* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiorespiratory Resuscitation
Survey
Document related concepts
Transcript
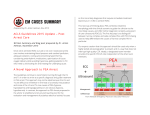
Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Short Title: Cardiopulmonary Resuscitation Full Title: Date of production/Last revision: Guideline for the management of cardiopulmonary resuscitation in children and young people January 2007 Explicit definition of patient group to which it applies: This guideline applies to all children and young people under the age of 19 years. Name of contact author Dr Gillian Body, Paediatric SpR Dr Stephanie Smith, Consultant Paediatrician Ext: 64042 January 2009 Revision Date This guideline has been registered with the Trust. However, clinical guidelines are 'guidelines' only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date. Cardiopulmonary Resuscitation In the event of Cardiac Arrest, call 2222, give location, and ask for the Paediatric Arrest Team. Cardiac arrest has occurred when there are no palpable central pulses. Effective basic life support must be established before any specific therapy is started. In children cardiac arrest is a rare event, and usually the result of prolonged hypoxia. This is different from adults where cardiac arrest is usually due to a primary cardiac problem. Scope of the Guideline This guideline outlines the advanced management of cardiac arrest in children. It is assumed that cardiac arrest has been confirmed, and Basic life support is in progress. BLS is outlined at the end of this document. Before the Child Arrives It is best to be prepared, if possible. Try to obtain basic information from ambulance crew – age or weight, time of arrest, any drugs and treatment given in transit. Assemble your team and assign roles, including allocating a team leader. o You may need to limit the number of people involved in the immediate area. o Allocate a member of staff to be with the parents if they wish to be present during resuscitation. (It is accepted good practice for parents/guardians to be present in the resuscitation room; however they should have a member of staff with them.) o A scribe is an important role – documenting timing and treatments. o Inform the Consultant on call. Consider any known resuscitation or end of life plans Calculate drug doses, (eg Adrenaline) in advance if possible. o If fluids are likely to be needed, start drawing them up in advance as it is a time consuming process. o Other drugs can be calculated depending on the history you obtain, (eg IV salbutamol for an asthmatic who has arrested). Gillian Body Page 1 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Broselow tapes and kits are available in some clinical areas to assist in the cardiac arrest situation. The child’s weight can be estimated using these tapes, or by using the formula; Weight (kg) = (Age in years + 4) x 2 Be prepared to adjust this dose once the child arrives. Not all children follow the formula! If the child is admitted as a child on the Paediatric wards – they should be treated as a child, and Paediatric resuscitation algorithms followed. Management of cardiac arrest follows ABC; Airway Breathing Circulation The airway, breathing and circulation must be assessed in this order and problems addressed as they are recognised. ONCE CARDIAC ARREST IS CONFIRMED, THE PATIENT SHOULD RECEIVE GOOD, EFFECTIVE, CONTINUOUS BASIC LIFE SUPPORT. Basic life support is detailed at the end of this guideline. BLS should be in progress before any drug treatment is given. Whilst BLS is ongoing a monitor should be attached to establish the arrest rhythm. Gillian Body Page 2 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Cardiac Arrest Rhythms and Management This guideline will outline the management of two different Arrest protocols 1. 2. Asystole and Pulseless Electrical Activity (PEA) Ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT) Cardiac Arrest confirmed Good BLS in progress Attach monitor VF Pulseless VT Gillian Body Determine arrest rhythm Page 3 of 12 PEA Aystole January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Asystole This is the most common arrest rhythm in children, and is the response of the young heart to prolonged severe hypoxia and acidosis. The ECG/monitor appearance of asystole is an almost straight line, with occasional p waves seen. Check that there are no loose connections and turn up the gain on the ECG monitor. Pulseless Electrical Activity (P E A) This is an impalpable pulse in the presence on the monitor, of a rhythm that should produce a pulse. The most common cause in children is profound shock. (Note: the term Electro-mechanical dissociation (EMD) is sometimes used interchangeably, although strictly this refers to a specific situation in adults with coronary disease) Both ASYSTOLE and PEA follow the same algorithm which is outlined on the following page. Before the administration of any drug the patient must be receiving continuous and effective basic life support NOTES: (notes relate to the numbers on the algorithm on the next page) 1. Intubation will protect the airway, but attempts to intubate should not delay good BLS. Effective ventilation can be maintained using a bag-valve-mask system. Once intubated, cardiac compressions should be continuous, unless doing so prevents effective ventilation. IV access can be attempted, but if not successful quickly – intraosseous is the preferred route of drug administration. The tracheal route is not recommended. 