* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download The use of BNP to monitor and guide treatment of heart failure patients
Survey
Document related concepts
Transcript
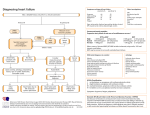
Health Policy Advisory Committee on Technology Technology Brief The use of BNP to monitor and guide treatment of heart failure patients August 2012 © State of Queensland (Queensland Health) 2012 This work is licensed under a Creative Commons Attribution Non-Commercial No Derivatives 2.5 Australia licence. In essence, you are free to copy and communicate the work in its current form for non-commercial purposes, as long as you attribute the authors and abide by the licence terms. You may not alter or adapt the work in any way. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/2.5/au/. For further information, contact the HealthPACT Secretariat at: HealthPACT Secretariat c/o Access Improvement Service, Centre for Healthcare Improvement, Queensland Health Lobby 2, Level 2, Citilink Business Centre 153 Campbell Street, Bowen Hills QLD 4006 Postal Address: GPO Box 48, Brisbane Qld 4001 Email: [email protected] Telephone: +61 7 3131 6969 For permissions beyond the scope of this licence contact: Intellectual Property Officer, Queensland Health, GPO Box 48, Brisbane Qld 4001, email [email protected], phone (07) 3234 1479. Electronic copies can be obtained from: http://www.health.qld.gov.au/healthpact DISCLAIMER: This brief is published with the intention of providing information of interest. It is based on information available at the time of research and cannot be expected to cover any developments arising from subsequent improvements to health technologies. This brief is based on a limited literature search and is not a definitive statement on the safety, effectiveness or costeffectiveness of the health technology covered. The State of Queensland acting through Queensland Health (“Queensland Health”) does not guarantee the accuracy, currency or completeness of the information in this brief. Information may contain or summarise the views of others, and not necessarily reflect the views of Queensland Health. This brief is not intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for a health professional's advice. It must not be relied upon without verification from authoritative sources. Queensland Health does not accept any liability, including for any injury, loss or damage, incurred by use of or reliance on the information. This brief was commissioned by Queensland Health, in its role as the Secretariat of the Health Policy Advisory Committee on Technology (HealthPACT). The production of this brief was overseen by HealthPACT. HealthPACT comprises representatives from health departments in all States and Territories, the Australian and New Zealand governments and MSAC. It is a subcommittee of the Australian Health Ministers’ Advisory Council (AHMAC), reporting to AHMAC’s Hospital Principal Committee (HPC). AHMAC supports HealthPACT through funding. This brief was prepared by Linda Mundy from the HealthPACT Secretariat. TECHNOLOGY BRIEF Register ID WP123 (NZ referral) Name of Technology B-type natriuretic peptide (BNP) assay Purpose and Target Group To monitor and guide the treatment of heart failure patients Stage of Development in Australia Yet to emerge Established Experimental Established but changed indication or modification of technique Investigational Should be taken out of use Nearly established Australian Therapeutic Goods Administration Approval Yes No Not applicable ARTG number International Utilisation COUNTRY LEVEL OF USE Trials underway or completed Limited use Widely diffused New Zealand France USA Switzerland Impact summary A number of companies manufacture immunoassays for the detection of either brain (or B-type) natriuretic peptide (BNP) or the inactive N-terminal proBNP including Roche Diagnostics (Elecsys® pro-BNP), Abbott Diagnostics (AxSYM® BNP) and Alere Triage® BNP Test (formerly Biosite Inc). In vitro diagnostic medical devices (IVDs), such as these immunoassays, are currently not required to be registered on the Australian Register of Therapeutic Goods; however, under the TGA regulatory framework introduced in July 2010, IVDs will be required to be registered as of July 2014. Since July 2008, a Medicare Benefits Schedule item number (66830) has existed for the “Quantitation of BNP or NT-proBNP for the diagnosis of heart failure in patients presenting with dyspnoea to a hospital Emergency Department”. This BNP to monitor and guide treatment of heart failure patients: August 2012 1 Brief is intended to assess the current safety and effectiveness evidence for the use of BNP assays to monitor and guide treatment in patients already diagnosed with heart failure. Background Heart failure (HF) is a common condition with an incidence and prevalence that increases with age. HF occurs when heart function is impaired causing the heart to pump blood less efficiently around the body. HF may be caused by a number of diseases or conditions that impair or overload the heart, including hypertension, ischaemic heart disease or cardiomyopathy. Symptoms of severe heart failure include chronic tiredness and dyspnoea or shortness of breath at rest or on exertion. HF results in irreversible damage to the heart muscle and, as such, is generally considered to be life-threatening and associated with poor survival.1 Systolic HF, where the heart fails to effectively contract in systole, is the most common cause of chronic HF. Diastolic HF, which is more common in the elderly, retains systolic function and is indicated by the impairment of left ventricle filling during diastole. 