* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Plasma cell dyscrasias
Cancer immunotherapy wikipedia , lookup
Monoclonal antibody wikipedia , lookup
Neuromyelitis optica wikipedia , lookup
Human cytomegalovirus wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Pathophysiology of multiple sclerosis wikipedia , lookup
Sjögren syndrome wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Multiple sclerosis signs and symptoms wikipedia , lookup
X-linked severe combined immunodeficiency wikipedia , lookup
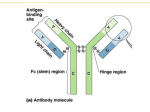
Plasma cell dyscrasias Mark Drayson 20 18 16 14 12 10 8 6 4 2 0 Age <45 45-54 55-64 65-74 75+ % 1.0 5.0 15.4 31.6 47.0 <4 5 45 -4 50 9 -5 4 55 -5 60 9 -6 4 65 -6 70 9 -7 75 4 -7 9 80 -8 85 4 -8 9 90 + Deaths in age cohort as percentage total deaths Mortality statistics for England and Wales. Deaths attributed to multiple myeloma from 1988-1997 by age cohort as a percentage of total (21,257) deaths Age Cohort (years) Types of normal plasma cells 1) Short lived plasma cells found in red pulp of spleen and medullary cords of lymph nodes IgM >>IgG/IgA Waldenstroms 2) Bone marrow plasma cells IgG, IgA, IgD, IgE, very rarely IgM Derived from germinal centres lymph nodes, spleen mutations in variable region gene segments / high affinity Multiple myeloma 3) Mucosal plasma cells IgA mostly germinal centre derived malignancy is rare 4) Plasma cells from type 1 B cells pleural/peritoneal cavities Self replenishing from fetal precursors natural antibodies IgM CLL Conditions with elevated serum immunoglobulins / paraproteins Chronic infection, liver disease, HepC, connective tissue disease, HIV, Hodgkins Post stem cell rescue, polyclonal/oligoclonal/temporary monoclonal MGUS monoclonal gammopathy of undetermined significance Light chain amyloid Paraprotein neuropathies POEMS etc. Lymphoplasmacytoid lymphoma (Waldenstroms) Other B cell NHL (marginal zone lymphoma) Multiple myeloma Polyclonal Immunoglobulin Small IgG kappa paraprotein With no immunoparesis Large IgG lambda paraprotein With immunoparesis Immunoparesis in myeloma IgM (2695 patients) N.R. 0.5 – 2.0 g/l <0.5g/l >0.5g/l >1.0g/l >2.0g/l 82% 18% 4.0% 0.8% IgA and IgM in patients with IgG paraprotein (1498 patients) N.R. IgM 0.5 – 2.0 g/l IgA 0.8 – 4.0 g/l IgM > 0.5 and IgA > 0.8 11% IgM > 1.0 and IgA > 2.0 1.4% IgM > 2.0 and IgA > 4.0 0.2% IgM and IgG in patients with IgA paraprotein (684 patients) N.R. IgM 0.5 – 2.0 g/l IgG 6.0 - 16.0 g/l IgM > 0.5 and IgG > 6.0 IgM > 1.0 and IgG > 10.0 IgM > 2.0 and IgG > 16.0 8.3% 0.7% 0% IgM, IgA and IgG in patients with light chain myeloma (349 patients) N.R. IgM 0.5 – 2.0 g/l IgG 6.0 - 16.0 g/l IgM > 0.5 and IgG > 6.0 IgM > 1.0 and IgG > 10.0 IgM > 2.0 and IgG > 16.0 IgA >0.8 IgM > 1.0 and IgG > 10.0 9.7% 0.8% 0% 8.0% Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders International Myeloma Working Group B. J Haem 2003, 121 749-757 MGUS •M-protein in serum <30g/l •Bone marrow plasma cells <10% low level infiltration in trephine biopsy •No evidence of other B-cell proliferative disorder •No related organ or tissue impairment MGUS a paraprotein with no evidence of related disease Prevalence >50yrs 1% >70yrs 3% 70% IgG, 12% IgA and 15% IgM 38% have immune paresis 31% have free light chains in urine MGUS associated with amyloid MGUS associated with paraprotein related neurological syndromes A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002 Feb 21;346(8):564-9. 