* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Diagnosing Heart Failure (HF)
Remote ischemic conditioning wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Cardiac surgery wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Heart arrhythmia wikipedia , lookup
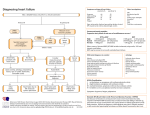
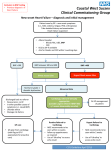
Diagnosing Heart Failure (HF)1 Perform ECG and baseline bloods (FBC, LFTS and renal function as minimal set) Heart Failure (HF) is a clinical syndrome typified by the following criteria: symptoms of HF (SOB at rest or on exercise, fatigue, tiredness, SOA) and signs of HF (tachycardia, tachypnoea, pulmonary rales, pleural effusion, raised JVP, peripheral oedema, hepatomegaly) and objective evidence of a structural or functional abnormality of the heart at rest (eg abnormality on the echocardiogram) Brain natriuretic peptide (BNP) and NT-Pro BNP This is a polypeptide secreted by the ventricles of the heart in response to stretch. It is a validated tool to aid in the diagnosis of HF. A normal BNP level suggests that HF is very unlikely (<5%) and is a good rule-out test. A raised BNP level can be due to HF amongst other causes. The BNP level does not differentiate between HF due to left ventricular systolic dysfunction and HF with preserved ejection fraction (see below). Do not perform BNP in patients with known HF or previous MI. Very useful in diagnosis of HFPEF or HFmREF Serum NT Pro-BNP tested in Dorset Expensive test: do not use as breathlessness screen! High > 2000 ng/l Raised 400-2000 ng/l Normal < 400 ng/l (236pmol/l) (47-36pmol/l) (47pmol/l) Other investigations: CXR TFT Fasting sugar and lipids Urinalysis Peak flow or spirometry Other causes of elevated BNP/NT-BNP include AF, ischaemia, tachycardia, LVH and renal failure. BNP may be normal in very well treated HF and also with ischaemic heart disease leading to SOB References: 1NICE Chronic Heart Failure; Management of chronic heart failure in adults in primary and secondary care August 2010, NICE Cardiac Resynchronisation Therapy 2007; Map of Medicine. http://www.nice.org.uk/nicemedia/live/13099/50526/50526.pdf 2Ponikowski P et al. ESC Guidelines for HF management. Eur Heart J 2016. Created by Dr C Boos, Consultant Cardiologist Poole Hospital; [email protected]; Version 4; 02-08-2016 Differential diagnoses to consider: Aetiology of HF Obesity and / or sleep apnoea Chest disease including COPD Venous insufficiency lower limbs Drug induced ankle swelling eg Ca channel blockers Drug induced fluid retention eg NSAIDs Hypoalbuminaemia, Renal or hepatic disease Pulmonary embolism Depression and/or anxiety Severe anaemia, and /or thyroid disease Ischaemic heart disease Hypertension Valvular disease Dilated cardiomyopathy Hypertrophic cardiomyopathy Pulmonary disease Alcohol Chemotherapy Tachycardiomyopathy etc NYHA Classification I no limitations, no symptoms with ordinary physical activity II slight limitation, symptoms with ordinary activity III marked limitation, symptoms with less than ordinary activity IV breathless at rest, any physical activity increases symptoms Heart Failure with Preserved Ejection fraction (HFPEF) of so called Diastolic HF (EF>50%) This is due to abnormal relaxation of the left ventricle in diastole. Hence normal LV systolic function and ejection fraction could still be HF.! Only consider if BNP is elevated. Typical patient is elderly, hypertensive (♀>♂). Difficult to diagnose, echocardiogram may show ‘diastolic markers’ and left ventricular hypertrophy ± left atrial dilatation. Functional: Mean E/e′ ≥13 and a mean e’ septal+lateral wall <9 cm/s on echocardiogram2. Heart Failure with mid-range ejection fraction HFmREF as above but EF 40-49% New term (ESC 2016) to represent a subgroup of HF-PEF Drug Treatment for Heart Failure Due to LVSD Diuretics use loop diuretic if congestion eg frusemide 40mg and uptitrate ACE inhibitors Start low and titrate upwards at intervals of every 2 weeks Measure urea, creatinine and electrolytes with each dosage increment Up-titration to be limited by symptomatic low blood pressure and renal function only if creatinine increases