2 There are two types of cardiac natriuretic peptides secreted by the heart: atrial (ANP) and brain (BNP). BNP is secreted constitutively from myocytes, with secretion increasing in response to pressure and volume overload in the ventricles, such as that noted to occur in heart failure patients. Two forms of BNP circulate in the plasma, BNP-32 and the inactive pro-hormone N-terminal fragment BNP (NTproBNP). The natriuretic peptides bind to, and mediate, activity via receptors found in a number of tissues, including the kidneys, brain, heart and the adrenal glands in addition to the vasculature. The physiological effects of the natriuretic peptides are varied including inhibition of neural-hormonal over-activation, relaxation of vascular and pulmonary smooth muscle, and the inhibition of cardiac hypertrophy and ventricular fibrosis. In addition, the peptides may cause lipolysis, increase the permeability of the endothelial vasculature and reduce intravascular volumes.3, 4 Normal plasma levels of BNP and NT-proBNP are 7.4 ng/L (range 5-50.3 ng/L) and 36.6 ng/L (range 7-163 ng/L), respectively. When used as a diagnostic tool, reported cut-off values for BNP or NT-proBNP vary according to presenting symptoms and age (Table 1), with levels affected by underlying conditions such as renal failure (increased levels), obesity (falsely low levels) and atrial fibrillation (higher than expected levels) (clinical feedback). Most authors agree that a cut-off level of 100 ng/L of BNP has a strong negative predictive value, ruling out a diagnosis of heart failure.3, 5 Although BNP and NT-proBNP are secreted in equi-molar proportions, the half-life of BNP is short (20 minutes) compared to NT-proBNP (120 minutes), therefore NT-proBNP is more often used for diagnostic purposes. In addition, the two peptides are cleared from the circulation using different pathways, with NTproBNP cleared via renal excretion only and BNP cleared using a combination of BNP to monitor and guide treatment of heart failure patients: August 2012 2 receptors, renal excretion as well as neutral endopeptidases (NEP).4, 6 In its current form, a BNP test acts as a tool to triage patients presenting to emergency departments. BNP testing is designed to rule out, rather than rule in, patients with HF. Patients testing positive for BNP, and therefore possibly HF, will undergo further diagnostic workup.7 A BNP value of <100 ng/L has a 96 per cent probability of excluding the diagnosis of HF, however, it is unlikely that BNP would be used to triage all patients, just those in whom a clinical diagnosis of HF is uncertain. 8 Table 1 Cut-off values for the diagnosis of heart failure using BNP or NT-proBNP Rule out: HF unlikely Rule in: HF likely BNP (ng/L) 100 500 NT-proBNP (ng/L), age <50 years* 300 450 NT-proBNP (ng/L), age >50 years* 300 900 NT-proBNP (ng/L), age <75 years** 125 NT-proBNP (ng/L), age >75 years** 450 * In patients presenting with dyspnoea (Weber and Hamm, 2006), ** Rademaker et al (2005) The level of BNP or NT-proBNP in the plasma directly relates to the severity of HF symptoms and is often associated with a worse patient prognosis. As described in Figure 1, increasing levels of BNP correlate with disease severity as assessed by the New York Heart Association (NYHA) functional class1.5 BNP has been demonstrated to be a strong predictor of cardiovascular and all-cause mortality. As such, levels of BNP may act as a prognostic tool that is independent of, and more accurate than, NYHA class and left ventricular eject fraction (LVEF).3, 4 Figure 1 1 Median BNP in patients with heart failure according to New York Heart Association (NYHA) functional status criteria (Weber and Hamm, 2006) See comparator section BNP to monitor and guide treatment of heart failure patients: August 2012 3 In addition to being used for the diagnosis and prognosis of HF patients, the cardiac peptides may also be beneficial in the treatment of certain HF patients with symptoms featuring volume overload and vasoconstriction. Two approaches have been used in the treatment of HF patients with BNP: administration of synthetic BNP or the use of NEP inhibitors, which increases the levels of endogenous BNPs by blocking their enzymatic breakdown.3 In June 2004, HealthPACT completed a report on the use of pro-BNP for the diagnosis of congestive heart failure9. MSAC conducted a full HTA on the use of BNP, Part A of which, the use of BNP in the hospital emergency setting, was finalised in November 2006 with the MSAC recommended public funding for this indication. Part B of which, the use of BNP assays in the diagnosis and monitoring of heart failure in the primary care setting, was finalised in May 2007, with public funding not supported by the MSAC. In the case of Part B, the MSAC recommended further research to identify appropriate usage and the patient group most likely to benefit in the non-hospital setting.7 Although a number of studies were identified that documented the use of BNP to monitor heart failure patients placed on pharmaceutical interventions, none of these studies reported on direct patient benefits, such as increased survival. Only two studies were identified for inclusion in the assessment of monitoring heart failure (HF) patients, one of which was a welldesigned, albeit small (n=69), randomised controlled trial conducted in New Zealand.10 This landmark trial reported that monitoring HF patients using a NTproBNP assay resulted in fewer cardiovascular deaths and total cardiovascular events than HF patients monitored using clinical criteria alone. Since the publication of the MSAC report, a number of studies have described the use of BNP testing to monitor the efficacy