* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Relationship of Left Ventricular Structure to
Remote ischemic conditioning wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
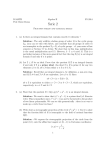
Relationship of Left Ventricular Structure to Maximal Heart Rate During Exercise* William F. Graettinger, MD, FCCP; David H. G. Smith, MD; Joel M. Neutel, MD; Jonathan Myers, PhD; Victor F. Froelicher, MD; and Michael A. Weber, MD Previous investigators using clinical, hemodynamic, or exercise parameters to predict maximal exercise heart rate (HRmax) have demonstrated age to be the major determinant. Regression coefficients have ranged from -0.3 to -0.6, leaving approximately two thirds of the variance in HRmax unexplained. Because cardiac size and function are directly related to stroke volume and should influence HRmax, we studied 114 male subjects (aged 19 to 73 years) with two-dimensional and M-mode echocardiography who underwent maximal treadmill testing with respiratory gas analysis. Seventy-three were normotensive (diastolic BP<95 mm Hg) and 41 were hypertensive. As in previous studies, HRmax was inversely related to age (HRmax= 199-0.63 [age], r= -0.47, p<0.001). M-mode left ventricular (LV) diastolic dimension (LVD) added significantly to the explanation of the variance in HRmax (r=-0.57, p<0.001) (HRmax=236-0.72 [age]-6.8 [LVD]). Thus, the larger the heart, the lower the HRmax. No other echocardiographic measurement or derived parameter added significantly to the explanation of the variance in HRmax. To evaluate the effects of hypertension on HRmax, we studied hypertensives and normotensives separately. Only age was significantly related to HRmax in the normotensives (r=-0.50, p<0.001). In the hypertensive subjects, however, both age and relative wall thickness (RWT) (which describes LV wall thickness in relation to 3he physiologic response to aerobic exercise is a complex cardiorespiratory, neurohumoral, vascular, and muscular process. The linear relationship between oxygen consumption and cardiac output throughout exercise is well known.1 The major factor mediating the increase in cardiac output associated with exercise is an increase in heart rate. Maximal heart rate (HRmax) is directly correlated with maximal oxygen consumption and therefore, HRmax has been used as an approximation for maximal cardiac work. Age has been demonstrated to be the prime *From the Cardiology and Hypertension Sections, Department of Veterans Affairs Medical Center, Long Beach, Calif, and the University of California, Irvine. Presente in part at the 64th Scientific Sessions, American Heart Association, Anaheim, Calif, Nov. 11-14, 1991 Supported in part by a Merit Review Grant from the Department of Veterans Aff airs. Manuscript received January 11, 1994; revision accepted May 24. Reprint requests: Dr. Graettinger, 1000 Locust Street (111), Reno, NV 89520 LV chamber size) were significantly related to HRmax. Age explained 45% of the observed variance in HRmax (r=0.67, p<0.001) and RWT added modestly (9%O) but significantly to the relationship (HRmax=173-0.96 [age]+94 [RWT], p<0.001), together explaining 54% of the variance observed in HRmax. Thus, HRmax is inversely related to LVD and patients with larger ventricles achieve lower HRmax. In hypertensives, the amount of LV muscle mass in relation to chamber size is an additional predictor of HRmax. However, despite controlling for age, sex, and cardiovascular disease, and the inclusion of echocardiographic indices of cardiac size and function, a large portion of the variance in HRmax could not be explained. The unexplained variance in HRmax is most likely due to intersubject variability in resting cardiac size, volume, function, and other as yet undefined factors. (Chest 1995; 107:341-45) HRmax=maximal heart rate; IVS=interventricular septal thickness; LV=left ventricular; LVD=left ventricular diastolic dimension; PW=posterior wall; RWT=relative wall thickness Key words: exercise; left ventricular size; maximal heart rate; variance determinant of maximal exercise heart rate. Regression coefficients for the inverse relationship between HRmax age have ranged from -0.3 to -0.5.2-6 This relationship explains only approximately one third of the variance in maximal exercise heart rate. This relatively poor relationship between HRmax and age therefore limits the prediction of HRmax as an indicator of maximal effort during exercise testing, to