* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File - Optometry Peer Tutoring
Idiopathic intracranial hypertension wikipedia , lookup
Corrective lens wikipedia , lookup
Contact lens wikipedia , lookup
Mitochondrial optic neuropathies wikipedia , lookup
Photoreceptor cell wikipedia , lookup
Macular degeneration wikipedia , lookup
Visual impairment due to intracranial pressure wikipedia , lookup
Cataract surgery wikipedia , lookup
Eyeglass prescription wikipedia , lookup
Fundus photography wikipedia , lookup
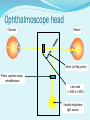
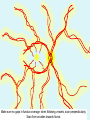
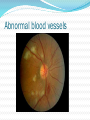
Ophthalmoscopy OP1201 – Basic Clinical Techniques Posterior eye Dr Kirsten Hamilton-Maxwell Today’s goals By the end of today’s lecture, you should be able to explain Why examining the posterior eye is important Basic construction and optical principles of the direct ophthalmoscope How to use it to examine the posterior eye and how to record results Have some awareness of normal and abnormal posterior eye conditions Limitations of direct ophthalmoscopy By the end of the related practical, you should be able to Assess and record the health of the posterior eye using direct ophthalmoscopy efficiently and accurately Ophthalmoscopy We have used the direct ophthalmoscope to examine the anterior eye Today we will look at the primary function of this device – examination of the posterior eye First, we need to know how it works The science How ophthalmoscopy works (the optics) Ophthalmoscope construction – lens rack, aperture stops and filters Basic anatomy of the posterior eye Optics of the eye Light from infinity enters the eye through the pupil and is focussed on the retina (in an eye with emmetropia only) Optics of the eye If a light source could be placed on the retina, it would exit the eye along the same path Light reflected from the retina behaves in the same way Optics of the eye The light reflected from the retina would be seen by an observer located along the same axis However, the observer would block the light source (why the pupil is black) Optics of ophthalmoscopy Concave mirror with central hole (or semi-silvered mirror) Alternatively a prism Light source at 90deg Optics of ophthalmoscopy If clinician and patient are both emmetropic then: Focussed on retina Convergent light Corrective lens is placed along pathway Parallel light Divergent light Convergent light, if subject myopic Divergent light, if subject hypermetropic Reflected light source Lens rack power In order for reflected light exiting the patient’s eye to be parallel, the patient’s ametropia (refractive error) must be corrected In order for the parallel light entering the clinician’s eye to be focussed correctly, the clinician’s ametropia must be corrected Need a corrective lens equal to sum of clinician’s and patient’s refractive errors As individual subjects and observers have a range of refractive errors, need a range of lens powers (i.e. a lens rack) Ophthalmoscope head Clinician Patient Mirror (or May prism) Filters, aperture stops, miscellaneous Lens rack (~-20D to +20D) Variable brightness light source Aperture stops Control the size of the beam Large, medium or small Use largest for external and internal examination If pupils small, reduce aperture size Use large or medium for internal examination Use smallest for foveal examination In general, use the largest beam possible for the best view Filters Red-free filter Blocks structures below Retinal Pigment Epithelium (RPE) and enhances contrast of retinal blood vessels and haemorrhages Helps in cup to disc (C/D) ratio assessment Helps identify nerve fibre layer (NFL) dropout – a sign of glaucoma Blue filter Can enhance reflectivity of optic disc drusen For use with fluorescein/fluorescein angiography Yellow filter Reduces UV exposure Miscellaneous Graticule Used in assessment of eccentric fixation Determine relative size and distance of fundus structures Slit beam Helps in assessment of 3-D structures e.g. optic cup Basic ocular anatomy Posterior eye Anterior eye Posterior eye anatomy Retinal nerve fibre radiations Macula – no Temporal blood vessels, darker pigment than surrounding area Vessel crossing Nasal Optic disc Blood vessels Veins are darker than arteries, usually larger Procedure Examining the posterior eye Examples Recording results How to do ophthalmoscopy Assume that the anterior eye examination has just been completed The lens power is +10D You are 10cm away from the eye The patient is looking 15deg up and to their temporal side Medium to large aperture stop First step is to locate the red reflex from the fundus We are aiming to bring this into focus = retinal structures visible What you see Direct ophthalmoscopy gives an erect, real, magnified image 15x magnification with a 5deg field of view through one eye Depends on Rx Higher magnification but smaller field of view for myopes Lower magnification but larger field of view for hypermetropes Pupil size Better field of view with larger pupils BUT field of view is always small No stereopsis What am I looking for? Lens Vitreous Optic disc Size Macula Whole area Fovea and foveal reflex Periphery C/D ratio Retina Margins Choroid Colour Blood vessels A/V ratio Crossings Calibre/tortuosity Reflectivity Leakage How to view the lens Retro-illumination Vitreous Get as close to your patient’s eye as you can With the red reflex visible, reduce lens rack power by 1D steps (towards zero, or plano) As you do this, you will focus at different depths within the vitreous until finally the fundus comes into focus If you and your patient are both emmetropic and not accommodating (almost impossible when you are learning), the lens power should be zero when you are in focus Vitreous floaters Will look like a dark shadow among the red/orange reflex Will move when the patient moves their eyes Scan the fundus Be systematic Use the disc as an orientation point If the patient is looking 15deg to the temporal side and you move in along the horizontal visual axis, you should find it straight away All of the blood vessels originate in the disc, so follow them from here. If you get lost, return to the disc and start again Ask the patient to look in the 9 cardinal directions to assess the periphery Make sure no gaps in fundus coverage: when following vessels, scan perpendicularly. Scan from arcades towards fovea. Blood vessels Look for Calibre – vessel width and regularity Tortuosity – “wriggliness” of vessels Artery/Vein (A/V) ratio Compare width of artery (red) to vein (darker red) Should be about 2/3 Crossings Does the vein change shape when crossed by an artery? Can be compressed leading to nipping Reflectivity – is the vessel sheath clear or opaque? Leaking – haemorrhages, exudates Normal vessels More normal vessels Abnormal blood vessels More abnormal blood vessels Retina Sometimes the word “retina” is used to mean the same thing as “fundus” Anatomically, the retina is a transparent layer containing photoreceptors and connecting cells The retinal interface with the vitreous may reflect light like a wet surface, but you will not usually see the retina itself unless there is a problem Retina Myelinated nerve fibres Retina Retinal detachment Macula Cones only Fovea in the centre More pigmented than surrounding retina No blood vessels Supplied by the underlying choroid and choriocapillaris Ask the patient to look directly into the light In young healthy eyes, you will see a yellow reflection = foveal reflex Note its presence and whether it is bright, moderate or dim Use graticule to assess centrality of the fovea Normal macula Darker at macula Note: This is also a tigroid fundus… choroidal blood vessels are visible (view usually blocked by the RPE) Macula disease ARMD - drusen Recording ophthalmoscopy Size and distance is recorded in terms of disc diameters Direction is recorded according to a clockface in hours Do not flip for RE and LE Locating a lesion - example This lesion is 1DD wide, 0.5DD high 1DD above the fovea OR 3DD from the disc at 10 o’clock Recording your findings Disc – for next week Clock directions 9 The area you can see with the direct ophthalmoscope 3 9 Macula Disc Use descriptive terms Write something for everything! 3 Background/periphery Vitreous Pigmentation changes in retinitis pigmentosa Asteroid hyalosis, floaters, haemorrhages Retinal tears, detachments Retinal nerve fibre layer Dropout in glaucoma, myelination at disc margin. Tumours Vessels Fovea Haemorrhages in diabetes, vessel occlusion, hypertension ARMD, drusen, macular holes Crossings: nipping in systemic hypertension Optic disc Myopic crescent in myopia Cupping and notching in glaucoma Bifurcations: embolisms, branch occlusions Anterior ischaemic optic neuropathy in diabetes Vessel walls: sheathing in systemic hypertension, leakage and neovascularisation in diabetes. Swelling and blurred margins in papilloedema and optic neuritis Limitations Limitations No stereopsis Small field of view Not all of the fundus covered, even by a thorough systematic technique Large lesions can be missed entirely, especially if the colour change is gradual Cannot see very far into the periphery Indirect ophthalmoscopy is preferred for fundus examination Further reading Elliott, Sections 6.4 to 6.5, 6.20 Become familiar with the procedural steps Memorise anatomical structures