of treatment for HF patients. Pharmacological therapy for HF patients usually involves a combination of diuretics, β-blockers and ACE2 inhibitors. High doses of diuretics may impact negatively on renal function; however, a failure to remove fluid may result in recurrent congestion and re-hospitalisation. Therefore, the clinical goal for HF treatment is to reduce or resolve congestion while minimising hypotension and renal dysfunction.11 As a result of effective treatment of HF, a reduction in the circulating levels of natriuretic peptides will be observed, which in turn correlates with improvements in clinical symptoms and haemodynamic function, and with an associated reduction of morbidity and mortality. Persistently high levels of natriuretic peptides, despite appropriate treatment, are indicative of patients who are at high-risk of adverse outcomes. It has been postulated that regular, serial measurements of BNP may be 2 ACE inhibitors = angiotensin-converting enzyme inhibitors block the angiotensin pathway, increasing vasodilation and in so doing decreases arterial pressure. In addition, the excretion of sodium and water via the kidneys is increased, reducing blood volume, and venous and arterial pressure. BNP to monitor and guide treatment of heart failure patients: August 2012 4 used as a tool to guide HF therapy, in particular, using BNP measurements as a guide to achieving optimal pharmacotherapy by titrating therapies.3 By optimising therapy, it is hoped that the number of re-hospitalisations of HF failure patients will be reduced, further reducing overall costs associated with HF. The measurement of NTproBNP should be used in patients where synthetic BNP is being administered as a treatment option.3 Although there are several BNP/NT-proBNP assays on the market, they are all essentially in vitro immunoassays, designed to be used on plasma, serum or whole blood. Most commercial assays use the basic principle of using antibodies to bind to BNP or NT-proBNP, followed by a detection step. The RAMP ® NT-proBNP assay, manufactured by Response Biomedical Corporation (Canada), can be used on whole blood and is a quantitative immunochromatographic assay, however this assay is not used in Australia. Test strips, impregnated with antibodies to NT-proBNP bound to fluorescent-dyed latex particles, are placed in the sample. Any NT-proBNP present will bind to this complex, emitting fluorescence proportional to its concentration. 12 Most BNP assays are designed to be used on plasma and are sandwich immunoassays. Two antibodies are used to bind to BNP, with one biotinylated antibody bound to streptavidin magnetic particles for detection. 13 Clinical Need and Burden of Disease Based on the 2007-08 national health survey, 277,800 Australians or 1.4 per cent of the population had self-reported HF failure or oedema, with females reporting higher disease prevalence (1.7%) than males (1.0%). Prevalence of HF increased with age from 2.6 to 8.2 per cent in people aged 55-64 and >75 years, respectively.14 Based on the 2004-05 National Aboriginal and Torres Strait Islander Health Survey, approximately one per cent, or 4,500, of indigenous Australians have HF: a prevalence rate that is 1.7 times higher than for non-indigenous Australians when adjusted for age. Differences in prevalence rates can also be observed in rural and remote areas, and between different socio-economic groups.1 In the year 2009-10 there were 45,004 and 4,054 public hospital separations for the principal diagnosis of heart failure (ICD-10 code I50) and cardiomyopathy (ICD-10 code I42), respectively. The majority of these separations were for congestive HF (36,158 or 80%) and dilated cardiomyopathy (1,865 or 46%). The average length of stay for cardiomyopathy and HF was five and seven days, respectively. The overwhelming majority of HF separations were for individuals aged over 70 years of age (36,054 or 80%), whereas 67 per cent of separations (2,718) for cardiomyopathy were in individuals aged ≥50 years.15 The number of public hospital separations for HF has remained steady over the past 10 years.14 BNP to monitor and guide treatment of heart failure patients: August 2012 5 In 2007, HF was the attributable cause of death in 4,055 individuals, however, due to the complex nature of the disease it was also listed as the underlying or associated cause of death in 19,967 cases. The majority of deaths (90%) occurred in people aged over 75 years. Over the past 20-years, the age-standardised death rate for heart failure has fallen markedly from 38 to 17 deaths per 100,000, however, this rate is much higher when heart failure and underlying and associated causes of death are taken into account (approximately 85.8 per 100,000).1, 14 The use of pharmaceutical agents may give an indication as to the number of patients who may progress to HF and, therefore require monitoring with BNP assays. ACE inhibitors may delay the development of symptomatic chronic HF in patients with asymptomatic left ventricular dysfunction and beta-blockers, when administered early post-myocardial infarction may reduce the subsequent development of chronic HF in patients with preserved ventricular function. In addition, other anti-hypertensive medications may reduce blood pressure and reduce the incidence of CHF.2 In Australia during 2007-08, 3.8 million patients filled in excess of 70 million PBS-subsidised prescriptions for medicines to prevent or treat cardiovascular disease, an increase of 8.2 per cent over the period 2004-05. During this period 838,427 patients had 5.8 million prescriptions for beta-blockers dispensed, 2 million patients filled 20.8 prescriptions for ACE