) Dementia Delirium tremens Drug induced psychosis (amphetamine induced psychosis)- haloperidol Organic hallucinosis, organic delusional disorders Non organic psychiatric disorders • Schizophremia • Schizoaffective disorders • Manic episodes in bipolar disorders • Tourette syndrome • Senile dementia • Major depression • Delusional disorders Neurotic and other psychiatric disorders • Severe , intractable and disabling anxiety • Refractory obsessive compulsory disorder • Anorexia nervosa Medical disorders • Huntington’s chorea (haloperidol) • Intractable cough (chlorpromazine) • Nausea and vomiting • Tic disorders ( haloperidol, risperidone ) Contd.. Non psychiatric indications • Anti-emetic effect (prochlor perazine) • Anti-pruritic effect (phenothiazines) • Preoperative anesthesia.(Promethazine) • Neuroleptic anesthesia.(Droperidol) A. Classification 1. Typical (conventional) antipsychotic drugs: – Often sub classified according to their oral potency (high potency or low potency). a. High-potency drugs – piperazine phenothiazines, e.g., fluphenazine – butyrophenones e.g., haloperidol – more likely to produce extra pyramidal reactions. a. Low-potency drugs • aliphatic phenothiazines, e.g.,triflupromazine • piperidine phenothiazines, e.g., thioridazine – are less likely to produce acute extrapyramidal reactions – more likely to produce sedation and postural hypotension. 2. Atypical antipsychotic drugs - example: Clozapine, risperidone, olanzapine, quetiapine, aripiprazole. – have generally replaced the conventional drugs for initial treatment of first-episode patients. – Clozapine is reserved for treatment-resistant patients. 3. Other typical heterocyclic antipsychotic drugs – e.g., loxapine and molindone – intermediate potency – have no clear advantage over other conventional drugs. E. • Adverse effects and contraindications The adverse effects of antipsychotic agents are due to their antagonist actions at receptors in the CNS – dopamine D2-receptors , histamine H1-receptors (and possibly serotonin receptors) in the periphery – muscarinic cholinoceptors and α-adrenoceptors 1. Central nervous system A. Extra pyramidal syndromes 1. These adverse effects are related to a dopaminereceptor blockade in the basal ganglia that leads to an imbalance in dopamine and acetylcholine actions in the nigro striatal pathway. 2. These effects are a major cause of noncompliance. Extra pyramidal effects are: • most likely to occur with high-potency conventional antipsychotic drugs that have a high affinity for post junctional dopamine D2- receptors in the basal ganglia. • occur with few atypical drugs like risperidone. - These effects can sometimes spontaneously remit. Extra pyramidal syndromes include the following: 1. Acute dystonia : sustained muscle contractions cause twisting and repetitive movements or abnormal postures – This condition is often elicited during the first week of therapy. Acute dystonia Contd… 2. Akathisia is the irresistible compulsion to be in motion. Walkies and talkies ( urge to move about) – This condition can develop as early as the first 2 weeks of treatment or as late as 60 days into therapy. Contd… 3. Parkinsonian-like syndrome • Parkinsonian-like syndrome is characterized by tremors, bradykinesia, rigidity, and other signs of parkinsonism. • This syndrome can develop from 5 days to weeks into treatment. 4. Periodic Tremor Rabbit Syndrome Peri-oral tremors after months or years of treatment B. Tardive dyskinesia (10—20%) • CNS disorder characterized by: • twitching of the face and tongue • involuntary motor movements of the trunk and limbs • More likely with conventional antipsychotic agents. The only effective treatment for tardive dyskinesia is the discontinuation of treatment. Orofacial movements Dystonic posture • Tardive dyskinesia generally occurs after months to years of drug exposure; it may be exacerbated or precipitated by the discontinuation of therapy. • Tardive dyskinesia is often irreversible. • More likely to occur in the elderly or in institutionalized patients who receive long-term, high-dose therapy. c. • Neuroleptic malignant syndrome Due to excessively rapid blockade of postsynaptic dopamine receptors. • This syndrome is characterized by: – altered blood pressure and heart rate. – muscle rigidity Contd… – diaphoresis – profound hyperthermia • This condition occurs, often explosively, in 1% of patients; it is associated with a 20% mortality rate. NMS • This condition is treated by: 1.Discontinuing drug therapy 2.Initiating supportive measures, including the use of bromocriptine to overcome the dopamine receptor blockade 3.Muscle relaxants such as dantrolene and diazepam to reduce muscle rigidity. d. • Sedation More likely with low-potency antipsychotic agents and with the atypical agents, are due to a central histamine H1-receptor blockade. • These effects may be mild to severe. • The elderly are particularly at risk. • May be temporary e. Confusional state with memory impairment. - This effect is likely with antipsychotic agents with pronounced antimuscarinic activity. f. Seizures: Seizures are especially common with chlorpromazine and clozapine. - This effect is due to a lowering of the seizure threshold; antipsychotic drugs may precipitate or unmask epilepsy. 2. Autonomic Nervous system 1. α-Adrenoceptor blockade More likely to occur with: – conventional low-potency – atypical antipsychotic agents. • Postural hypotension- phenothiazines when a person moves to a more vertical position: from sitting to standing or from lying down to sitting or standing. CONTD.. • Orthostatic hypotension – (atypical drugs) symptoms: dizziness, faintness or lightheadedness which appear only on standing, and which are caused by low blood pressure. • Failure to ejaculate –(phenothiazines) contd.. 2. Muscarinic cholinoceptor blockade • More common with: conventional low-potency antipsychotic agents atypical agent like clozapine. symptoms : (dry mouth, constipation, urinary retention, and visual problems) • Elderly patients are more at risk 3. Endocrine and metabolic disturbances • Most likely with – most conventional antipsychotic agents – atypical agent risperidone • Due to dopamine (D2)-receptor antagonist activity in the pituitary, resulting in hyperprolactinemia. Contd.. In women, these disturbances include: galactorrhea loss of libido delayed ovulation and menstruation or amenorrhea. In men; gynecomastia impotence. Contd.. Weight gain, which is likely with: most conventional atypical antipsychotic agents, except aripiprazole and ziprasidone, may be due in part to histamine H1-receptor antagonist activity. 4. Other adverse effects a. Withdrawal-like syndrome 1. Symptoms: nausea, vomiting, insomnia, and headache • in 30% of patients, especially those receiving lowpotency antipsychotic drugs. 2. Symptoms may persist for up to 2 weeks. 3. Symptoms can be minimized with a tapered reduction of drug dosage. b. Cardiac arrhythmias • More likely with thioridazine and ziprasidone, which can prolong the Q-T interval and lead to conduction block and sudden death. c. Blood dyscrasias – rare, except in the case of clozapine, which may induce agranulocytosis (severe neutropenia) in up to 3% of patients and, therefore, is used only when other drug groups prove ineffective. c. Cholestatic jaundice, which is caused primarily by chlorpromazine d. Photosensitivity 1. The effect is specific to chlorpromazine – it includes dermatitis (5%), rash, sunburn, and pigmentation, and it may be irreversible. 2. Chlorpromazine and high-dose thioridazine also produce retinitis pigmentosa