by > 50% or to > 200mmol/l. Beta-blockers ‘Start low and go slow’, dosage increments every 2-4 weeks Monitor HR, BP and clinical status after each titration Warn patients that they may experience transient mild symptomatic deterioration but should improve with continued treatment Switch stable patients on B for co-morbidty to a B licensed for HF (eg bisoprolol), Up-titration to be limited by symptomatic low blood pressure or by bradycardia (if symptomatic or HR < 50/minute) Most patients with COPD without reversibility will tolerate Effective and safe in elderly, PVD, DM, erectile dysfunction Aldosterone antagonists (spironolactone 1st line; eplerenone second line) if symptomatic in spite of optimised treatment esp in NYHA II-IV and EF <35% Monitor renal profile at 1w, 1m and every 6m if on ACEI/ARB ARBs Consider as alternative to ACEI if intolerant Not in addition to ACE-I ARNI angiotensin receptor neprilysin inhibitor – Entresto* (HF Specialist use) Consider in NYHA II-IV HFREF instead of ACE-I o/ARB if deteriorating 48h wash out on conversion from ACE-I; avoid if SBP <100mmHg (*contains valsartan) If-channel blocker - Ivabradine (Pure HR lowering drug) Consider in patients with HR >75/minute, in sinus rhythm and BB intolerant or on max tolerated BB dose if still symptomatic (aim HR 50-60/minute); contraindicated in AF Digoxin Usual dosage 125mcg; no need to monitor levels Aspirin use only if other indication eg CHD/PVD Not improving 1. ECG (AF/LBBB) 2. Hb and Iron status and consider Iron replacement (note can be iron deficient and not anaemic) Transferrin sat <20% +/ferritin <100 mg/L. 3. TFTs 4. Drug compliance 5. Sleep disordered breathing? Digoxin od if EF <45% or AF and Ivabradine bd if EF<35% and HR >75/minute in sinus rhythm Target doses Bisoprolol 10mg od Ramipril 10mg/day Candesartan 32 mg daily Ivabradine 7.5mg/bd Consider Entresto ARNI Lifestyle advice Exercise: encourage regular exercise within capabilities; HF rehab NYHA I-III Diet: encourage low salt diet Smoking: strongly advise not to smoke Alcohol: abstain in those with alcohol related HF Sexual activity: be prepared to discuss Vaccination: offer annual vaccination against influenza and one-off vaccination against pneumococcus Driving: consult DVLA guidelines HF nurse Strongly consider referral to help with HF dose titrations and education etc CRT (resynchronisation pacing +/- ICD) * Broad QRS and low EF = HIGH risk* It should be considered in pts with: QRS > 130ms (>150ms without LBBB) LVEF ≤35% Symptomatic HF despite good treatment Refer to a HF specialist for treatment optimisation and consideration of device therapy. NB. CRT without ICD is relatively cheap and has significant short term symptom benefit as well as mortality benefit, often appropriate in the elderly. Check QRS duration. ICD generally not recommended within 40/7 of MI Palliative Care NYHA IV in spite of optimal Rx Clinician would not be surprised if patient died within 12 months Discuss CPR Consider referral to palliative care team Consider advanced care and treatment escalation plans Drugs to avoid NSAIDs CCBs except amlodipine Erythromycin, Tricyclics Other drugs that prolong QT Steroids, Lithium Class I antiarrhythmics Glitazones Some others! Nebivolol 10mg daily Enalapril 20mg bd Spironolactone 50mg od Digoxin 125-250mcg od Carvedilol 25-50mg bd Lisinopril 25-35mg od Eplerenone 50mg od Entresto 97/103mg bd Monitoring Monitor all patients. Include: Clinical assessment of functional capacity, cardiac rhythm, cognitive, fluid and nutritional status Re-iterate lifestyle advice especially diet, exercise, smoking Review of drug treatment include need to change and monitoring for side ffects Minimum of urea, electrolytes, creatinine, eGFR Monitor at short intervals (days to 2 weeks) if clinical condition or drug treatment has changed, otherwise monitor at least 6 monthly. HF-PEF and HFmREF Manage fluid retention with diuretics Treat the cause Currently no trial evidence for ACEIs or beta blockers but important to consider their use particularly with HFmREF If AF, consider adding digoxin for rate control Treat co-morbidities esp. hypertension