* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Microbes and diseases: what to study-1
Survey
Document related concepts
Staphylococcus aureus wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
Neglected tropical diseases wikipedia , lookup
Infection control wikipedia , lookup
Molecular mimicry wikipedia , lookup
African trypanosomiasis wikipedia , lookup
Onchocerciasis wikipedia , lookup
Transmission (medicine) wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Schistosomiasis wikipedia , lookup
Coccidioidomycosis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Gastroenteritis wikipedia , lookup
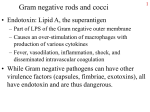
Transcript
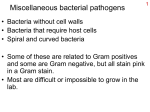
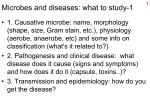
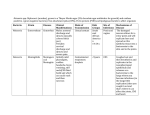
Microbes and diseases: what to study-1 1 • 1. Causative microbe: name, morphology (shape, size, Gram stain, etc.), physiology (aerobe, anaerobe, etc) and some info on classification (what's it related to?) • 2. Pathogenesis and clinical disease: what disease does it cause (signs and symptoms) and how does it do it (capsule, toxins..)? • 3. Transmission and epidemiology: how do you get the disease? Microbes and diseases: what to study-2 • 4. Diagnosis: How does the lab usually identify the causative agent? • 5. Treatment: antibiotics prescribed (or not- no cell wall, no penicillin) or other treatment (oral rehydration therapy for cholera). • 6. Prevention and control (stop the spread; condoms, kill urban rats..) 2 Staphylococcus: G+ coccus 3 • S. aureus and S. epidermidis. – S. aureus much worse, S. epi an opportunist. – Sturdy, salt tolerant, fac anaerobes; clusters – S. epidermidis common on skin, S. aureus less. • Diseases of S. aureus – Food poisoning, skin diseases (impetigo, folliculitis, furuncles & carbuncles, scalded skin syndrome), systemic diseases (TSS, bacteremia, heart, lung, and bone infections) – Diseases spread by fomites and direct contact. Characteristics of S. aureus infections 4 tray.dermatology.uiowa.edu/ DIB/SSSS-002.htm www.omv.lu.se/.../ rorelse/popup/01d1x.htm S. aureus virulence factors & Rx 5 • Coagulase, triggers blood clotting. • Capsules, beta-lactamases (destroy penicillins) • Toxins: various, including TSS toxin, exfoliatin, and enterotoxins (heat stable) • 95% resistant to penicillin, but now many resistant to methicillin, oxacillin. Treatment usually clindamycin (oral) or vancomycin (IV). http://www.biology4kids.com/extras/dtop_micro/7821_580.jpg Streptococci: G+ cocci • Genera: Streptococcus and Enterococcus • Aerotolerant anaerobes, catalase negative – Grow in chains, pairs – Strep: Lancefield groups, viridans, S. pneumoniae • Group A strep: S. pyogenes – Pharyngitis, scarlet fever, pyoderma, erysipelas, TSS, necrotizing fasciitis – Sequelae: rheumatic fever and glomerulonephritis http://genome.microbio.uab.edu/strep/info/strep5.gif 6 Characteristics of Streptococcal infections http://euclid.dne.wvfibernet.net/~jvg/Bio208/resp_pix/scarlet-fever.jpg http://textbookofbacteriology.net/vvpath.jpeg 7 Virulence factors, etc. • S. pyogenes (“pus-producing”) – M protein and capsule: avoids phagocytosis – Streptokinase, streptolysins for escape & attack – Pyrogenic erythrotoxins (SPEs) • at least 3 different types • Cause scarlet fever: fever, rash; toxic shock – Beta hemolytic on blood agar • Viridans group: greenish alpha hemolysis – Common in throat, mouth, but can be opportunists – S. mutans associated w/ dental caries 8 Clostridium: G+ rods 9 • Strict anaerobes! Endospore formers. Toxigenic – Common in soil, sewage animal GI tracts – Produce neurotoxins, enterotoxins, histolytic toxins • Four important species: C. perfringens, C. botulinum, C. tetani, and C. difficile. • C. perfringens – Food poisoning: cramps and diarrhea – From injury: myonecrosis to gas gangrene • Fermentation in tissues, killing of tissues and spread of cells into anaerobic areas. • Oxygen treatment, debridement, amputation More clostridia 10 • C. difficile: normal GI microbiota – Cause of pseudomembranous colitis, resulting from overgrowth following broad spectrum antibiotics • Damage to GI wall can lead to serious illness – Nosocomial infection, easily transmitted • C.botulinum: cause of botulism – Usually acquired by ingestion: intoxication • Food borne, infant (no honey), wound – Produces neurotoxin, inhibits acetylcholine release • Flaccid paralysis; Botox: deadly poison / beauty – Mouse bioassay; administer antitoxin Opposing muscle groups When biceps contracts, triceps relaxes. When triceps contracts, biceps relaxes. Excitatory neurons send signal to contract, inhibitory neurons send signal to NOT contract. http://upload.wikimedia.org/wikipedia/sv/thumb/d/dd/185px-Muscles_biceps_triceps.jpg 11 Function of nerves 12 http://upload.wikimedia.org/wikipedia/fr/thu mb/e/e4/200px-Synapse.png http://www.people.virginia.edu/~dp5m/phys_304/figures/motor_unit.jpg More clostridia-2 • C. tetani: cause of tetanus – Growth in anaerobic wounds, makes tetanus toxin – Toxin prevents action of inhibitory neurons • Opposing muscle pairs both contract • Spastic paralysis, leading to death. – Recommendation is booster shot every 10 years • DPT, Toxoid vaccine • Booster: DT (with diphtheria toxoid) • No natural immunity: you would die first. 