1384 patients 11,009 years follow up 1960 – 1994 115 progressed – relative risk 7.3 (25 MM, 46 Waldenstroms, 2 IgM lymphoma, 8 primary amyloid, 0.9 CLL) actual risk >1% per year (12% at 10 years, 30% at 25 years) Initial paraprotein concentration and IgM/IgA versus IgG only significant prognostic indicators. Paraprotein level 10 year risk of progression to disease:<5g/l 6% 15g/l 11% 20g/l 20% 25g/l 24% 30g/l 34% Symptomatic myeloma Must have evidence of related organ or tissue impairment (ROTI) C calcium >0.25mmol/l above normal / >2.75mmol/l R renal impairment attributable to myeloma A anaemia 2g/dl below normal or <10g/dl B bone lesions lytic or osteoporosis with compression fractue O other symptomatic hyperviscosity, amyloidosis, recurrent bacterial infection - With •Bone marrow clonal plasma cells (usually>10%) •M-protein in serum and / or urine (usually) Asymptomatic myeloma No evidence of end-organ damage with both: •Bone marrow plasma cells >10% •M-protein in serum and or urine SYMPTOMATIC MYELOMA ASYMPTOMATIC MYELOMA MGUS Bone marrow clonal plasma cells In 95% of cases is >10% Usually present at >10% Often detectable Always <10% Serum paraprotein Present in 80%. No specific diagnostic levels Always present If plasma cells <10% then >30g/l Always present <30 g/l Bence-Jones proteinuria Present in 70% 15 – 20% no serum paraprotein Present in >50% Present in 30% Immune paresis Present in >80% Present in >50% Present in 40% Symptoms Present in 85% Absent Absent Myeloma related organ dysfunction Always present Absent Absent UK Guidelines on the diagnosis and management of multiple myeloma. Br J Haematol. 2001 Dec;115(3):522-40. BCSH and UK MF BSH Website Up-dated with NORDIC group Summer 2005 Indications for Starting Therapy 1. Chemotherapy is indicated for management of symptomatic myeloma 2. Chemotherapy is not indicated for patients with MGUS or those with asymptomatic myeloma (equivocal/indolent/smouldering). Patients with no symptoms, normal Hb, calcium and renal function and no bone lesions may remain stable for a long period without treatment. Early intervention has shown no benefit in 2 randomised controlled trials (Hjorth. 1993; Riccardi et al 2000). Overall survival by age and by plateau status 100 < 65yrs - 571 patients > 65yrs - 428 patients % alive 75 50 31% 25 39% 0 0 1 2 3 4 5 6 7 Years from entry to trial 8 9 10 Relapse free interval from start of plateau phase 100 < 65 65 and over % relapse free 75 50 25 0 0 1 2 3 4 5 6 Years from plateau 7 8 9 10 Overall survival from progression 100 % alive 75 < 65 65 and over 50 25 0 0 1 2 3 4 5 6 7 Years from progression 8 9 10 Infection in myeloma Respiratory tract encapsulated pyogenic bacteria Incidence 14% in year before diagnosis 25% in first 3 months 10% per patient year in plateau Innate immunity IL-6, CRP Specific immunity TI2 antibody responses Intravenous immunoglobulin replacement First 3 months MRC IVIg trial 203 patients no significant benefit ?Problems with innate immunity predominate Antibiotic prophylaxis in first 3 months •reduce morbidity / mortality from infection Am J Med 1996 - 54 patients first 3 months Control patients 11 infections Septrin 2 infections p=0.004 •Reduce disease activity by reducing infection induced IL-6 levels? Intravenous immunoglobulin replacement Plateau phase 82 patients Chapel et al Lancet 1994 p = 0.019 Placebo 38 infections in 470 patient months IVIg 