inhibitors and 173,854 patients had 846,068 prescriptions dispensed for anti-hypertensive medication.14 In New Zealand there were 8,426 and 685 public hospital discharges for HF and cardiomyopathy, respectively, during the year 2009-10. The average length of stay was 18.6 days for HF patients compared to 5.6 days for those patients admitted with cardiomyopathy. Although numbers of female and male patients were similar, the average length of stay for females with HF was considerably longer than that for males (24.1 days vs 13.4 days). In the private system there were only eight separations for cardiomyopathy with an average length of stay of 11.2 days. Although there were only 132 separations in the private system for HF, the average length of stay was 146.4 days.16 In 2009, there were a total of 10,372 deaths from diseases of the circulatory system in New Zealand. Of these 170 were attributable to cardiomyopathy, with the majority of these deaths occurring in males (73.5%). Conversely, 293 deaths were attributable to HF, the majority of which occurred in females (66.9%).17 Diffusion of technology in Australia The use of BNP assays for the diagnosis of HF is in widespread use in Australia. It was difficult to ascertain the status of BNP testing in New Zealand due to each District Health Board having different schedules for diagnostic tests. BNP to monitor and guide treatment of heart failure patients: August 2012 6 In Australia during 2011, the number of services performed using the MBS item number 66830 to diagnose heart failure was 6,061, however, this is only indicative of the number of services provided in private, rather than public hospitals where it would be expected that the number of services would be much higher.18 Comparators Commonly used monitoring tools include clinical evaluation, which may involve functional capacity assessment; fluid status; cardiac rhythm; and circulating levels of urea, electrolytes and creatinine. Functional capacity may be measured by quality of life questionnaires, exercise tests such as the 6-minute walk or maximal exercise test, and peak VO2 consumption. Fluid states are measured by physical examination such as assessing body weight, blood pressure and jugular venous distension; and cardiac rhythm is assessed by an electrocardiogram.19 The severity of HF may be classified according to the New York Heart Association Classification (NYHA) system (Table 2). Table 2 Assessment of heart failure patients using the NYHA classification criteria Class New York Heart Association Classification I (mild) No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnoea II (mild) Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnoea. III (moderate) Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnoea. IV (severe) Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased. 5 Safety and Effectiveness Several randomised controlled trials (RCTs) reporting on the use of BNP or NTproBNP for guiding treatment of HF were identified for inclusion in this Brief,11, 20-22 however, two meta-analyses of RCTs were later identified via pearling of the references in these papers.23, 24 The meta-analysis by Felker et al (2009) included six studies, all of which, bar the STARBRITE trial11, were included in the meta-analysis of eight studies by Porapakkham et al (2010). Therefore, only the results from the latest meta-analysis will be reported here (level I intervention evidence). The STARBRITE3 trial was 3 In brief, the STARBRITE trial enrolled 137 patients admitted to hospital with acute HF, a LVEF ≤35% who were NYHA class III/IV on admission, randomised to usual care (n=69) or BNP guided care (n=68). Patients were placed on medication, including ACE inhibitors, β-blockers etc, according to their needs; however, only diuretic therapy was adjusted or titrated during follow-up visits. Diuretics were adjusted according to BNP levels in the BNP group or by clinical symptoms in the UC group. At 90 day follow-up, there was no significant difference in the number of days alive and not hospitalised (hazard ratio 0.72, 95% CI [0.41, 1.27], p=0.25) between the two groups. This may have been due to a BNP to monitor and guide treatment of heart failure patients: August 2012 7 excluded from this meta-analysis on the grounds that it was only reported in a single study. Two studies were included using results presented at conference meetings: the PRIMA4 and SIGNAL-HF5 studies. Characteristics of the individual studies are summarised in Table 4. Of the eight studies included in the meta-analysis, three would be considered small, with 20 to 36 patients in each arm. The majority of the remaining studies were medium to large sized RCTs (110 to 250 patients in each arm). In total, results from 1,726 patients were pooled for analysis. The results from all of the individual studies and the overall risk ratio are summarised in Table 3. Overall, the all-cause mortality was lower in patients whose post-discharge HF treatment was guided by the use of BNP compared to those patients who received usual care (RR= 0.76, 95% CI [0.63, 0.91], p=0.003). There was no significant heterogeneity between the trials, with a χ 2 value of 3.81 (p=0.80), however there was variation between the studies in respect to the type of assay used (BNP and NT-BNP), the cut-off values used and the medications used when treatment was guided by BNP. The TIME-CHF trial dominated the effect, contributing 49.6 per cent of the weight. Two trials, the TIMECHF and BATTLESCARRED trials, stratified randomisation by age, providing data on patients younger than 75 years or 75 years or older. A sub-group analysis found that all-cause mortality in patients <75 years with HF treatment guided by BNP testing was lower (RR= 0.52, 95% CI [0.33, 0.82], p=0.005) compared with patients treated with usual care (heterogeneity χ2 =0.57, p =0.45). There was no significant difference between the two groups when all-cause mortality was assessed for those aged >75 years (RR = 0.94, 95% CI [0.71, 1.25], p= 0.70, heterogeneity χ2 = 1.14, p =0.29). Only three studies provided data on all-cause hospitalisation. There was no significant difference between the intervention and usual care groups for this outcome (RR = 0.82, 95% CI [0.64, 1.05], p= 0.12). This analysis was dominated by the STARS-BNP study, which contributed 80.4 per cent of the weight. Similarly, there was no significant difference between the two groups for the outcome of survival free of any hospitalisation, however, this outcome was only reported by two studies (RR = 1.07, 95% CI [0.85, 1.34], p= 0.58). number of factors including small sample size, inadequate length of follow-up and the fact that only diuretic medication was adjusted in response to BNP measurements. 4 PRo-brain-natriuretic peptide guided therapy of chronic heart failure IMprove heart failure morbidity and mortality Study. Paper presented at: Annual Scientific Meeting of American College of Cardiology; March 29, 2009; Orlando, Florida. 5 SIGNAL-HF Study. Paper presented at the European Heart Failure Association Annual Meeting; June 1, 2009; Nice, France. BNP to monitor and guide treatment of heart failure patients: August 2012 8 Table 3 Summary of outcome measures comparing BNP-guided HF treatment to usual care All-cause mortality Risk ratio [95% CI] All-cause hospitalisation Risk ratio [95% CI] Troughton et al 0.16 [0.02, 1.20] 0.69 [0.31, 1.58] Beck-da-Silva et al 0.48 [0.05, 4.85] 0.48 [0.10, 2.32] Esteban et al 1.25 [0.37, 4.21] STARS-BNP 0.64 [0.26, 1.58] TIME-CHF 0.75 [0.58, 0.96] BATTLESCARRED 1.00 [0.45, 2.22] PRIMA 0.79 [0.57, 1.10] SIGNAL-HF 0.79 [0.22, 2.86] Overall 0.76 [0.63, 0.91] Survival free of hospitalisation Risk ratio [95% CI] 1.06 [0.69, 1.62] 0.87 [0.67, 1.12] 1.07 [0.82, 1.38] 0.82 [0.64, 1.05] 1.07 [0.85, 1.34] An informal analysis of two studies: the PRIMA and the excluded STARBRITE study, reported that the number of days patients were alive and not hospitalised was slightly higher in the BNP-guided treatment group compared to usual care, however this difference did not reach significance in either study (85 ± 12.1 (BNP) vs 80.4 ± 20.6 (UC) days and 685 (BNP) vs 664 (UC) days in the STARBRITE and PRIMA studies, respectively). The STARS-BNP and PRIMA studies reported the number of patients in whom medical treatment was adjusted (Figure 2A). Patients in the BNP-guided group had their medications adjusted more than those who received usual care, with the difference reaching significance for diuretics, ACE inhibitors and β-blockers. The STARS-BNP and TIME-CHF studies also reported that significantly more patients in the BNP group reached their target medication doses (Figure 2B). Figure 2 24 Medical treatment adjustment A: percentage of patients having doses of medication increased B: percentage change of patients reaching target dose BNP to monitor and guide treatment of heart failure patients: August 2012 9 Table 4 Patient characteristics and study overview of the included trials Troughton et 10 al Beck-da25 Silva Esteban et al 26 STARS-BNP 20 TIME-CHF 22 BATTLE 21 SCARRED PRIMA SIGNAL-HF Number of patients Intervention arm Usual care 33 36 21 20 30 30 110 110 251 248 121 121 174 171 126 124 Follow-up (months) 9.5 3 18 15 18 24 24 9 Mean age (years) ± SD Intervention arm Usual care 68 72 64.5 ± 15.2 65.6 ± 13.5 65 ± 5 66 ± 6 76 ± 7 77 ± 8 76 76 71 ± 12 73 ± 12 >18 >18 Mean NYHA functional class Intervention arm Usual care 2.3 2.3 2.6 2.4 NA NA 2.29 2.21 NA NA NA NA NA NA 2-4 2-4 Mean LVEF % ± SD Intervention arm Usual care 28 26 23.8 ± 8.8 20.9 ± 9.2 Similar in both groups 31.8 ± 8.4 29.9 ± 7.7 29.8 ± 7.7 29.4 ± 7.9 37 37 31 35 <50 <50 NT-proBNP BNP BNP BNP NT-proBNP NT-proBNP NT-proBNP NT-proBNP 1,844 2,133 502 702 NA NA 3,998 4,657 2,012 1,996 2,958 2,932 NT-proBNP <1700 ng/L β-blocker when BNP , or when BNP >10% lower than previous value, or BNP is within ± 10% previous level NA BNP <100 ng/L NYHA II plus NT-proBNP <400 ng/L (<75 years), <800 ng/L (>75 years) NT-proBNP <1300 ng/L Lowest level achieved 2weeks post HF BNP or NT-proBNP Mean baseline measurement of BNP or NT-proBNP (ng/L) Intervention arm Usual care Target for BNP guided therapy Similar in both groups Male >800 Female >1,000 5 BNP to monitor and guide treatment of heart failure patients: August 2012 10 Troughton et 10 al 5 Beck-da25 Silva Target for usual care HF score <2 on Framingham a score Clinical assessment Medical adjustment involved ACE inhibitors, diuretic, digoxin, aldactone, metolazone Only β-blocker Esteban et al 26 Framingham a score STARS-BNP 20 TIME-CHF 22 BATTLE 21 SCARRED PRIMA SIGNAL-HF Physical examination NYHA functional class <2 HF score <2 on Framingham a score Clinical assessment Clinical assessment β-blocker, ACE inhibitors, diuretic, aldactone β-blocker, ACE inhibitors, or ARB, diuretic, aldactone, nitrate β-blocker, ACE inhibitors, diuretic, aldactone, digoxin, metolazone β-blocker, ACE inhibitors, or ARB, diuretic, aldactone, digoxin β-blocker, ACE inhibitors, or ARB, aldactone NYHA = New York Heart Association functional class, NA = not available, LVEF = left ventricular ejection fraction, ARB = angiotensin receptor blocker a Framingham HF score: one point for each major criteria present, 0.5 point for each minor criteria present. Major criteria: paroxysmal nocturnal dyspnoea; neck vein distention; rales; radiographic