establish a target heart rate for exercise training, and to identify individuals with a truly abnormal HRmax. Previous studies have used age as the predictor of HRmax. The potential effects of other clinical or echocardiographic parameters remain unknown. This study was undertaken to (1) evaluate further which factors, alone or in combination with age, might have a significant relationship with HRmax, thus more accurately predicting the HRmax response to exercise, and (2) what effect, if any, untreated hypertension has on this relationship. CHEST / 107 / 2 J FEBRUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21708/ on 05/02/2017 341 METHODS Study Group The study group consisted of 114 healthy male subjects (aged 19 to 73 years). Of these, 41 were hypertensive (diastolic BP>95 mm Hg) and 73 were normotensive based on the mean of six resting blood pressure readings. Two measurements were made in the sitting position by standard mercury sphygmomanometer after 3 min of quiet sitting. Measurements were obtained at each of three office visits and all readings were averaged. No patient was receiving antihypertensive medication. The hypertensive subjects either had never been treated with antihypertensive medication or had not been receiving medication for greater than 8 months. Subjects were without any known medical conditions (other than hypertension in 41) and had normal results of physical examinations. All subjects gave written informed consent approved by the Institutional Review Board. Echocardiography Cardiac structure and function were assessed by two-dimensional guided M-mode echocardiography utilizing a commercially available phased-array echocardiograph (GE Pass II or RT 5000, Milwaukee). M-mode data were recorded on strip-chart at a paper speed of 50 mm/s. M-mode measurements were made utilizing the standards of the American Society of Echocardiography.7 M-mode tracings were accepted only for inclusion after two-dimensional echo analysis revealed normal left ventricular (LV) contractile pattern and function. Relative wall thickness (RWT) was computed by the following equation: RWT=(IVS+PW)/LVD, where IVS=interventricular septal thickness, PW=LV posterior wall thickness, and LVD=left ventricular diastolic dimension. The LV mass was calculated by the formula of Troy et al.8 All measurements were made by two observers who were unaware of the patients' blood pressure or exercise data and any disagreement was resolved by consensus. Exercise Protocol Two cardiopulmonary exercise treadmill tests separated by 7 to 14 days were performed by each patient. The first utilized a modified Balke-Ware protocol.9 Its purpose was to familiarize the subject with the procedures of treadmill exercise and expired gas analysis and to measure the subject's maximal oxygen consumption as previously described.'0 These data were utilized to perform a second test from which the data described herein were derived. Subjects were exercised to exhaustion using a ramp treadmill protocol during which treadmill speed and grade were individualized to achieve maximal workload corresponding to maximal oxygen consumption as determined by the first test11 in approximately 10 min. Maximal heart rate was calculated from the R-R intervals using a 6-s rhythm strip'2 at maximal exercise recorded on the peak exercise electrocardiogram. Blood pressure was measured immediately prior to the test, every 2 min during exercise, at peak exercise, and immediately after exercise. Perceived effort was reported throughout and at maximal exertion.13 Catecholamines Blood for epinephrine and norepinephrine was drawn via heparin lock after a 30-min supine rest period, standing immediately before the treadmill, and standing immediately after the treadmill. Statistical Analysis Statistical analysis was done using software (SPSS/PC+) on a microcomputer. Correlations between variables were obtained by stepwise multiple linear regression analysis. Variables were included in the regression equation if the f-test for inclusion was 342 Table 1-Clinical Characteristics Normotensive Hypertensive Group Group n=73 n=41 43±13 Age, yr Weight, kg 83+12 129 ± 13 Resting systolic BP, mm Hg 86 + 6 Resting diastolic BP, mm Hg 67 ± 10 Resting heart rate, bpm SBP max, f mm Hg 195 +21 DBP max,f mm Hg 81±14 HR max, bpm 170±18 *p<0.05. fDBP max=maximal diastolic BP; SPP max=maximal 50±14* 88±12* 149 + 15* 101 ± 4* 74 ± 10* 209 ± 22* 94 ± 16* 165 ±18 systolic