* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Electrocardiography
Heart failure wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
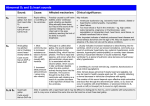
Atrial fibrillation wikipedia , lookup
Electrocardiography (ECG) An Overview of the Cardiovascular System The Heart Valves of the Heart (1) Valves of the Heart (2) Cardiac Conduction System Cardiac Conduction System • The sinoatrial (SA) node, located in the wall of the right atrium. • The atrioventricular (AV) node, located at the junction between the atria and ventricles. • Conducting cells interconnect the two nodes and distributethe contractile stimulus throughout the myocardium. In the atria, conducting cells are found in internodal pathways, which distribute the contractile stimulus to atrial muscle cells as this electrical impulse travels from the SA node to the AV node. (The importance of these pathways in relaying the signal to the AV node remains in dispute, because an impulse can also spread from contractile cell to contractile cell, reaching the AV node at about the same time as an impulse that travels an internodal pathway.) In the ventricles, conducting cells include those in the AV bundle and the bundle branches, as well as the Purkinje( ) fibers, which distribute the stimulus to the ventricular myocardium. Impulse Conduction through the Heart Sinoatrial Node and Ventricular Muscle Fibre Action Potentials Sinoatrial (SA) node fibres possess the ability to depolarize spontaneously until a threshold potential of about -40 mV is reached, which generates a new action potential . These pacemaker action potentials spread to working myocardial fibers, resulting in working myocardium action potentials. In the ventricle, a working myocardium action potential begins with a rapid reversal of the myocardial cell membrane potential, from a resting potential of about -90 mV to the initial peak of about +20 mV. Ten Electrode Locations for a Standard 12-lead Electrocardiogram • • • • • • • • • • LA: left arm RA: right arm LL: left leg RL: right leg V1: Fourth intercostal (between the ribs) space, right of sternum (breastbone) V2: Fourth intercostal space, left of sternum. V4: Fifth intercostal space, in the same vertical line as the clavicle (collarbone) V3: Midway between V2 and V4 V6: Fifth intercostal space, in same vertical line as armpit fold V5: Between V4 and V6 Limb Leads • Lead I = LA - RA • Lead II = LL - RA • Lead III = LL - LA Lead III=Lead II - Lead I RL is connected to ground. Vw = (RA+LA+LL)/3 Vw: Wilson's central terminal is the average of the three limb leads. This approximates common, or average, potential over the body Augmented Limb Leads • Augmented voltage right (AVR) AVR = RA - (LA+LL)/2 = 3(RA-Vw)/2 = -(I+II)/2 • Augmented voltage left (AVL) AVL = LA - (RA+LL)/2 = 3(LA-Vw)/2 = I-II/2 • Augmented voltage foot (AVF) AVF = LL - (LA+RA)/2 = 3(LL-Vw)/2 = II-I/2 Chest Leads (Precordial Leads) V1, V2, V3, V4, V5 and V6 are placed directly on the chest. Wilson's central terminal is used for the negative electrode, and these leads are considered to be unipolar Electrocardiograph (ECG) An Electrocardiogram An Electrocardiogram • The small P wave, which accompanies the depolarization of the atria. The atria begin contracting about 25 msec after the start of the P wave. • The QRS complex, which appears as the ventricles depolarize. This electrical signal is relatively strong, because the ventricular muscle is much more massive than that of the atria. It is also a complex signal, largely because of the complex pathway that the spread of depolarization takes through the ventricles. The ventricles begin contracting shortly after the peak of the R wave. • The smaller T wave, which indicates ventricular repolarization. Atrial repolarization is not apparent, because it takes place while the ventricles are depolarizing, and the QRS complex masks the electrical events. Cardiac Muscle Polarization and ECG Standard ECG Grid RR interval ~ 5 division = 1000ms -> 60 bpm Normal ECG Recordings from the 12 Surface Leads Electrocardiograph System Diagram Key Features • Input Dynamic Range – display ± 5 mV to ± 10 mV at a signal varying rate within 320 mV/sec. – direct current offset voltage ±300 mV. • Frequency Response A general rule of thumb is to preserve 30 harmonics. For example, a heartbeat of 60 bpm sampling rate is 60 Hz , a heartbeat of 100 bpm, sampling rate is 120 Hz • System Noise Not exceed 30 μV p-p over a 10-s period (The special circuit consists of a 51-kΩ resistor in parallel with a 47-nF capacitor, in series with each patient-electrode connection (AAMI, 2007)). • Arrhythmia Detection – The FDA recommends that ANSI/AAMI EC57:2003 Testing and Reporting Performance Results of Cardiac Rhythm and ST Segment Measurement Algorithms (AAMI, 2003) be followed. • Leads-Off Detection – Less than 1 μA of current is transmitted to various pairs of patient electrodes in order to determine whether each electrode is properly connected to the patient. If an open circuit is detected, an alarm monitor sounds (AAMI, 2002). Cardiac Arrhythmias • A heart rate lower than 60 bpm is referred to as sinus bradycardia. • A heart rate higher than 100 bpm is referred to as sinus tachycardia. • Arrhythmias can be categorized into five classes: 1. Escape. 2. Irregular rhythms. 3. Premature beats. 4. Tachyarrhythmias. 5. Heart blocks. Escape (1) A potential pacemaker may replace a failing SA node. These potential pacemakers in cardiac tissue are known as ectopic foci. Escape arrhythmia refers to the ability of an ectopic focus to “escape” overdrive suppression and pace at its inherent rate, according to a physiologic hierarchy. The fastest available pacemaker paces and suppresses slower pacemaking activities, in what is known as overdrive suppression. - If the SA node fail, an atrial focus begins to pace at an inherent rate of 60-80 bpm (Atrial escape: normal P morphology is lost. - If atrial foci fail to pace, an AV junctional focus begins to pace at an inherent rate of 40-60 bpm (Junctional escape a normal P wave is not seen, may occasionally see a retrograde P wave). The AV junction is the portion of the AV node possessing ectopic foci. - If AV junctional foci fail to pace, a ventricular focus paces at an inherent rate of 20-40 bpm (Ventricular escape: no P wave, wide, abnormal QRS). Ventricular foci are composed of Purkinje cells within the Purkinje fibers. Escape (2) A: Sinus rhythm, followed by atrial escape beats (printed with Rivertek RSIM). B: Sinus beat, followed by a junctional escape beat and then a junctional escape beat with retrograde (invertyed) P wave superimposed on the T wave C: Ventricular escape rhythm, enormous ventricular complexes, without P waves Irregular Rhythms A:Wandering pacemaker. occurs when pacemaker activity “wanders” from the SA node to nearby atrial ectopic foci. This results in rate variation within the normal range and a shape variation in the P wave. B:Multifocal atrial tachycardia. multifocal atrial tachycardia (MAT). Now the rate is greater than 100 bpm, and the P-wave shape varies greatly, as three or more atrial foci pace. C: Atrial fibrillation. When multiple atrial ectopic foci continuously fire, complete depolarization of the atria may be prevented, with only occasional depolarization through the AV node to stimulate the ventricles. Atrial fibrillation (Afib) is present—chaotic atrial spikes and irregular ventricular rhythm. References 1. 2. 3. 4. Fundamental of Anatomy and Physiology, Frederic H. Martini Biomedical Instrumentation: Application and Design, John G. Webster Medical Device Technologies: A Systems Based Overview Using Engineering Standards, Gail D. Baura The Biomedical Engineering Handbook, Joseph D. Bronzino