cardiomegaly (increasing heart size on chest radiography); acute pulmonary oedema; S3 gallop; increased central venous pressure (>16 cm H2O at right atrium); hepatojugular reflux; weight loss >4.5 kg in 5 days in response to treatment. Minor criteria: bilateral ankle oedema; nocturnal cough; dyspnoea on ordinary exertion; hepatomegaly; pleural effusion; decrease in vital capacity by one third from maximum recorded; tachycardia (heart rate>120 beats/min.). BNP to monitor and guide treatment of heart failure patients: August 2012 11 Cost Impact A number of cost-effectiveness studies, including the 2007 MSAC report, were identified that reported on the use of BNP assays to diagnose HF in the emergency department setting. However, there was a dearth of literature on the use of these assays to monitor and guide therapy in HF patients. The 2007 MSAC assessment did report an indicative price of $50.59 for the performance and reporting of a single test, allowing for a 17 per cent profit and no co-payment. This figure was based on the purchase of a 100 test kit at a cost of $2,187.50, and a scenario of conducting 10specimens per run, seven days a week. Laboratory costs including salaries, assets and overheads were included in this estimate. The current fee for MBS item number 66830 is $58.90. The current list price for the AxSYM® BNP assay is $3,756.55 for a test kit for 100 specimens. It is estimated that this cost would be reduced to $2,000, and therefore $20 per sample, when purchased in bulk. However, this price would not take into account the cost of performing and reporting on the assay (personal communication Abbott Diagnostics Australia). Roche Diagnostics were contacted regarding the current cost of the Elecsys® proBNP kit, however no reply was received. Cardiovascular disease accounts for approximately 11 per cent of Australia’s health care budget, with chronic heart failure estimated to presently cost one billion dollars. The current cost of hospitalised patients in acute beds is $1,100/day compared to $550/day for subacute stays.27 By using BNP measurements to optimise therapy it is hoped that the number of re-hospitalisations of HF failure patients will decrease, further reducing overall costs associated with HF. Only one cost-effectiveness analysis, conducted in Austria, was identified for inclusion in this Brief.28 Although 278 patients with HF6 were randomised to receive either usual care, home-based nurse care (HNC) or HNC plus decision-making based on NT-proBNP levels (BNC), only 190 fulfilled the criteria for a per-protocol analysis. There was no difference between the treatment groups in age, sex, HF medication and ventricular function at discharge. HNC and BNC patients participated in two outpatient clinics 10 days and 2-months post-discharge, in addition to receiving four home visits by a HF nurse at 1, 3, 6 and 12-months. Patients in the BNC group had a NT-proBNP test during these visits and those patients with a NT-proBNP level >2200 ng/L -1 received a visit to a HF-outpatient clinic. The price for one determination of NT-proBNP was €25.85, which currently converts to A$31.74, considerably less than the $50.59 used in the MSAC report. Re-hospitalisation was estimated to cost €388 (A$476) per bed per night. Home visits by a HF nurse were estimated to cost €80 and 6 NYHA class III or IV, LVEF <40% and cardiothoracic ration >0.5 BNP to monitor and guide treatment of heart failure patients: August 2012 12 a 15 minute outpatient appointment with a cardiologist was estimated to cost €15.15. The clinical outcomes for these patients are summarised in Table 5. Death or rehospitalisation was significantly lower in patients who received home-based nurse care with or without BNP testing, however fewer patients experienced this outcome in the BNC group (37%, p= 0.001). Mortality rates were also significantly lower in the HNC and BNC groups compared to usual care. Table 5 Clinical outcomes for patients included in the economic analysis Outcome 28 Usual care (n=47) Homebased nurse care (n=85) Homebased nurse care + BNC (n=58) Death or re-hospitalisation for HF 66% 53% 37% Overall UC vs HNC: HNC vs BNC: UC vs BNC: 0.002 0.012 0.311 0.001 Mortality 45% 24% 17% Overall UC vs HNC: HNC vs BNC: UC vs BNC: 0.004 0.002 0.533 0.017 Re-hospitalised for any cause 83% 75% 65% Overall UC vs HNC: HNC vs BNC: UC vs BNC: 0.115 0.095 0.698 0.052 Re-hospitalised for HF 60% 41% 25% Overall UC vs HNC: HNC vs BNC: UC vs BNC: <0.001 0.014 0.012 <0.001 P-value Per patient costs for hospitalisation due to worsening heart failure were significantly less for patients in the BNC group compared to usual care (€2991 vs €7109, p=0.027). However, it should be noted that the high standard deviation in all care groups indicates a great deal of variation within the groups (Table 6). Costs in the BNC group were also significantly less than those for the HNC group (p= 0.033). Although costs increased marginally in both groups when corrected for death as a competing risk, costs remained significantly less in the BNC group compared to usual care (€3148 vs €7893, p= 0.012). Differences between costs in the HNC and BNC groups were also significant (p=0.016). When the costs for all cause re-hospitalisations per year survived after discharge were calculated, BNC was found to be more cost-effective than usual care (€8787 vs €19694, p = 0.015), again with high standard deviations in all groups indicating a great deal of variation. The cost-effectiveness ratio of HNC and BNC compared to usual care was €0.83 and €24.85, respectively, indicating that both care groups cost less and result in longer survival times. In all models HNC was cost neutral