BP. significant at the p value<0.05 level. Only variables that made statistically significant contributions to the explanation of the variance observed in the dependent variable are reported. Comparisons between groups were made with unpaired Student's t tests. A two-tailed t test with a p value <0.05 was required for significance. Results are presented as mean ± 1 SD. RESULTS Clinical characteristics of the study groups are given in Table 1. The hypertensive subjects tended to be older and slightly heavier than normotensive subjects. Their resting and maximal exercise blood pressures were significantly higher than those in normotensive subjects. Resting heart rate was slightly higher and HRmax tended to be slightly but not significantly lower in the hypertensive group. Maximal perceived effort was similar in both groups (19.2 ± 1 vs 19.2 ± 1 Borg units). Echocardiographic characteristics of the groups are given in Table 2. There were no significant differences between the two groups in any of the measured or derived parameters. The catecholamine data are given in Table 3. There were no differences in the mean epinephrine or norepinephrine levels between the normotensive and hypertensive groups at rest or immediately after exercise. Both groups demonstrated a similar rise in Table 2-Echocardiographic Characteristics* LVD, cm IVS, cm PW, cm LA, cm LVM, g LVMI, g/m2 Normotensive Hypertensive Group Group n=73 n=41 5.1±0.4 1.05±0.12 1.06± 0.12 4.0± 0.5 259 ± 57 128 ±25 LVM/HT, g/cm 1.45±0.32 RWT 0.41 ± 0.05 5.1±0.4 1.09±0.11 1.09 ±0.11 4.0±0.5 265 ±52 130±25 1.5±0.29 0.43 ± 0.06 *LA=left atrium; LVM=LV mass; LVMI=LV mass index; LVM/ HT=LV mass/height LV Structure and Maximal Heart Rate During Exercise (Graettinger et al) Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21708/ on 05/02/2017 REFERENCES 1 2 3 4 5 6 7 8 Astrand PO. Textbook of work physiology. New York: McGraw Hill, 1977; 188 Hammond HK, Kelly TL, Froelicher VF. Radionuclide imaging correlates of heart rate impairment during maximal exercise testing. J Am Coll Cardiol 1983; 2:826-33 Scheffield LT, Malouf JA, Sawyer JA, Roitman D. Maximal heart rate and treadmill performance of healthy women in relation to age. Circulation 1978; 57:79-84 Bruce RA, Fischer FD, Cooper MN, Gey GO. Separation of effects of cardiovascular disease and age on ventricular function with maximal exercise. Am J Cardiol 1974; 34:757-63 Froelicher VF, Yanowitz F, Thompson AJ, Longo MR, Triebwasser JH. Treadmill exercise testing at the USAF School of Aerospace Medicine: physiologic responses in aircrewmen and the detection of latent coronary artery disease. Advisory Group for Aerospace Research and Development 1975; 210:1-37 Lester M, Sheffield LT, Trammell P, Reeves TJ. The effect of age and athletic training on the maximal heart rate during muscular exercise. Am Heart J 1968; 76:370-76 Sahn DJ, DeMaria A, Kisslo J, Weyman A. Committee on M-mode standardization of the American Society of Echocardiography: recommendations regarding quantization in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978; 58:1072-83 Troy BL, Pombo J, Rackley CE. Measurement of ventricular wall thickness and mass by echocardiography. Circulation 1972; 45:602-11 9 Wolthuis RA, Froelicher VF, Fischer J, Noguera I, Davis G, Stewart AJ, et al. New practical treadmill protocol for clinical use. Am J Cardiol 1977; 39:697-700 10 Myers J, Walsh D, Froelicher VF. Effect of sampling on vari- ability and plateau in oxygen uptake. J Appl Physiol 1990; 68:404-10 11 Myers J, Buchanan N, Walsh D, Kraemer M, McAuley P, Hamilton-Wessler M, et al. A comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol 1991; 17:1334-42 12 Drayer JIM, Gardin JM, Brewer DD, Weber MA. Disparate relationships between blood pressure and LV mass in patients with and without LVH. Hypertension 1987; 9(suppl 2):11611164 13 Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med 1970; 23:92-8 14 Longhurst JC. Arterial baroreceptors in health and disease. Cardiovasc Rev Rep 1982; 3:271-99 15 Bainbridge FA. The influence of venous filling upon the rate of the heart. J Physiol 1915; 50:65-84 16 Robinson BF, Epstein SE, Beiser GD, Braunwald E. Control of heart rate by the autonomic nervous system: studies in man on the interrelation between baroreceptor mechanisms and exercise. Circ Res 1966; 19:400-11 17 Atwood JE, Myers J, Sandhu S, Lachterman B, Friis R, Oshita A, et al. Optimal sampling interval to estimate heart