19 infections in 449 patient months Vaccination in plateau 5 studies (13 – 52 patients per trial) Pneumovax (TI2) 20% normal response Haemophillus conj (TD) normal responses Study of Hib and new pneumococcal conjugate vaccine In plateau phase? Immunoglobulin 2 identical heavy chains 2 identical light chains Either Kappa Or Lambda (Gene chromosome 14) (Gene chromosome 2) (Gene chromosome 22) Normal plasma cell secretion of whole immunoglobulin and free light chains Kappa Plasma cells Lambda Plasma cells Production of FLC Increased malignant FLC Decreased alternate polyclonal FLC FLC BLOOD FLC from blood by GF do not alter Κ/Λ serum FLC ratio FLC FL C NEOPLASTIC CLONE GLOMERULAR FILTRATION Changes in removal of FLC TUBULAR REABSORPTION FLC production and filtration must exceed TR for FLC to appear in urine FLC Therefore altered serum κ/λ FLC ratio 32% of MM patients have <40mg/l FLC in urine URINE FLC 100000 S e rum flc La m bda (m g/L) 10000 1000 Normals 100 10 1 0.1 0.1 1 10 100 1000 Serum flc Kappa (mg/L) 10000 100000 100000 S erum flc La m bda (m g/L) 10000 Normals 1000 Lambda BJ 100 Kappa BJ 10 1 0.1 0.1 1 10 100 1000 Serum flc Kappa (mg/L) 10000 100000 Lancet 2003 361 489-491 100000 Free light chain serum Lambda (mg/L) Kappa BJM Lambda BJM 10000 Nonsecretory myeloma 1000 Normal sera 100 10 1 0.1 0.1 1 10 100 1000 Free light chain serum Kappa (mg/L) 10000 100000 100000 Free light chain serum Lambda (mg/L) Kappa BJM Lambda BJM 10000 Nonsecretory myeloma AL Amyloidosis 1000 Normal sera 100 10 1 0.1 0.1 1 10 100 1000 Free light chain serum Kappa (mg/L) 10000 100000 Serum free light chain measurements Diagnosis: More sensitive than immunofixation (10-100x) No problem with renal threshold 1/3 patients with no detectable urinary FLC FLC only myeloma, Non-secretory myeloma Amyloidosis Monitoring: Not confounded by changes in renal function Rapid response to changes in tumour load because of short half life (hours) More sensitive (What is a complete response?) Observations of the MRC Myelomatosis Trials IVth MP vs MVP 3 litres of fluid per day Vth M7 vs ABCM 316 / 314 P=0.003 VIth ABCM vs ABCMP 343 / 342 P=0.11 VIIIth ABCM vs ABCM/CW 536 Bisphosphonates reduce skeletal morbidity Interferon in prolongs plateau phase but not overall survival Overall survival by treatment 100 ABCM ABCMP % alive 75 χ2=2.52, P=0.11 50 25 0 0 2 4 6 8 Years from entry to trial 10 12 The clodronate trial showed: •Reduced morbidity from skeletal disease •Patients (155) without overt skeletal disease at presentation appeared to benefit more than patients with fractures at presentation •No overall survival benefit Overall survival by treatment CLODRONATE PLACEBO 100 CLODRONATE PLACEBO 100 χ2=0.94, P=0.33 χ2=8.24, P=0.004 75 % alive 75 % alive Overall survival by treatment for those patients presenting with no fractures 50 50 25 25 0 0 0 2 4 6 8 Years from entry to trial 10 12 0 2 4 6 8 Years from entry to trial 10 12 Non-intensive treatment Melphalan +/- prednisolone ABCM Intensive treatment VAD / CVAMP (avoid stem cell damage) Then high dose melphalan with PBSCT mortality <5% Allogeneic high mortality 20% - 38% Interferon in plateau phase - probably not Intensive versus conventional chemotherapy New England J Med 2003 348 1875 - 83 THALIDOMIDE MONOCLONALS MINI-ALLOGRAFTS PROTEASOME INHIBITORS MRC 9 Clodronate / zoledronate CVAD / CTD or MP / CTD Thalidomide maintenance MERIT Randomisation to plasma exchange