and NT-proBNP testing in addition to HNC was found to be cost-effective and cheaper than usual care.28 Although this study was limited by the relatively small BNP to monitor and guide treatment of heart failure patients: August 2012 13 number of patients in each group, it was considered unlikely that the results would be biased towards the BNC group. Table 6 Costs for clinical outcomes 28 Costs Usual care Home-based nurse care Home-based nurse care + BNC Including all-cause re-hospitalisations €12,450 ± 16,185 €12,391 ± 16,641 €9,674 ± 11,309 Including all-cause re-hospitalisations correcting for death as a competing risk €14,737 ± 16,064 €13,828 ± 16,757 €10,235 ± 11,439 Including only hospitalisation due to worsening HF €7,109 ± 11,687 €5,225 ± 7,508 €2,991 ± 4,885 Including only hospitalisation due to worsening HF correcting for death as a competing risk €7,893 ± 11,734 €5,740 ± 7,787 €3,148 ± 4,949 Considering all-cause re-hospitalisations €19,694 ± 26,754 €14,262 ± 25,330 €8,787 ± 14,728 Considering re-hospitalisation due to congestive HF €15,151 ± 26,791 €7,084 ± 17,170 €3,978 ± 13,261 Cost-effectiveness Ethical, Cultural or Religious Considerations No issues were identified/raised in the sources examined. Other Issues The RCT conducted in New Zealand by Lainchbury et al (2009), The BNP Assisted Treatment to Lessen Serial Cardiac Readmissions and Death, appears to be ongoing. The 2009 study reported on 364 HF patients randomised to therapy guided by NTproBNP levels, intensive clinical management or usual care. When registered on the Australian New Zealand Clinical Trials Registry (ACTRN12605000735651) this trial aimed to recruit 1,000 HF patients. Summary of Findings Levels of BNP and NT-proBNP are elevated in heart failure patients, with increasing levels correlating with an increased severity of symptoms. BNP and NT-proBNP assays are currently approved by the MBS for the diagnosis of heart failure, however insufficient evidence was available for the use of BNP to monitor the treatment of heart failure patients when this indication was assessed by the MSAC in 2007. Since 2007, several medium to large RCTs have been published, with total enrolments ranging from 220 to 499 heart failure patients. These studies, plus the results of two studies presented at conferences, were included in a meta-analysis of BNP-guided treatment of HF patients compared to usual care. All-cause mortality was lower in patients whose post-discharge HF treatment was guided by the use of BNP compared to those patients who received usual care (RR= 0.76, p=0.003). A subBNP to monitor and guide treatment of heart failure patients: August 2012 14 group analysis found that all-cause mortality in patients <75 years with HF treatment guided by BNP testing was lower (RR= 0.52, p=0.005) compared to patients treated with usual care, a difference that was absent in those aged >75 years (RR = 0.94, p= 0.70). There was no significant difference between the intervention and usual care groups for the outcome of all-cause hospitalisation (RR = 0.82, p= 0.12) or for survival free of any hospitalisation (RR = 1.07, p= 0.58). However, these last three outcomes were not reported by all studies. The one cost-effectiveness analysis included for assessment was relatively small but concluded that BNP-guided treatment of heart failure patients was found to be more cost-effective than usual care. It is unclear if the results of this Austrian analysis would be generalisable to Australia or New Zealand, however base costs were similar, albeit lower, to those used in the Australian health system. HealthPACT Assessment: Anecdotal evidence suggests the MBS item number that describes the use of BNP tests for the diagnosis of heart failure is being used “off-label” to monitor the treatment of heart failure patients. Since the publication of the 2007 MSAC assessment a wealth of good quality RCTs have been published that describe the use of BNP or NT-proBNP assays to monitor therapy in heart failure patients. In addition, an on-going New Zealand study is currently being conducted that intends to enrol the largest patient group to date and offers the potential for a cost-effectiveness analysis being conducted that is relevant to the Australasian health system. HealthPACT have recommended that jurisdictional data on the use of the BNP MBS item number be collated and that this information be brought to the attention of the Medical Benefits Branch with a view that a full health technology assessment be conducted. Number of Studies included All evidence included for assessment in this Technology Brief has been assessed according to the revised NHMRC levels of evidence. A document summarising these levels may be accessed via the following link on the HealthPACT web site. Total number of studies Total number of Level I intervention studies 1 1: a meta-analysis of 8 RCTs (level II intervention studies) References 1. 2. AIHW (2011). Cardiovascular disease: Australian facts 2011, Australian Institute of Health and Welfare, Canberra http://www.aihw.gov.au/publication-detail/?id=10737418510&tab=2. Chronic Heart Failure Guidelines Expert Writing Panel (2006). Guidelines for the prevention, detection and management of chronic heart failure in BNP to monitor and guide treatment of heart failure patients: August 2012 15 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Australia, 2006, National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand http://www.heartfoundation.org.au/SiteCollectionDocuments/CHF%202006 %20Guidelines%20NHFA-CSANZ%20WEB.pdf. Rademaker, M. T.&Richards, A. M. (2005). 'Cardiac natriuretic peptides for cardiac health'. Clinical Science, 108 (1), 23-36. Tang, W. H. (2007). 