2. Adrenaline should be given by IV or IO route, followed by saline flush. Doses should be repeated every 3-5 minutes. A monitor check is performed every 2 minutes, and a pulse check performed if there is any change in rhythm. Giving the adrenaline before every second pulse check, means it is given, in effect, every 4 minutes. 3. The four Hs and 4 Ts are some of the reversible causes of arrest, and should all be considered whilst resuscitation continues. These are outlined in the following table. Alkalising agents, (Sodium Bicarbonate: 1 mmol/kg = 1 ml/kg of an 8.4% solution), can be considered in children with prolonged arrest / TCA overdose / hyperkalaemia. Gillian Body Page 4 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Good effective BLS Ventilate with high flow oxygen Intubate Obtain IV or IO access Adrenaline IV or IO 10 mcg/kg 0.1ml/kg of 1:10,000 1 2 Check monitor every 2 minutes 4 minutes CPR Consider 4 Hs and 4 Ts Consider alkalising agents and repeat as needed 3 Algorithm for asystole and PEA 4 Hs and 4 Ts Hypoxia Hypovolaemia Hyper/Hypokalaemia/metabolic Hypothermia Particular relevance in asystole Yes Yes Cardiac Tamponade Tension pneumothorax Toxins Thrombo-embolic events Gillian Body Particular relevance in PEA Yes Yes (low Ca) Yes Yes Yes Yes Page 5 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Ventricular Fibrillation This arrhythmia is uncommon in children but may occur in hypothermia, tricyclic antidepressant poisoning, and in the presence of pre-existing cardiac disease. Pulseless Ventricular Tachycardia This is also an uncommon rhythm in children, but may occur in similar situations to ventricular fibrillation. (Note: pulsed VT is treated differently). Gillian Body Page 6 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation 1 DC shock 4J/kg 3 2 mins CPR Check monitor Intubate. High flow O2 Obtain IV/IO access 2 DC shock 4J/kg 2 mins CPR Check monitor Intubate. High flow O2 Obtain IV/IO access Adrenaline 10mcg/kg then DC shock 4J/kg 4 2 mins CPR Check monitor Amiodarone 5mg/kg then DC shock 4J/kg 5 2 mins CPR Check monitor Adrenaline 10mcg/kg then DC shock 4J/kg 6 2 mins CPR Check monitor 2 mins CPR Check monitor DC shock 4J/kg 7 Consider 4 Hs and 4 Ts Consider alkalising agents and repeat as needed Algorithm for VF and pulseless VT Gillian Body Page 7 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation NOTES: (notes relate to numbers on algorithm) 1. and 2. Defibrillation is the first action, as it is defibrillation that will restore the heart to a sinus rhythm. It is likely, however, that in an unmonitored patient, BLS will be in progress while the rhythm is being determined. Shocks are given as single shocks at 4J/kg. CPR for 2 minutes is continued immediately, and then the monitor checked, (with a brief pause in compressions) before the next shock. A single shock should be given every 2 minutes. Cardiac compressions should be interrupted for as little time as possible. 3. Intubation will protect the airway, but attempts to intubate should not delay good BLS or defibrillation. Effective ventilation can be maintained using a bag-valve-mask system. Once intubated, cardiac compressions should be continuous, unless doing so prevents effective ventilation. IV access can be attempted, but if not successful quickly – intraosseous is the preferred route of drug administration. The tracheal route is not recommended. 4. Adrenaline is given immediately before the 3rd shock, after the monitor check that confirms there is no change in rhythm. As the shock comes immediately after this, the adrenaline will not be circulated until CPR resumes after the shock. The adrenaline is to support coronary and cerebral perfusion. 5. Amiodarone is the anti-arrhythmic drug of choice in shock resistant VF. It aims to keep the heart in a sinus rhythm once the shock has been successful. Lignocaine (Lidocaine) can be used if Amiodarone is not available. 6. The cycle of shocks every 2 minutes after a monitor check should continue, with Adrenaline given every 4 minutes (alternate shocks). A pulse check should be done if a change in rhythm is seen that is compatible with a perfusing rhythm. If there is a change in rhythm, then resuscitation should follow the appropriate algorithm. 