* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Mechanisms of Activation of Cardiac Glycogen Phosphorylase in
Survey
Document related concepts
Transcript
Mechanisms of Activation
of Cardiac Glycogen Phosphorylase
in Ischemia and Anoxia
By James G. Dobson, Jr., and Steven E. Mayer
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
ABSTRACT
The effects of ischemia and anoxia on cardiac adenosine 3',5'-monophosphate (cyclic
AMP) concentration, glycogen phosphorylase activity ratio (— 5'-AMP: + 5'-AMP),
phosphorylase kinase activity ratio (pH 6.8:8.2), and myocardial contractility (left
ventricular dP/dt) were studied in an open-chest rat heart preparation. Ischemia produced by termination of coronary blood flow increased cyclic AMP from 0.55 to
0.77 yu.moles/kg in 5 seconds and phosphorylase from 0.14 to 0.57 in 20 seconds. Anoxia
induced by breathing N., increased cyclic AMP from 0.50 to 0.62 ju.moles/kg in 10
seconds and phosphorylase from 0.14 to 0.65 in 30 seconds. Phosphorylase kinase increased with ischemia but did not change with anoxia. Beta-receptor blockade with
practolol prevented the rise in cyclic AMP and phosphorylase kinase but blocked the
increase in phosphorylase only in ischemia. Myocardial contractility declined precipitously during the first 20 seconds of anoxia. Epinephrine (0.1 |ixg/kg) caused an increase
in cyclic AMP comparable to that elicited by anoxia, and it produced an increase in
dP/dt during Na breathing. These results suggest that in the intact working heart
ischemia induces phosphorylase a formation through a cyclic AMP—dependent transformation of phosphorylase kinase; however, in anoxia phosphorylase a formation
depends only on the regulation of the catalytic activity of phosphorylase kinase without conversion of this enzyme to its activated form. An increase in cyclic AMP during
anoxia is not associated with a positive inotropic response even though such a response
is obtained with epinephrine. Factors other than the elevation of myocardial cyclic
AMP may be limiting in the control of both cardiac glycogenolysis and inotropic state.
KEY WORDS
glycogenolysis
adenosine 3',5'-monophosphate
phosphorylase kinase
contractility
epinephrine
rat heart
• The activation of glycogenolysis that occurs with
ischemia and anoxia in the myocardium results from
an increase in glycogen phosphorylase activity
(1-4). The increase in enzyme activity occurs very
rapidly, within approximately 10 seconds, and
appears to be largely due to the conversion of the
enzyme from the b to the a form (4-6). Epinephrine elicits activation of cardiac phosphorylase by a
sequence of reactions beginning with the production of adenosine 3',5'-monophosphate (cyclic
AMP) through the activation of adenylate cyclase
(7-9). The mechanism of action of cyclic AMP
appears to be the activation of protein kinase
(10). This enzyme catalyzes the adenosine triphosphate-dependent transformation of phosphoryFrom the Division of Pharmacology, Department of
Medicine, University of California, San Diego, La Jolla,
California 92037.
This investigation was supported by U. S. Public Health
Service Grants HE-50416 and HE-12373 from the National
Heart and Lung Institute.
Received July 10, 1973. Accepted for publication August
15, 1973.
412
practolol
lase kinase to its activated form. Phosphorylase
kinase catalyzes the phosphorylation of phosphorylase h, converting it to phosphorylase a. Thus
amplification is achieved through a series of
reactions that result in rapid and intense glycogen
utilization.
Ischemia in the nonworking heart causes an
increase in myocardial cyclic AMP concentration
and a subsequent formation of phosphorylase a by
the release of norepinephrine from cardiac stores
(6). However, it is not known if this mechanism is
the sole or the major one responsible for phosphorylase activation in the ischemic working heart, i.e., a
heart in which the myocardium continues to develop tension while coronary flow is interrupted. Since
anoxia-induced formation of phosphorylase a in the
heart is only slightly reduced by pronethalol, a
^3-adrenergic antagonist (4), or reserpine (3), activation of phosphorylase by oxygen deprivation appears to involve only minimal adrenergic participation. The mechanisms responsible for the activation
of glycogenolysis in the anoxic working heart are
not known.
Circulation Research, Vol. XXXI11, October 1973
413
MECHANISMS OF PHOSPHORYLASE ACTIVATION
The purpose of this investigation was to compare
the effects of ischemia and anoxia on the formation
of cyclic AMP and the transformation of phosphorylase kinase and phosphorylase to their activated
forms in the intact rat heart developing tension in
situ with the objective of demonstrating cyclic
AMP-dependent and cyclic AMP-independent
mechanisms controlling glycogenolysis. Since it has
been hypothesized that cyclic AMP participates in
the control of the inotropic state of the heart
(11-13), we also sought to correlate changes in
cyclic AMP concentration during anoxia with
measurements of the inotropic state of the myocardium.
Methods
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
OPEN-CHEST HEART PREPARATION
Male albino Sprague-Dawley rats weighing 225—325 g
were obtained from local suppliers and maintained on
nonmedicated Purina chow ad libitum in rooms with a
lighting sequence of 12 hours light and 12 hours dark.