13 Mycobacterium: G+ rods • Many non-pathogenic species, most disease: M. tuberculosis and M. leprae – Mycolic acids as part of complex cell wall • Protects against desiccation • Protects against destruction by phagocytes • Requires acid-fast staining – Generally grow very slowly (chronic illnesses) – Can grow intracellularly 14 Acid Fast stain of Mycobacteria http://www.md.huji.ac.il/mirror/webpath/AIDS071.jpg 15 M. tuberculosis 16 • Causes disease tuberculosis, mostly lung dis. • Disease: cells enter lungs, infect macrophages – Macrophages not activated, can’t kill invader – Cell mediated immunity fights back, walls off infection; forms tubercle (caseous necrosis occurs) – Disease remains controlled, cured, or returns • Disseminated TB: spreads thru body • Worldwide problem; lowered immunity=risk – Skin test, chest x-ray, drug treatment, vaccine? M. leprae • Cause of Hansen’s disease, aka leprosy • Slow growing, likes it cool; armadillos as model • Grows in peripheral nerve and skin cells – Numbness is characteristic of disease • Tuberculoid vs. lepromatous leprosy – Mild, severe, respectively, depending on cell mediated immune response. – Numbness vs tissue destruction • Spread mostly by direct contact • Treatable with antibiotics, but long term 17 Gram negative rods and cocci 18 • Endotoxin: Lipid A, the superantigen – Part of LPS of the Gram negative outer membrane – Causes an over-stimulation of macrophages with production of various cytokines – Fever, vasodilation, inflammation, shock, and disseminated intravascular coagulation • While Gram negative pathogens can have other virulence factors (capsules, fimbriae, exotoxins), all have endotoxin and are thus dangerous. Enterobacteriaceae: Gram negative rods 19 • Gram negative, small rods, facultatively anaerobic, oxidase negative; found in soil, water, and GI tracts – some strictly pathogens, others opportunists – Coliforms (ferment lactose) and non-coliforms • Virulence factors – Endotoxin, capsules, fimbriae, exotoxins, others. • Enteric bacteria identified by biochemical tests – Selective/differential media, IMViC tests, etc. – Strains identified by serological techniques Serology and enteric bacteria 20 • Because enteric bacteria are very closely related to each other, differentiation requires serology – Use of antibodies to identify particular antigenic molecules on cell surfaces – O antigen: repeating sugar group on LPS – H antigen: flagellar protein – K antigen: capsule antigen around cell. – Example: E. coli O157:H7 describes particular serotype which happens to also produce a dangerous exotoxin. 21 http://www.ratsteachmicro.com/Assets/Enterobacteriaceae/Enterobact_diagra m2.gif E. coli: friend or foe? 22 • E. coli: cause of 90% of urinary tract infections – Most strains common to GI tract, not harmful there. – Strains have fimbriae needed for attachment – Proanthocyanidins in cranberry juice interfere • E. coli: common cause of diarrhea – Many strains possess genes (some on plasmids) that code for additional virulence factors like exotoxins which cause disease • E. coli O157:H7: possesses shiga toxin; strain causes hemolytic uremia syndrome, damages kidneys. • E coli strains classified as EHEC, EIEC, EPEC, etc. – Enterohemorrhagic, enteroinvasive, etc. Truly pathogenic enterics 23 • Salmonella: species so closely related that they are really all S. enterica. But medically, species epithets still used: S. typhi and others. Divided serologically. – Present in eggs, poultry, on animals such as reptiles – Large dose results in food poisoning; diarrhea, fever, etc. – Cells phagocytized by intestinal lining cells, kill cells causing symptoms, may pass through into blood. – S. typhi: typhoid fever. Spread through body • Gall bladder as reservoir; Typhoid Mary • Importance of clean water and sewage treatment. • http://www.newsday.com/community/guide/lihistor y/ny-history-hs702a,0,6698943.story Truly pathogenic enterics-2 