rate at rest and during exercise in atrial fibrillation. Am J Cardiol 1989; 63:45-8 18 Neutel JM, Smith DHG, Graettinger WF, Weber MA. Heredity and hypertension: impact on metabolic characteristics. Am Heart J 1992; 124:435-40 19 Neutel JM, Smith DHG, Graettinger WF, Weber MA. Depen- dency of arterial compliance on circulating neuroendocrine and metabolic factors in normal subjects. Am J Cardiol 1992; 69:1340-44 20 Hammond HK, Froelicher VF. Normal and abnormal heart rate responses to exercise. Progress Cardiovasc Dis 1985; 27:271-96 A Practicum: Exercise Testing and Interpretation March 23 - 25, 1995; Harbor-UCLA Medical Center, Torrance, California Sponsored by the Division of Respiratory and Critical Care Physiology and Medicine, Harbor-UCLA Medical Center. Contact: Shirley Zagala, Box 405, Harbor-UCLA Medical Center, RB2, Room 319, 1000 W. Carson Street, P.O. Box 2910, Torrance, CA 90509-2910. Tel: 310 222-3803. CHEST / 107/21 FEBRUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21708/ on 05/02/2017 345 A ber size is inversely related to HRmax. The addition of LV dimension to the regression equation explained M . an additional 4% of the variance in HRmax. These A o- ~ . * . x data confirm a previous study from our group that *. suggested that hypertensive subjects with larger M A hearts might have reduced LV performance during L exercise.12 However, RWT, a measure of appropriH ateness of hypertrophy in relation to LV size, was a E predictor of HRmax in the hypertensive subjects; the A D .-. R greater the wall thickness recorded for a given LV T size, the greater the HRmax. That is, increased wall D R A r * -0.5, p <0.001 thickness in proportion to LV chamber size appears T to be associated with increased ability to do maximal D_ E 45 55 35 65 25 15 75 work in hypertensive patients. In contrast, LV enAGE largement without an appropriate increase in wall thickness results in decreased ability to do maximal B work. M The reasons for the varying degrees of myocardial A x 0 hypertrophy in relation to ventricular size are poorly understood. Intrinsic or secondary myocardial M o . . * . A changes related to hypertension and its concomitant L * * * . *. .metabolic'8 and neuroendocrine changes'9 may play H a role. A possible explanation for the relationship E . between 0 * * HRmax and RWT is that catecholamines, A R which have growth-promoting effects on myocardial T also mediate the heart rate response to exercise. cells, D R As the subjects in this study had only minimal r * -0.67, p <0.001 A amounts of LV hypertrophy and normal to miniT D0 E E 28 35 85 45 65 75 15 mally dilated ventricles, it is unlikely that these AGE changes would be associated with diminished function or exercise capacity. FIGURE 1. The linear regression of maximal heart rate on age is plotted in the normotensive (top, A) and hypertensive (bottom, B) subjects or de]monstrable cardiovascular disease; they reportedI similar activity levels; and all subjects were exercihsed utilizing the same type of exercise. The hyperltensive subjects tended to be heavier than the normc tensive subjects, but weight has not been demoiastrated to have an influence on HRmax in previo)us studies. There was no difference in the perceived[ maximal effort as assessed by the Borg scale and mieasured Vo2max was similar in the two groups indicaLting that even if true maximal effort was not attain(ed, both groups at least achieved a similar level of exertion. Heart rate continuously increases throughout exercise and does not achieve a steady-state. It then drops rapidly on stopping exercise and then gradually decreases during the recovery phase. To avoid inaccuracies in HRmax measurement induced by these phenomena, HRmax was calculated from R-R intervals on a 6-s rhythm strip'7 recorded at peak exercise, thus providing a close representation of the instantaneous maximal rate attained. The current data also demonstrate that LV cham344 Our findings are also in agreement with the observation of reduced HRmax in aerobically trained individuals, especially younger individuals who may experience an increase in LV mass.20 The large portion of the variance in HRmax that remains unexplained by age appears to be partially attributable to intersubject variability, including cardiac size, LV hypertrophy relative to the LV size, and the presence of hypertension. The inclusion of these factors improved the prediction of HRmax, especially in hypertensive