'B-type natriuretic peptide: a critical review'. Congestive heart failure (Greenwich, Conn), 13 (1), 48-52. Weber, M.&Hamm, C. (2006). 'Role of B-type natriuretic peptide (BNP) and NT-proBNP in clinical routine'. Heart, 92 (6), 843-9. Gassanov, N., Biesenbach, E.et al (2012). 'Natriuretic peptides in therapy for decompensated heart failure'. European Journal of Clinical Pharmacology, 68 (3), 223-30. Merlin, T., Moss, J.et al (2007). Brain natriuretic peptide assays in the diagnosis and monitoring of heart failure, Medical Services Advisory Committee, Canberra. Report No.: 1087 http://www.msac.gov.au/internet/msac/publishing.nsf/Content/2CDBC3816 FDE8D20CA2575AD0082FD8E/$File/1087%20-%20Carbonlabelled%20urea%20breath%20tests%20Report.pdf. Beck-da-Silva, L., Rohde, L. E.et al (2007). 'Clinical findings, natriuretic peptides, and echocardiography: integrating tools to optimize heart failure management'. Congestive heart failure (Greenwich, Conn), 13 (3), 158-63. Bywood, P., Merlin, T.et al (2004). Horizon Scanning Report: Pro-BNP for the diagnosis of congestive heart failure, HealthPACT, Canberra http://www.horizonscanning.gov.au/internet/horizon/publishing.nsf/Content /58685F8B48CC9EE7CA2575AD0080F340/$File/elecsys.pdf. Troughton, R. W., Frampton, C. M.et al (2000). 'Treatment of heart failure guided by plasma aminoterminal brain natriuretic peptide (N-BNP) concentrations'. Lancet, 355 (9210), 1126-30. Shah, M. R., Califf, R. M.et al (2011). 'The STARBRITE trial: a randomized, pilot study of B-type natriuretic peptide-guided therapy in patients with advanced heart failure'. J Card Fail, 17 (8), 613-21. FDA (2008). 510(k) Summary of Safety and Effectiveness RAMP NT-proBNP Assay. [Internet]. Food and Drug Administration. Available from: http://www.accessdata.fda.gov/cdrh_docs/pdf6/K063662.pdf?utm_campaig n=Google2&utm_source=fdaSearch&utm_medium=website&utm_term=Brai n%20natriuretic%20peptide%20assay&utm_content=4 [Accessed 27th June 2012]. FDA (2003). 510(k) Summary of Safety and Effectiveness ADVIA Centaur@B Type Natriuretic Peptide (BNP) Assay. [Internet]. Food and Drug Administration. Available from: http://www.accessdata.fda.gov/cdrh_docs/pdf3/k031038.pdf [Accessed 27th June 2012]. AIHW (2010). Australia’s health 2010, Australian Institute of Health and Welfare, Canberra http://www.aihw.gov.au/publications/aus/ah10/ah10.pdf. Separation statistics by principal diagnosis in ICD-10-AM, Australia, 2008-09 to 2009-10 [database on the Internet]. Australian Institute of Health and BNP to monitor and guide treatment of heart failure patients: August 2012 16 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. Welfare. 2012 [cited 26th June 2012]. Available from: http://www.aihw.gov.au/hospitals-data-cube/?id=10737419429. Ministry of Health (2012). Hospital event data and stats. [Internet]. New Zealand Ministry of Health. Available from: http://www.health.govt.nz/nzhealth-statistics/health-statistics-and-data-sets/hospital-event-data-and-stats [Accessed 26th June 2012]. Ministry of Health (2012). Mortality and Demographic Data 2009. [Internet]. New Zealand Ministry of Health. Available from: http://www.health.govt.nz/publication/mortality-and-demographic-data2009 [Accessed 27th June 2012]. MBS Item Statistics Reports [database on the Internet]. Australian Government. 2012 [cited 26th June 2012]. Available from: https://www.medicareaustralia.gov.au/statistics/mbs_item.shtml. NICE (2010). Chronic heart failure: Management of chronic heart failure in adults in primary and secondary care, National Institute for Health and Clinical Excellence http://www.nice.org.uk/nicemedia/live/13099/50517/50517.pdf. Jourdain, P., Jondeau, G.et al (2007). 'Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP Multicenter Study'. J Am Coll Cardiol, 49 (16), 1733-9. Lainchbury, J. G., Troughton, R. W.et al (2009). 'N-terminal pro-B-type natriuretic peptide-guided treatment for chronic heart failure: results from the BATTLESCARRED (NT-proBNP-Assisted Treatment To Lessen Serial Cardiac Readmissions and Death) trial'. J Am Coll Cardiol, 55 (1), 53-60. Pfisterer, M., Buser, P.et al (2009). 'BNP-guided vs symptom-guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial'. JAMA, 301 (4), 383-92. Felker, G. M., Hasselblad, V.et al (2009). 'Biomarker-guided therapy in chronic heart failure: a meta-analysis of randomized controlled trials'. Am Heart J, 158 (3), 422-30. Porapakkham, P., Zimmet, H.et al (2010). 'B-type natriuretic peptide-guided heart failure therapy: A meta-analysis'. Arch Intern Med, 170 (6), 507-14. Beck-da-Silva, L., de Bold, A.et al (2005). 'BNP-guided therapy not better than expert's clinical assessment for beta-blocker titration in patients with heart failure'. Congest Heart Fail, 11 (5), 248-53; quiz 54-5. Esteban, F., Anguita, M.&Castillo, J. (2006). 'BNP levels guided therapy for heart failure: a comparative study against usual clinical monitoring'. Eur Heart J, Suppl (1416). Betihavas, V., Newton, P. J.et al (2011). 'Australia's health care reform agenda: implications for the nurses' role in chronic heart failure management'. Aust Crit Care, 24 (3), 189-97. Adlbrecht, C., Huelsmann, M.et al (2011). 'Cost analysis and costeffectiveness of NT-proBNP-guided heart failure specialist care in addition to home-based nurse care'. Eur J Clin Invest, 41 (3), 315-22. Search Criteria to be used (MeSH Terms) Biological Markers/blood BNP to monitor and guide treatment of heart failure patients: August 2012 17 Heart Failure/diagnosis Heart Failure/drug therapy* Monitoring, Physiologic Natriuretic Peptide, Brain/blood* BNP to monitor and guide treatment of heart failure patients: August 2012 18