* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Atypical antipsychotic medications
Serotonin syndrome wikipedia , lookup
Adherence (medicine) wikipedia , lookup
Drug interaction wikipedia , lookup
Pharmacognosy wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Pharmacogenomics wikipedia , lookup
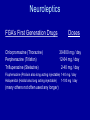
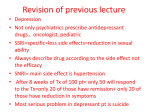
Little Known Secrets of Psychopharmacology David Cutler, MD Medical Director Bentson McFarland MD PhD Mental Health and Addiction Services Multnomah County Psychopharm (The Old and The New) • Part I Antipsychotics • Part II Antidepressants and Mood Stabilizers Childhood and adolescent depression. • Bhatia SK, Bhatia SC. Major depression affects 3 to 5 percent of children and adolescents. Depression negatively impacts growth and development, school performance, and peer or family relationships and may lead to suicide. Biomedical and psychosocial risk factors include a family history of depression, female sex, childhood abuse or neglect, stressful life events, and chronic illness. Diagnostic criteria for depression in children and adolescents are essentially the same as those for adults; however, symptom expression may vary with developmental stage, and some children and adolescents may have difficulty identifying and describing internal mood states. • Safe and effective treatment requires accurate diagnosis, suicide risk assessment, and use of evidence-based therapies. Current literature supports use of cognitive behavior therapy for mild to moderate childhood depression. If cognitive behavior therapy is unavailable, an antidepressant may be considered. Antidepressants, preferably in conjunction with cognitive behavior therapy, may be considered for severe depression. Tricyclic antidepressants generally are ineffective and may have serious adverse effects. Evidence for the effectiveness of selective serotonin reuptake inhibitors is limited. Fluoxetine is approved for the treatment of depression in children eight to 17 years of age. All antidepressants have a black box warning because of the risk of suicidal behavior. If an antidepressant is warranted, the risk/benefit ratio should be evaluated, the parent or guardian should be educated about the risks, and the patient should be monitored closely (i.e., weekly for the first month and every other week during the second month) for treatment-emergent suicidality. Before an antidepressant is initiated, a safety plan should be in place. This includes an agreement with the patient and the family that the patient will be kept safe and will contact a responsible adult if suicidal urges are too strong, and assurance of the availability of the treating physician or proxy 24 hours a day to manage emergencies. Major depressive disorder • Low mood / loss of pleasure (anhedonia) • Four or more of: Sleep disturbance Appetite disturbance Agitation / retardation Loss of energy Worthlessness / guilt Impaired concentration / decision-making Suicidal ideation Evidence- based treatments for people with major depressive disorder • • • • Cognitive-behavioral therapy Interpersonal therapy Antidepressant medication Electroshock treatment Antidepressants • Tricyclics • MAOIs Monoamine Oxidase Inhibitors • SSRIs Selective Serotonin Reuptake Inhibitors • Others: Trazodone, Nefazodone, Bupropion, and Mirtazapine Tricyclics • • • • • • • • Imipramine Amitriptyline Nortriptyline Desipramine Clomipramine Doxepin Maprotiline Protriptyline Doses 75-300Mg 50-300Mg 75-150Mg 100-300Mg 25-250Mg 75-350Mg 75-225Mg 15-60Mg MAOIs • • • • • Phenylzine (Nardil) 15-90Mg Isocarboxazid (Marplan) 20-60Mg Tranylcypromine (Parnate) 30-60MG Selegiline Transdermal (EMSam) 20-40Mg Food Restrictions: Cheese, Fava Beans, Salami,Brewers Yeast, Red Wine, Chocolate, and others may cause hypertensive crisis. • Used for Atypical depression, Dysthymia, Narcolepsy, Chronic Pain, Headache,Bulimia,OCD, GAD SSRIs • • • • • • • Fluoxetine (Prozac) 20-80 Mg Paroxetine (Paxil) 10-60Mg Fluvoxamine (Luvox) 50-300Mg Citalopram (Celexa) 20-60Mg Escitalopram (Lexapro) 10-20Mg Duloxetine (Cymbalta) 20-60Mg Venlafaxine (Effexor) 75-375Mg Others • Trazodone (Desyrel) 150-600Mg (used mostly for sleep) • Nefazodone (Serzone) 200-600Mg (liver problems) • Bupropion (Wellbutrin) 200-450 Mg (Less side effects) • Mirtazapine (Remeron) 15-45Mg (also used for sleep) CNS Neurotransmitter Effects Serotonin Norepinephrine Dopamine • • • • • • • Amitriptyline ++++ Bupropion 0/+ Citalopram ++++ Fluoxetine ++++ Maprotiline 0 Paroxetine ++++ Venlafaxine ++++ ++++ + 0 0 ++++ 0/+ +++ 0 ++ 0 0/+ 0 0/+ 0/+ Antidepressant medications • Effectiveness more or less same – Roughly 60% of drug-naïve patients respond (mostly in drug company studies but also in federally funded studies) – Roughly 30% of patients respond to placebo • Side effects different • Prices different (but patents expiring rapidly) Adverse Effects • Tricyclics: Sedation, Risk of Death with Overdose • MAOI’s: Hypertensive Crisis, Serotonin Syndrome • SSRI’s: P450 Enzyme Drug interactions + Wt Gain, Decreased Sex Drive, Serotonin Syndrome. • Venlafaxine can raise B/P Cost of a Month’s Antidepressant Treatment • • • • • • • Nortriptiline Fluoxetine Citalopram Mirtazapine Paroxetine Bupropion XR Duloxetine (Cymbalta) $ 6 $ 20 $ 20 $ 40 $ 60 $ 70 $120 $4 / month scripts at Target • • • • • • • • • Amytriptyline 10,25,50,75,and 100Mg x30 Doxepin 10,25, 50, 75, 100 Mg x 30 Nortriptyline 10, and 20 Mg x 30 Citalopram 20, 40 Mg x 30 Fluoxetine 10 tbs + 10,20,40 Mg Cps x 30 Paroxetine 10,20 Mg x 30 Trazodone 50, 100, 150 Mg Tabs x 30 LI CO3 300 Mg x 90 Carbamezepine 200Mg x 60 Antidepressant medications • What to do if patient fails to respond ? – Switch (different drug) – Augment (continue original drug and add another drug) – Stop drug / start cognitive behavioral therapy – Cognitive behavioral therapy with a drug Mood Stabilizers For Bipolar • • • • • • • Lithium Carbonate 900-1500Mg / Day Anticonvulsants Carbamazapine 400-1600Mg/Day Valproic Acid 750-4200Mg/Day Lamotrigine 50-200Mg/Day Topiramate 50-400Mg/Day Neurontin 1200-3600Mg/day Adverse Effects of Mood Stabilizers • Lithium: Vomiting, Tremor, Polyuria, Hypothyroidism, Confusion, Death • Valproic Acid: Tremor, Wt Gain, Edema, Thrombocytopenia, Diplopia, Sedation • Carbamezapine: Leukopenia,Ataxia, Sedation, Wt Gain • Lamotragine: Dizzyness, Ataxia, Diplopia, • Headaches, Rash (slow titration reduces the chances of getting a rash) Sequenced Treatment Alternatives to Relieve Depression (STAR*D) • Funded by National Institute of Mental Health • Drug companies provided medication • What to do when depressed patient fails to improve with medication? STAR*D • Level One = citalopram (Celexa) • Level Two = switch drug or augment – Switch drug = Level Two • • • • Bupropion (Wellbutrin) SR Sertraline (Zoloft) Venlafaxine XR (Effexor) Cogntive Behavioral Therapy – Augment = Level Two • Celexa plus Bupropion • Celexa plus Buspirone • Celexa plus Cognitive Behavioral Therapy • Level Three (switch again or more complex augmentation) • Level Four (switch to Remeron plus Effexor = California Rocket Fuel) Star*D Algorithm Levels 1&2 • Level 1 (twelve weeks more or less) • Initial Treatment Citalopram (Celexa) • Level 2 (twelve weeks more or less) • Switch to: Bupropion SR, Cognitive Therapy, Sertraline, Venlafaxine ER or • Augment With: Bupropion SR, Buspirone, Cognitive Therapy STAR*D Algorithm Level 2A • (Only for those receiving cognitive therapy in level 2) • Switch to : Bupropion SR (Sustained release) or Venlafaxine ER (Extended release) STAR*D Algorithm Level 3 &4 • Level 3 (twelve weeks more or less) • Switch to : Mirtazapine or Nortriptyline or • Augment with: Lithium or Triiodothyronine (T3) (only with Bupropion SR, Sertraline, Venlafaxine ER) • Level 4 (twelve weeks mor or less) • Switch to: Mirtazapine combined with Venlafaxine ER STAR*D Treatment of Depression • The STAR*D study is the largest prospective study of a sequential series of treatments for depression ever conducted. In this study, 3,671 patients entered treatment at 41 sites, 18 of which were primary care facilities. The STAR*D study differs from typical clinical trials. Subjects were identified as they came for treatment. Although