* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download A Quick Tour Through: Endocrinology
Survey
Document related concepts
Transcript
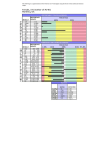
A Quick Tour Through: Endocrinology Veronica Piziak MD,PhD Scott & White • • • • Obesity New medications and surgical outcomes Hirsutism – evaluation and management Disclosures: none 2010 2006 1990 Prevalence* of Self-Reported Obesity Among U.S. Adults 2011 *us years. 30.4 15%–<20% 20%–<25% 34.9 25%–<30% Obesity = BMI >/=30 30%–<35% ≥35% 17% OBESE Therapy Old and New Combination Therapy (Qsymia) • A combination of phentermine, a sympathomimetic amine anorectic, and topiramate extended-release, an antiepileptic drug, indicated as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults initial body mass index (BMI) of: • • 30 kg/m2 or greater (obese) • • 27 kg/m2 or greater (overweight) in the presence of at least one weight-related comorbidity such as hypertension, type 2 diabetes mellitus, dyslipidemia Combination Therapy • Phentermine and Topiramate extendedrelease • Phentermine - enhancing the effect of dopamine • Topiramate - enhances the activity of GABA in the brain creates a feeling of fullness • Patients on the highest dose of lost an average of 10.6% of their starting body weight. • Weight loss persists at two years if drug continued Phentermine/Topiramate • Recommended dose: P/T 3.75 mg/23 mg daily for 14 days; then increase to 7.5 mg/46 mg daily • Discontinue or escalate dose if 3% weight loss is not achieved after 12 weeks on 7.5 mg/46 mg dose • Maximum daily dose of 15 mg/92 mg Discontinue P/T if 5% weight loss is not achieved after 12 weeks on maximum dose. • Discontinue 15 mg/92 mg dose gradually to prevent possible seizure Phentermine/Topiramate • Increase in Heart Rate: Monitor heart rate in all patients, especially • those with cardiac or cerebrovascular disease • Suicidal Behavior and Ideation: Monitor for depression or suicidal • thoughts. Discontinue if symptoms develop. • • Acute Myopia and Secondary Angle Closure Glaucoma: • Discontinue. Phentermine/Topiramate • Fetal Toxicity: Females of reproductive potential: • Obtain negative pregnancy test before treatment and monthly thereafter; use • effective contraception. • P/T is available through a limited • program under a Risk Evaluation and Mitigation Strategy (REMS) Phentermine/Topiramate • • • • • Mood and Sleep Disorders: Consider dose reduction or withdrawal for clinically significant or persistent symptoms. Cognitive Impairment: May cause disturbances in attention or memory. Caution patients about operating automobiles or hazardous machinery when starting treatment. • Metabolic Acidosis: Measure electrolytes before/during treatment • Elevated Creatinine: Measure creatinine before/during treatment • Use of Antidiabetic Medications: Weight loss may cause • hypoglycemia. Measure serum glucose before/during treatment Phentermine/Topiramate Drug Interactions • • Oral contraceptives: Altered exposure may cause irregular bleeding but not increased risk of pregnancy. Advise patients not to discontinue oral contraceptives if spotting occurs. • CNS depressants including alcohol: Potentiate CNS depressant effects. Avoid concomitant use of alcohol. • Non-potassium sparing diuretics: May potentiate hypokalemia. • Measure potassium before/during treatment Lorcaserin (Belviq) • A serotonin 2C receptor agonist indicated as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults • Initial body mass index (BMI) of: • • 30 kg/m2 or greater (obese) • • 27 kg/m2 or greater (overweight) in the presence of at least one weight-related comorbid condition • hypertension, dyslipidemia, type 2 diabetes Lorcaserin (Belviq) • Dosage: One tablet of 10 mg twice daily • Discontinue if 5% weight loss is not achieved by week 12 • Contraindicated in pregnancy • Do not use with other weight loss medications. • Monitor for hypoglycemia in diabetes Lorcaserin (Belviq) • Binds to serotonin receptors in the brain to increase satiety but much greater affinity for brain receptors then heart receptors. • Valvular heart disease: If signs or symptoms develop consider discontinuation and evaluate the patient for possible valvulopathy. • Study participants were monitored closely for heart valve irregularities, and no difference was seen in the two groups Lorcaserin Side Effects • Most common adverse reactions • (greater than 5%) • Non-diabetic: headache, dizziness, fatigue, nausea, dry mouth, constipation • Diabetic patients: hypoglycemia, headache, • back pain, cough, and fatigue Lorcaserin Side Effects • Cognitive Impairment: May cause disturbances in attention or memory. • Caution with use of hazardous machinery. • Psychiatric Disorders, including euphoria and dissociation: • Monitor for depression or suicidal thoughts. • Priapism: Patients should seek emergency treatment if an erection lasts >4 hours Lorcaserin- Drug Interactions • Serotonergic drugs use with extreme caution due to the risk of serotonin syndrome • Selective serotonin reuptake inhibitors (SSRIs) • Serotonin-norepinephrine reuptake inhibitors (SNRIs) • Monoamine oxidase inhibitors (MAOIs) Triptans, Bupropion, Dextromethorphan, St. • John’s Wort, lithium, tramadol Lorcaserin • About half of obese people who took the drug for a year lost at least 5% of their body weight, compared