24 • Shigella: especially S. sonnei (most common) and S. dysenteriae (most serious); cause shigellosis. – Food, flies, fingers, feces, fomites: very small infectious dose, personal hygiene important in prevention. – Infection of intestinal lining damaged, cells pass directly from cell to cell; cramps, diarrhea, bloody stools. – S. dysenteriae produces shiga toxin which inhibits protein synthesis, increases damage. – Most serious problem with diarrheal diseases in general is dehydration. Truly pathogenic enterics-3 25 • Yersinia: Y pestis is cause of plague, other species cause food-borne infections • Plague: 3 cycles: sylvan, urban, and human – endemic in sylvan cycle; mixing of woodland and urban rodents brings urban cycle, fleas jump from dying rats to humans. – Infection leads to large swollen lymph nodes: buboes • Bubonic plague, with high fever. • Septicemic plague: with DIC, bruising (black death) – Raises mortality from75% to near 100% • Pneumonic: coughed out and spread human to human – 100% mortality The S.F. earthquake and plague http://library.thinkquest.org/03oct/00904/images/sanf.jpg http://www.cdc.gov/ncidod/dvbid/plague/plagwest.htm 26 Other Gram - rods • Francisella: F. tularensis, cause of tularemia – – – – Also called rabbit fever, tick fever, deerfly fever, etc. Most cases in US in Arkansas/Missouri Ozarks Survives phagocytosis, lives intracellularly Present in many animals, transferred to humans by vector, ingestion, direct contact, inhalation – Chills, fever, malaise, swollen nodes http://er1.org/docs/photos/Tularem ia/Amblyomma%20Americanum% 20(lone%20star%20tick).jpg http://mercury.bio.uaf.edu/ ~george_happ/Francisella. jpg 27 Other Gram – rods-2 28 • Legionella: L. pneumophila and several others – Fastidious in culture, requires special media – Very common in aquatic environments: ponds, cooling towers, hotwater heaters, showers. – Grows normally in amoebae, so also grows in phagocytes – Most dangerous as opportunistic pneumonia, inhalation – Mild form of disease: ‘pontiac fever’ www.angelfire.com/.../ bicentennial.html Chlamydia • Very small, obligate intracellular parasites – Cell and outer membrane, but no peptidoglycan • Spread directly rather than by vectors • Two stage life cycle – Elementary body: tiny (0.2-0.4 µm) and inert • Spore-like: dormant and resistant • Infectious: form that moves between cells – Reticulate body: 0.6-1.5 µm, metabolically active, reproduce inside host cells 29 Chlamydial diseases • C. trachomatis: infects cells of mucous membranes, conjunctiva. Mostly eye & STD – Infection kills cells, stimulates inflammation which also causes cell destruction • Trachoma- leading cause of non-traumatic blindness. Caused by certain strains. – Infection of conjunctiva causes scarring, turning in on eyelashes which scratch cornea. – Scarred cornea, with ingrown blood vessels, obscure vision. – STD strains can also infect eyes, self-inoculation. 30 Sexually transmitted Chlamydial disease 31 • Non-gonococcal urethritis, about 50% of cases • Chlamydia infections are the most common STD, but even more are infected and asymptomatic – 85% of women asymptomatic; others can develop PID; scarring of uterine tubes can lead to sterility, ectopic pregnancy. • Eye infections of newborns prevented with antibiotic drops. – Also protects against N. gonorrhoeae Gram negative curved rods 32 • Vibrio: comma shaped – Like enteric but oxidase positive; polar flagella – Halotolerant to halophilic, grow in estuarine and marine environments – V. cholerae: cause of cholera • Toxin-mediated severe diarrhea • Salt, fluid leave intestinal cells, patient dies of dehydration. • Oral rehydration therapy (ORT): water, salts, and glucose, now saving lives. • Causes pandemics that spread around the world – Lack of adequate sewage treatment Campylobacter • Campylobacter jejuni: number one cause of bacterial gastroenteritis; zoonotic – More common than Salmonella and Shigella combined for food borne disease. – Most retail chickens are contaminated; improperly cooked chicken and contaminated milk typical vehicles. – Low infectious dose – Gram neg. curved rod http://www.shef.ac.uk/staff/newsletter/vol23no10/image s/campylobacter.gif 33 Helicobacter pylori • Cause of ulcers and gastritis – 2005 Nobel Prize for Medicine or physiology to Barry Marshall and J Robin Warren – Unusual because it can live in stomach – Produces urease enzyme • Released ammonia neutralizes stomach acid, irritates stomach lining. • Basis for radioactive urease test. – Correlated with stomach cancer. http://s99.middlebury.edu/BI330A/STUDENTS/KASSIS/images/pylori1b.jpg 34