psychotic and bipolar patients were excluded, most other psychiatric disorders were allowed. Most clinical trials in depression exclude patients with recent active substance abuse. STAR*D only excluded patients likely to need inpatient detoxification. Of the patients entering the first treatment step, 61.5% had a concurrent psychiatric disorder. As the result of broad inclusion criteria, the STAR*D study is more representative of patients in clinical practice. STAR*D Remission • • • • Level One (Celexa) Level Two (switch or augment) Level Three (switch or augment) Level Four (rocket fuel) 37% 31% 14% 13% STAR*D Remission Are some drugs better than others? • Switch to bupropion (Wellbutrin), sertraline (Zoloft), venlafaxine (Effexor considered more potent): – all the same • Augment with bupropion (Wellbutrin) or buspirone (Buspar): – bupropion (Wellbutrin) maybe a little more effective and better tolerated Remission • Remission rates were 36.8%, 30.6%, 13.7%, and 13% after treatment steps 1 through 4. Remission rates drop substantially after two failed treatments. • Higher remission rates during the initial trial were seen in patients who were female, Caucasian, employed, or had higher levels of education and income. Patients who required more treatments were more severely depressed and had more concurrent psychiatric and medical disorders. Relapse • Among those achieving remission, relapse rates were 33.5%, 47.4%, 42.9%, and 50.0% after the four treatment steps. Relapse rates were even higher in patients who improved but did not achieve remission (range=59% to 83%). It is particularly worrisome that at steps 3 and 4, in addition to low remission rates (13.7% and 13.0%), nearly half of those remitting relapsed. From step 2 on, less than half of those responding and remitting remained well. • The study also found that intolerance increased after each treatment step: 16.3%, 19.5%, 25.6%, and 34.1%. (the term "intolerance" includes dropouts for any reason during the first 4 weeks, or side effects after that). Perhaps patients that drop out are becoming demoralized with each failure and are giving up. STAR*D Relapse within twelve weeks of remission • • • • Level 1 (Celexa) 34% Level 2 (Switch or augment) 47% Level 3 (Switch or augment) 43% Level 4 (Rocket fuel) 50% For STAR*D patients, Maintaining Recovery is not Easy. • This study paints a less hopeful picture for the treatment of depression, but it may be consistent with "real world" patients. More than 75% of the STAR*D patients had recurrent or chronic depression, 61.5% had a concurrent psychiatric diagnosis, and 83% had previous treatment for their current episode (N=3,057 of 3,671). • • • • 0123 0 20 40 60 80 100 age Behavior Suicidality Psychosis /Positive Symptoms • Hallucinations (false perceptions) – hearing voices others do not hear – Seeing,feeling,or smelling things other do not • Delusions (false beliefs) – Not believed by others in the culture – Thoughts controlled by Martians – Radios implanted in teeth • Disordered Thought Processes Loose associations, Word salad, Flight of Ideas Diagnostic Criteria S/A 295.70 • A. An uninterrupted period of illness with major depression or mania or mixed with Schizophrenic Symptoms. • B. During the same period delusions or hallucinations without mood symptoms. • C. Mood Symptoms are present for a substantial portion of the illness period • D. Not due to drugs • Type: Bipolar (includes mania) Depressive Biochemistry of psychosis • Dopamine relative excess • Causes – Substance abuse (e.g., methamphetamine) – Medications (e.g., prednisone) – Heredity (e.g., Huntington’s disease) – Functional disorder (e.g., schizophrenia) People with schizophrenia • Psychosis (“positive” symptoms) • Decline in function (“negative” symptoms) – Lack of ambition – Social withdrawal Medications for people with schizophrenia • Neuroleptics – First generation antipsychotic drugs – Typical antipsychotic drugs • Atypical antipsychotic drugs – Second generation antipsychotics Neuroleptics FGA’s First Generation Drugs Chlorpromazine (Thorazine) Perphenazine (Trilafon) Trifluperazine (Stelazine) Doses 30-800 mg / day 12-64 mg / day 2-40 mg / day Fluphenazine (Prolixin also long acting injectable) 1-40 mg / day Haloperidol (Haldol also long acting injectable) 1-100 mg / day (many others not often used any longer) Neuroleptic medications • Block doparmine • Reduce psychosis (positive symptoms) • Extrapyramidal side effects – – – – – Involuntary motor system Stiffness Tremors Restlessness Tardive dyskinesia • May worsen negative symptoms • Some weight gain • Cheap (five to ten cents per day) Tardive dyskinesia • Abnormal involuntary movements – Lip smacking – Tongue thrusting • Neuroleptic side effect • May be permanent Atypical Antipsychotic drugs SGAs • • • • • • Clozapine (Clozaril) 12.5-900 Mg/Day Risperidone (Risperdal) 2-16 Mg/Day Olanzapine (Zyprexa) 5-20 Mg/Day Ziprasidone (Geodon) 40-60 Mg/Day Quetiapine (Seroquel) 50-750 Mg/Day Aripiprazole (Abilify) 10-30 Mg/Day Atypical antipsychotic drugs • Block dopamine but also involve serotonin (and maybe other neurotransmitters) • Reduce psychosis (positive symptoms) • May improve negative symptoms • Few motor side effects • Weight gain • Diabetes • Strokes in users over age 65 • Expensive (e.g., $5 to $10 per day) Clozapine • • • • Clozaril (and generics) Affects dopamine, serotonin, perhaps more May improve positive and negative symptoms Side effects include weight gain, seizures, sedation, and salivation (but not tardive dyskinesia) • Agranulocytosis (no white blood cells) possible – Blood draws weekly or twice monthly – National registry system – Need to fail other antipsychotic drugs • Works extremely well for a few people Olanzapine • • • • • • Zyprexa Improves positive symptoms Might help negative symptoms Weight gain in almost all users Diabetes in many (perhaps most) users Intramuscular (short acting) form available • Used (at least once) by 20 million people worldwide • Used annually by 2 million people worldwide • $ 4 billion per year for manufacturer Eli Lilly • Indicated for schizophrenia and bipolar mania Disparity Emerges in Lilly Data on Schizophrenia Drug • • By ALEX BERENSON NY Times, December 21, 2006 • • • • • • • For at least a year, Eli Lilly provided information to doctors about the blood-sugar risks of its drug Zyprexa that did not match data that the company circulated internally when it first reviewed its clinical trial results. The original results showed that patients on Zyprexa, Lilly's pill for schizophrenia, were 3.5 times more likely to experience high blood sugar levels than those taking a placebo. But the results that Lilly eventually provided to doctors indicated that patients taking Zyprexa were only slightly more likely to suffer high blood sugar as those taking a placebo, or an inactive pill. Another Lilly report, from November 1999, shows that Lilly found after examining 70 clinical trials that 16 percent of patients taking Zyprexa for a year gained more than 66 pounds. The company did not publicly disclose that figure, instead they showed trials that showed about 30 percent of patients gained 22 pounds. • • • • Risperidone • • • • • • • Risperdal (generic in 2007) Risperdal Consta (long acting injection – two weeks or more) Improves positive symptoms Rare improvement of negative symptoms Extra-pyramidal side effects not uncommon Some weight gain Indicated for autism irritability as well as psychosis (schizophrenia and bipolar mania) Quetiapine • • • • • • Seroquel Some improvement in positive symptoms Rare improvement in negative symptoms Sedating Twice a day dosage not uncommon Indicated for bipolar depression as well as schizophrenia and bipolar mania Ziprasidone • • • • Geodon Some impact on positive symptoms Rare impact on negative symptoms Usually taken twice a day • Intra-muscular (short acting) form available • Indicated for schizophrenia and bipolar mania • Some weight gain Aripiprazole • Abilify • Perhaps some impact on positive symptoms • Rare (if ever) impact on negative symptoms • No (or rare) weight gain Research on atypical antipsychotic medications • Clozapine versus haloperidol (U.S. Veterans) • Clinical antipsychotic trial of clinical effectiveness (CATIE – United States) • Cost