* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinical Concept of Heart Failure
Baker Heart and Diabetes Institute wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Rheumatic fever wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
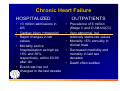
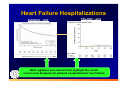
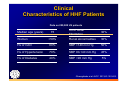
Clinical Concept of Heart Failure Mihai Gheorghiade MD, FACC Professor of Medicine and Surgery Director of Experimental Therapeutics Center for Cardiovascular Innovation Northwestern University Feinberg School of Medicine FDA’s View -Treat the Disease instead of the Condition “Heart Failure is not a disease and we should no longer approve drugs for a heterogeneous broad population, but for a well defined sub-population where we can demonstrate a marked benefit” Dr. Stephen Grant Deputy Director, Division of Cardiovascular Renal Products, CDER ACC/AHA 2009 Guideline: Classification of HF Stage Patient Description A High risk for(60mil.) •• • developing HF HTN CAD Diabetes mellitus B C D MI Asymptomatic HF •• Previous LV systolic dysfunction • Asymptomatic valvular disease 10 mil. • Known structural heart disease Symptomatic HF • Shortness of breath and fatigue • Reduced exercise tolerance 5 mil. • Marked symptoms at rest despite Refractory maximal medical therapy (eg, those who are end-stage HF(200000) recurrently hospitalized or cannot be safely discharged from the hospital without specialized interventions) Hunt SA et al. J Am Coll Cardiol. 2009. Congestive Heart Failure • Congestive heart failure (CHF) is a lifethreatening condition in which the heart isn't able to pump enough blood to the rest of the body. The failing heart continues to work, but not as efficiently as it should. Many conditions that lead to congestive heart failure can't be reversed, but heart failure can often be treated with medications and lifestyle changes. Case Study • • • • 51 year-old Elecrophysiologist Functional Class III for 6 months BP 90/60 mmHg; PCWP 30 mmHg; LVEF 10% Angiogram: no significant coronary disease; MRI: no hyper-enhancement (no scar tissue) • Receiving: furosemide, digoxin, enalapril • Started on carvedilol 3.125 mg BID that was titrated to 25 mg BID in addition to micro and macronutrients • 6 months later: – EF 60% – Functional Class I Bruce Bruce H H AJC AJC 2005 2005 Improve HF Viable but Dysfunctional Myocardium: Possibility for Recovery Etiologic Factors Ischemia/Hibernation Neurohormones (e.g. NE) Myocyte Cytokines (e.g. TNF a) Hemodynamics Metabolic Gheorghiade M. JACC 2009 Metabolism Needs The human heart weighs between 200-425 g This relatively small mass uses more energy, in the form of adenosine triphosphate (ATP), than any other organ It pumps 5 liters of blood per minute, 7200 liters per day, and over 2.6 million liters per year Over 6 kilograms of ATP is hydrolyzed by the heart daily undergo constant turnover and rebuilding. Every 30 days, an entire heart itself is reconstructed with brand new protein components Soukoulis et al JACC 2010 Chronic Heart Failure HOSPITALIZED • >3 million admissions in US • Cardiac injury (+troponin) • Rapid changes in lab values • Mortality and re hospitalization as high as 15% and 30%, respectively, within 60-90 after d/c • Event rate has not changed in the last decade OUTPATIENTS • Prevalence of 6 million (Stage C and D AHA/ACC) • Very abnormal, but relatively stable lab values • Mortality <5% annually in clinical trials • Decreased morbidity and mortality in last two decades • Death often sudden Hospitalizations for HF • Worsening chronic heart failure (HF):80% of all admissions* *The majority managed by non cardiologist • Acute de novo heart failure (diagnosed for the first time) :15% • Advanced/end-stage/refractory HF:5% Gheorghiade et al Circulation 2005 Heart Failure Hospitalizations EVEREST - HHF TRILOGY - ACS Both registries and clinical trials highlight the unmet need in new therapies for patients hospitalized for heart failure. Clinical Characteristics of HHF Patients Data on 200,000 US patients Median age (years) 75 