subjects. Additional factors that may influence HRmax need to be identified and may allow better description of the physiologic attributes involved. CONCLUSIONS It is of physiologic interest that LV measurements inversely related to HRmax. However, the improvement in prediction of HRmax by the addition of LV size to age is not great enough to be meaningful for clinical application, and there remains too much unexplained variance to establish normalcy or to set heart rate goals during exercise using modified regression equations. Age-adjusted goals still have are significant clinical utility. LV Structure and Maximal Heart Rate During Exercise (Graettinger et al) Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21708/ on 05/02/2017 REFERENCES 1 2 3 4 5 6 7 8 Astrand PO. Textbook of work physiology. New York: McGraw Hill, 1977; 188 Hammond HK, Kelly TL, Froelicher VF. Radionuclide imaging correlates of heart rate impairment during maximal exercise testing. J Am Coll Cardiol 1983; 2:826-33 Scheffield LT, Malouf JA, Sawyer JA, Roitman D. Maximal heart rate and treadmill performance of healthy women in relation to age. Circulation 1978; 57:79-84 Bruce RA, Fischer FD, Cooper MN, Gey GO. Separation of effects of cardiovascular disease and age on ventricular function with maximal exercise. Am J Cardiol 1974; 34:757-63 Froelicher VF, Yanowitz F, Thompson AJ, Longo MR, Triebwasser JH. Treadmill exercise testing at the USAF School of Aerospace Medicine: physiologic responses in aircrewmen and the detection of latent coronary artery disease. Advisory Group for Aerospace Research and Development 1975; 210:1-37 Lester M, Sheffield LT, Trammell P, Reeves TJ. The effect of age and athletic training on the maximal heart rate during muscular exercise. Am Heart J 1968; 76:370-76 Sahn DJ, DeMaria A, Kisslo J, Weyman A. Committee on M-mode standardization of the American Society of Echocardiography: recommendations regarding quantization in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978; 58:1072-83 Troy BL, Pombo J, Rackley CE. Measurement of ventricular wall thickness and mass by echocardiography. Circulation 1972; 45:602-11 9 Wolthuis RA, Froelicher VF, Fischer J, Noguera I, Davis G, Stewart AJ, et al. New practical treadmill protocol for clinical use. Am J Cardiol 1977; 39:697-700 10 Myers J, Walsh D, Froelicher VF. Effect of sampling on vari- ability and plateau in oxygen uptake. J Appl Physiol 1990; 68:404-10 11 Myers J, Buchanan N, Walsh D, Kraemer M, McAuley P, Hamilton-Wessler M, et al. A comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol 1991; 17:1334-42 12 Drayer JIM, Gardin JM, Brewer DD, Weber MA. Disparate relationships between blood pressure and LV mass in patients with and without LVH. Hypertension 1987; 9(suppl 2):11611164 13 Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med 1970; 23:92-8 14 Longhurst JC. Arterial baroreceptors in health and disease. Cardiovasc Rev Rep 1982; 3:271-99 15 Bainbridge FA. The influence of venous filling upon the rate of the heart. J Physiol 1915; 50:65-84 16 Robinson BF, Epstein SE, Beiser GD, Braunwald E. Control of heart rate by the autonomic nervous system: studies in man on the interrelation between baroreceptor mechanisms and exercise. Circ Res 1966; 19:400-11 17 Atwood JE, Myers J, Sandhu S, Lachterman B, Friis R, Oshita A, et al. Optimal sampling interval to estimate heart rate at rest and during exercise in atrial fibrillation. Am J Cardiol 1989; 63:45-8 18 Neutel JM, Smith DHG, Graettinger WF, Weber MA. Heredity and hypertension: impact on metabolic characteristics. Am Heart J 1992; 124:435-40 19 Neutel JM, Smith DHG, Graettinger WF, Weber MA. Depen- dency of arterial compliance on circulating neuroendocrine and metabolic factors in normal subjects. Am J Cardiol 1992; 69:1340-44 20 Hammond HK, Froelicher VF. Normal and abnormal heart rate responses to exercise. Progress Cardiovasc Dis 1985; 27:271-96 A Practicum: Exercise Testing and Interpretation March 23 - 25, 1995; Harbor-UCLA Medical Center, Torrance, California Sponsored by the Division of Respiratory and Critical Care Physiology and Medicine, Harbor-UCLA Medical Center. Contact: Shirley Zagala, Box 405, Harbor-UCLA Medical Center, RB2, Room 319, 1000 W. Carson Street, P.O. Box 2910, Torrance, CA 90509-2910. Tel: 310 222-3803. CHEST / 107/21 FEBRUARY, 1995 Downloaded From: http://journal.publications.chestnet.org/pdfaccess.ashx?url=/data/journals/chest/21708/ on 05/02/2017 345