Utility of Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS – England) Clozapine versus Haloperidol • Supported by U.S. Department of Veterans Affairs • 423 veterans at 15 veterans hospitals • Refractory schizophrenia • Clozapine versus haloperidol (plus benztropine = Cogentin) • No difference in positive or negative symptoms • More extra-pyramidal side effects in haloperidol group • More weight gain in clozapine group • Expenditures same • Comments: – Do veterans represent everyone with schizophrenia? – Does the veterans health care system represent other systems? • Rosenheck et al. New England Journal of Medicine 337:809, 1997 Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) – I Study design • Sponsored by National Institute of Mental Health (U.S. Public Health Service) • • • • • • 1,493 patients with schizophrenia at 57 sites (2001 – 2004) Average age 41 74% male 60% white 85% unemployed Randomized to: – – – – – • • Olanzapine (Zyprexa) Risperidone (Risperdal) Quetiapine (Seroquel) Ziprasidone (Geodon) Perphenazine (Trilafon = neuroleptic) Outcome = discontinuation of medication assigned at baseline Lierberman et al. (2005). New England Journal of Medicine 353:1209 Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE)-II Baseline Psychotropic use Among Participants • Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) – III Main outcome Discontinuation of assigned medication for any reason Olanzapine (Zyprexa) * Quetiapine (Seroquel) Risperidone (Risperdal) Ziprasidone (Geodon) Perphenazine (Trilafon = neuroleptic) Percent Months on drug 64% 82% 74% 79% 75% 9.2 4.6 4.8 3.5 5.6 * Participants stayed on Zyprexa significantly longer than any other drug Time on all other drugs the same (i.e., Trilafon same as atypicals) Lierberman et al. (2005). New England Journal of Medicine 353:1209 Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) – IV Secondary outcome Hospitalization due to schizophrenia exacerbation Olanzapine (Zyprexa) * Quetiapine (Seroquel) Risperidone (Risperdal) Ziprasidone (Geodon) Perphenazine (Trilafon = neuroleptic) Percent Admits per year 11% 20% 15% 18% 16% 0.29 0.66 0.45 0.51 0.57 * Participants on Zyprexa stayed out of hospital more than any other drug Hospitalization rate on all other drugs the same (i.e., Trilafon same as atypicals) Lierberman et al. (2005). New England Journal of Medicine 353:1209 Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) – V Side effects Pounds per month Olanzapine (Zyprexa) * Quetiapine (Seroquel) Risperidone (Risperdal) Ziprasidone (Geodon) Perphenazine (Trilafon = neuroleptic)@ + 2.0 + 0.5 + 0.4 - 0.2 - 0.3 Extra-pyramidal side effects 2% 3% 3% 4% 8% * Weight gain significantly more on Zyprexa than other drugs @ More participants on Trilafon stopped due to extra-pyramidal side effects than did users of other drugs Lierberman et al. (2005). New England Journal of Medicine 353:1209 Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) – VI Phase Two: clozapine • • 99 Phase One participants who discontinued first drug due to lack of efficacy Randomized to clozapine versus atypical not received in Phase One Months to discontinuation in phase two Clozapine * Olanzapine Quetiapine Risperidone * 10.5 2.7 3.3 2.8 Time on clozapine significantly longer than time on other drugs No differences among drugs other than clozapine Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) – VII Comments • More reports coming (e.g. cost-effectiveness) • Do participants represent everyone with schizophrenia? (if you were doing well, would you volunteer?) Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia (CUtLASS) • Supported by United Kingdom Ministry of Health • • • • • • • • • • • 227 participants with schizophrenia at 14 community clinics in England Randomized to first generation versus second generation antipsychotic Psychiatrists chose drug in each class before randomization Average age 40 68% female 75% white 40% inpatients at randomization Primary outcome = quality of life Quality of life same at one year after randomization Cost studies forthcoming Jones et al. (2006). Archives of General Psychiatry 63:1079