Hx of Atrial Fibrillation 30% Women >50% Renal abnormalities 30% Hx of CAD 60% SBP >140 mm Hg 50% Hx of Hypertension 70% SBP 90-140 mm Hg 45% Hx of Diabetes 40% SBP <90 mm Hg 5% Gheorghiade et al JACC 2013;61:391-403. Admission Systolic BP and Outcomes in Hospitalized Patients With HF: An OPTIMIZE-HF Analysis Characteristic % (SD) Mean Age, y ≤119 Admission SBP mmHg 120-139 140-161 ≥161 (n=12,252) (n=12,096) (n=12,099) (n=12,120) 72.9 (14.0) 74.0 (13.5) 73.8 (13.6) 72.1 (14.6) Mean EF (%) 33.3 (17.4) 37.8 (17.6) 40.9 (17.1) 44.4 (16.5) Ischemic Etiology 50.7 48.8 44.1 39.2 HTN Etiology 13.4 18.1 25.4 34.8 Serum Cr>2 (mg/dl) 20.7 18.0 18.1 21.5 Mean Wt change (kg) -2.45 (5.00) -2.68 (4.82)-2.60 (4.64)-2.42 (4.62) Edema Admission 63.9 65.1 65.6 63.9 Total mortality in-hospital 7.2 3.6 2.5 1.7 Total mortality 60-90d 14.0 8.4 6.0 5.4 Readmission 30.6 29.9 30.3 27.6 Mean LOS, days 6.5 (6.6) 5.7 (5.3) 5.4 (5.0) 5.1 (4.8) Gheorghiade M et al. JAMA. 2008;299:2656-66 Hibernating Myocardium In an experimental study of short-term hibernation, dobutamine infusion resulted in myocardial infarction (right) when subendocardial blood flow was further reduced from 0.17 mL/min per gram (right). With and Without indicate with and without infarction. Reproduced with kind permission of Professor Gerd Heusch, Essen, Germany. Hospitalization for Heart Failure(HHF) • Improving post-discharge mortality and prevention of readmissions are the most important goals for HHF patients. Treat Beyond Clinical Congestion. The main reason for admission and readmission among patients Although this goal is often accomplished, some patients may be discharged with high left ventricular filling pressures as illustrated by high circulating natriuretic peptide levels, orthopnea, and poor exercise capacity. A more aggressive strategy to treat “subclinical” congestion may potentially improve outcomes. Gheorghiade and Braunwald JAMA 2012 Adopt a Mechanistic Approach to Cardiac Abnormalities. Heart failure is not a disease, but a manifestation of different cardiac abnormalities. Accordingly, an in-depth systematic assessment should be conducted of cardiac abnormalities (eg, valvular disease, cardiac dyssynchrony,ischemia). Gheorghiade and Braunwald JAMA 2011 Pang,Komajda,Gheorghiade EHJ 2010 Treat Noncardiac Comorbidities. The increasing rates of important non cardiac comorbidities, including hypertension and renal dysfunction, over the last decade, highlight the importance of targeting these conditions in the overall management of HF. In addition, diabetes, chronic obstructive pulmonary disease, and sleep apnea may also contribute to this high event rate after hospitalization. Gheorghiade and Braunwald JAMA 2011 Augment Use of Underused Agents Known to Decrease Hospitalizations. The use of digoxin is on a steep decline and mineralocorticoid antagonists are underused in patients with HF in the United States. DIG trial showed that use of digoxin reduced overall hospitalization rate by almost 30%, EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure) trial revealed that compared with placebo, use of eplerenone reduced all-cause hospitalization by almost 25%. Gheorghiade and Braunwald JAMA 2011 Results by high-risk patients subgroups: HF Hospitalization or HF mortality in DIG Trial % (events/total) NYHA class III or IV LVEF <25% CTR >55% High risk (either of the above) Placebo Digoxin 40% (445/1105) 39% (444/1129) 40% (465/1170) 36% (783/2167) 29% (329/1118) 27% (304/1127) 29% (336/1175) 26% (566/2191) Absolute risk difference – 11% – 12% – 11% – 10% Hazard ratio (95% CI) 0.65 (0.57–0.75) 0.61 (0.53–0.71) 0.65 (0.57–0.75) 0.66 (0.59–0.73) P value <0.001 <0.001 <0.001 <0.001 Gheorghiade et al, LBCT ESC HF Belgrade 2012 Translating the Basic Knowledge of Mitochondrial Functions to Metabolic Therapy Mitochondrial dysfunction is at the basis of a constellation of metabolic abnormalities that significantly contribute to Chronic conditions and diseases. Summary Myocardium as a main target for therapy Hospitalized Heart Failure (HHF) Practical consideration to improve HHF outcomes