to 20% of dieters who took a placebo • 1 in 5 Lorcaserin users lost 10% or more of their body weight, compared to 1 in 14 placebo users. • People on medication for two years were able to maintain their weight loss better than those who switched to placebo after one year. NEJM 7/2010 Surgery Comorbid conditions • • • • • • • Sleep apnea Hypertension Type 2 diabetes Dyslipidemia Fatty liver GERD Metabolic syndrome Lap Band Long Term • No malabsorption / Weight loss more user dependent • At 2 years percentage of excess weight loss was 47.5% • 12 year follow up from Univ of Penn >50% revisions • Medical outcomes: • Hypertension: 25.6% at baseline, 29.5% at follow-up • Type 2 diabetes: 6.4% at baseline, 14.1% at follow-up • Treatment for obstructive sleep apnea: 2.6% at baseline, 7.7% at follow-up • Himpens J, et al Long term outcomes of laparoscopic adjustable gastric banding Arch Surg 2011 Which is better? • Gastric bypass – more complications, malabsorption, vitamin deficiency • 2 years 61.6% excess weight lost • 6 years 76% still maintained a 20% weight loss • 62 % of patients with diabetes were still in remission • Development of diabetes: 2% surgery group • 15% control group • LDL, HDL and triglycerides all significantly improved over control P<0.001 • Adams et al JAMA 2012;308:1122 (prospective Utah bases study) Gastric bypass is better! • 8 years, 83% of patients with preoperative T2DM had normal levels of plasma glucose, • Hypertension - not different • Sleep apnea – not resolved in most • Dyslipidemia improved in majority • .Can J Surgery. 2013 Feb;56(1):47-57. Gastric sleeve gastrectomy Sleeve Vs Gastric Bypass • Same comorbidity resolution at 1 year • Surgery 11/12 • Sleep apnea 58% • Diabetes 58% • Dyslipidemia 63% • Hypertension 38% • No resolution of GERD • Vidal et al Obesity Zhang et al Surg Endosc 2012,Dec 13 Hirsutism Approach to Hirsutism Type of Hair Vellus hair is short, soft, and lightly pigmented. Terminal hair is longer, stiff, and pigmented. Scalp hair is an example of terminal hair. Distribution Female terminal hair pattern lacks temporal balding and terminal facial hair other than on the upper lip and chin and eyebrows • Amount of Hair, Duration of the condition • • • • • • Approach to the Patient with Androgen Excess • Hormones of interest: Testosterone (5α-reductase) Dihydrotestosterone (DHT) (DHEA) – adrenal • Increased levels lead to hirsutism, which is excessive androgenic hair growth in a female pattern. • Virilization result from higher levels of hormone or prolonged stimulation with modest elevations. • Developing a male hair pattern, increased • pectoral musculature, and huskiness of the voice. • voice change, changes in libido, and clitoromegaly. • Must exclude tumors. Approach to Hirsutism • “In the United States, the “ideal” woman has, no terminal hair except for the scalp, eyebrows, eyelashes, and pubis. • This standard puts most, normal women in the hirsute category.” • Etching from the 14th century Lynn Loriaux Therapy for Hirsutism • Determine the degree of patient concern • Cosmetic procedures • Hair Growth Attenuation • Eflornithine (Vaniqa) • Cream is applied topically twice daily. 70% of women have a favorable response compared to control subjects Treatment • Treat the underlying Problem • Antiandrogens • • • • • Spironolactone 100 and 200 mg/day. Side effects mild diuretic effect,postural hypotension and hyperkalemia. High incidence of menstrual irregularity Coadministration of an estrogen/progestin-based birth control pill. Contraception is necessary • Finasteride 5 and 7.5 mg/day is an inhibitor of type II 5- reductase. There are no reported serious complications with this • medication in the treatment of hirsutism. • Contraception should be used Hirsutism Annoying Facial Hair Distribution is important Pathological Hair Distribution Frequently associated with virilization and tumors Case 1 • 18 yo lady comes to your office for amenorrhea and excess hair growth on her face and thinning of the hair on her head worsening over about the last two years. • She was told when she was a child that she might have a problem with her adrenal glands and she takes hydrocortisone 10 mg in the AM and 5 mg in the PM • Family history is positive for early puberty in males • On exam Blood pressure 120/70 BMI 25 Congenital Adrenal Hyperplasia ACTH high • • • • • • • low Most commonly partial 21 hydroxylase deficiency Measure Androstenedione And Testosterone Therapy: increase hydrocortisone Case 2 • 28 yo lady with progressive hirsutism over three months, • Deepening of her voice, “hot spells/headaches” • Enlarging upper body muscles secondary to weight training (virilization). Amenorrhea • 20 pound weight gain over last 4 months • BP 160/100 p 76 • Severe terminal hair hirsutism • What lab would you like to order? What lab would you like? • Abnormal menses, terminal hair hirsutism • Measure testosterone less then 200 ng/dl --benign • greater then/= 200 ng/dl --• adrenal or ovarian tumor • Remember the time course --- Case 2 Our patient Testosterone 400ng/dl Differentiating the adrenal from the ovary Exclude adrenal causes Measure adrenal steroids DHEA 4x normal Cortisol (24 hour urine) 10 x normal ACTH below assay limit MRI abdomen large left adrenal tumor with multiple metastases • Adrenal carcinoma • • • • • • • •