7. The four Hs and 4 Ts are some of the reversible causes of arrest, and should all be considered whilst resuscitation continues. These are outlined in the table below. Particular attention should be paid to those which are more common in VF or pulseless VT. Hypothermic patients below 320C should be actively warmed, and the number of shocks reduced until the patient is warmer. Alkalising agents, (Sodium Bicarbonate: 1 mmol/kg = 1 ml/kg of an 8.4% solution), be considered in children with prolonged arrest / TCA overdose / hyperkalaemia. can Particular relevance in VF/pulseless VT 4 Hs and 4 Ts Hypoxia Hypovolaemia Hyper/Hypokalaemia/metabolic Hypothermia Yes Yes Cardiac Tamponade Tension pneumothorax Toxins Yes Thrombo-embolic events Gillian Body Page 8 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation If resuscitation is unsuccessful 1. Ensure that all team members present are happy to stop the resuscitation attempt. Special consideration needs to be given to children who are hypothermic (prolonged period outside / drowning), as resuscitation may need to continue until the child has a normal body temperature. 2. Spend time with the relatives and ensure they are being supported by a member of staff. 3. Inform the GP and all other relevant parties 4. If appropriate refer to the: Sudden Unexpected Death guideline Care of the Next Infant (CONI) guideline If resuscitation is successful 1. Assessment of ABCD should be made. The airway may need to be protected by controlled intubation if not already done. 2. Post resuscitation care should be discussed with the consultant on call for PICU. Some children will remain intubated and ventilated and need inotropic support. 3. Attention should be paid to electrolytes, glucose and temperature control. 4. Further evidence of the cause of the arrest should be sought if this is not yet determined. Non-Accidental Injury should be considered. 5. If appropriate refer to the Acute Life Threatening Event guideline. Gillian Body Page 9 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Basic Life Support SAFE Shout for Help Approach with Care Free from Danger Evaluate ABC Infant Neutral position SAFE Approach Are you alright? Airway Opening Manoeuvres Head tilt, chin lift Jaw thrust Child Sniffing position Look, listen, feel for 10 seconds 5 rescue breaths Brachial/femoral Two fingers, compress to between 1/3 and ½ depth of chest Check for pulse/signs of circulation Carotid Pulse 15:2 Compressions/ventilation Heel of 1 or 2 hands, compress to between 1/3 and ½ depth of chest Ensure help on the way. Call 999/2222 Gillian Body Page 10 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Notes An ‘infant’ is under 1 year of age, and a ‘child’ from 1yr to ‘puberty’. For this guideline this includes all those children over 1 yr admitted to the paediatric wards. The landmark for compressions is one finger breadth above the xiphisternum in all ages. The rate of compressions is 100 per minute. With pauses for ventilation less than 100 will be achieved, however the rate should be maintained. Compressions should commence if no pulse, no signs of circulation, or a pulse less than 60 in a shocked child with circulatory compromise. Airway Adjuncts and Intubation Oropharyngeal airways (Guedel): A suitable sized Guedel airway reaches from the centre of the incisors to the angle of the mandible when laid on the face concave side up. In infants and small children the airway should be inserted the “correct” way up, under direct vision, using a tongue depressor or laryngoscope to avoid soft tissue trauma. Nasopharyngeal Tubes A suitable size tube reaches from the tip of the nose to the tragus of the ear. The diameter should be that which snugly fits in the child’s nostril –this is approximately the size of their little finger, or can be estimated using the formula below. Intubation Children frequently require endotracheal intubation during cardiac arrest. Uncuffed or cuffed tubes can be used. A change in tube size (or to a cuffed tube) may be needed if there is difficulty ventilating the intubated child. The appropriate size of an endotracheal tube is estimated using the following formula; Endotracheal tube size Internal diameter (mm) = (Age/4) + 4 Length (cm) = (Age/2) + 12 for an oral tube Length (cm) = (Age/2) + 15 for a nasal tube These formulae are appropriate for ages over 1 year. Neonates usually require a tube of internal diameter 3-3.5 mm. Another useful guide is to use a tube of the same diameter as the child’s little finger, or a size that will just fit into the nostril. Gillian Body Page 11 of 12 January 2007 Paediatric Clinical Guideline Emergency: 1.1 Cardiopulmonary Resuscitation Title Cardio-Respiratory Arrest Guideline Number 1.1 Version Final Distribution All wards QMC and CHN Author Dr Gillian Body Paediatric Specialist Registrar Dr Stephanie Smith Consultant Emergency Paediatrician Document Derivation APLS Manual 4th Ed ILCOR Update 2005 First Issued Review Date January 2009 Latest Version Date January 2007 Ratified By Paediatric Clinical Guidelines Meeting Date January 2007 Audit Amendments Gillian Body Induction Programme Page 12 of 12 January 2007