The rats were anesthetized with sodium penlobarbital
{25 mg/kg, ip) and a-chloralose (50 mg/kg, ip). In
addition all rats received atropine sulfate (1 mg/kg, ip)
to suppress vagal responses in the heart. Body temperature was maintained at 37 ± 1°C. Aortic blood pressure
was continuously recorded from a saline-filled cannula
inserted in the left common carotid artery with a
Statham P23Db strain-gauge manometer. The left
jugular vein was cannulated for the administration of
drugs.
Acute bilateral adrenalectomy was performed in all
experiments to eliminate the influence of adrenal
catecholamines. The chest was opened, and the rat was
ventilated with 95% (X-5& CO, via a tracheal cannula
with a Harvard respirator (model 673) at 80/min.
Proper lung inflation was ensured by a side tube
connected to the inspiratory cannula that was submerged in a 15-cm column of water. The beating hearts
were frozen in situ by compressing them into thin (1-2
mm) wafers with silver clamps precooled in liquid
nitrogen 0-120 seconds after the onset of either ischemia
or anoxia (14).
Ischemia was introduced in the open-chest heart by
techniques producing either a working or a nonworking
preparation. In the working preparation the base of the
heart was cross-clamped with a hemostat. This
maneuver terminated coronary blood flow and maintained a constant ventricular volume by occluding
ventricular inflow and outflow. Consequently, the
myocardium continued to develop tension by contracting against a constant afterload. In the nonworking
preparation the descending aorta and the inferior vena
cava were severed cephalad to the diaphragm. Aortic
pressure fell to zero within 2—3 seconds. Anoxia was
produced without manipulation of afterload by substitution of the respiratory gas (95% O-2-5% CO2) with
100% N2.
In several rats in which N2 breathing was introduced,
arterial oxygen tension (Po 2 ) was recorded by a microCircuUlion Research, Vol. XXXIII, October 1973
oxygen electrode (IBC multi-purpose differential oxygen analyzer, model 145-071). The electrode was
inserted into the aorta via a common carotid artery so
that aortic blood flow was not restricted. The response
of the electrode to changes in Po2 was determined in
saline bubbled with O 2 . When the Po, was changed
abruptly from 300 to 1-2 mm Hg, the electrode recorded the change exponentially and required 15 seconds to
indicate a decrease in Po2 to 10 mm Hg.
In some open-chest preparations intraventricular
pressures were recorded through an 18-gauge stainless
steel cannula (1 cm in length) filled with heparinized
degassed saline inserted through the cardiac apex into
the left ventricle. The cannula and the pressure
transducer (Pitran pressure transistor, model PT22)
had a frequency response of 290 Hz. Left ventricular
dP/dt was derived from the left ventricular pressure
signal by resistance-capacitance differentiation. All
pressure and dP/dt data were recorded directly on
magnetic tape at 15 ft/min (Hewlett-Packard magnetic
recorder system, model 3955) and played back at 3.75
ft/min on a multichannel oscillograph (Sanborn series
7700 recorder).
ANALYTICAL PROCEDURES
Tissue Preparation and Extraction,—Cardiac muscle
samples were stored at —65°C prior to analysis. The
entire ventricles were finely powdered by percussion
with a stainless steel mortar and pestle. The samples
and the pulverization apparatus were previously cooled
in liquid nitrogen. The powdered samples were transferred to screw-cap glass vials and stored at —65°C
until they were assayed. Approximately 10 mg of the
powdered muscle was weighed and transferred to a
Duall homogenizing tube (size 20, Kontes Glass Co.)
in a room at —20°C. Fifty to one hundred volumes
(based on sample weight) of an ice-cold solution containing 20 iriM KF, 4 mM ethylenediaminetetraacetate,
20 mM /3-gIycerophosphate, and 20 mM ^8-inercaptoethanol (pH 6.8) was rapidly added; the mixture was
homogenized at 0°C. The homogenization was performed in 1—2 minutes with a motor driven pestle at a
speed of 100—200 rpm. The homogenate was centrifuged at 3000 g for 20 minutes, and the supernatant
fluid was assayed immediately for phosphorylase and
phosphorylase kinase.
Another 35-40-mg portion of the powdered muscle
was transferred to a Duall homogenizing tube (size 20);
it was homogenized and extracted as described elsewhere (15) for assay of cyclic AMP.
Chemical Assays.—Glycogen phosphorylase was
measured by the production of glucose-1-phosphate in
the absence and the presence of 5'-AMP (16). One unit
of phosphorylase is defined as the amount of enzyme
that produces 1 jj.mo\e of glucose-1-phosphate from
glycogen per minute at 30 c C. The results were expressed as the ratio of phosphorylase activity without
AMP to phosphorylase activity assayed with AMP. An
increase in the ratio indicates an increase in the conversion of phosphorylase b to phosphorylase a, which is
physiologically more active. Phosphorylase kinase was
assayed using the modification by Drummond and Duncan (17) of the method of Krebs et al. (18). The
DOBSON, MAYER
414
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
activity of the enzyme was measured by the production
of phosphorylase a from crystalline skeletal muscle phosphorylase b. The results were expressed as the ratio of
phosphorylase kinase activity measured at pH 6.8 to
that measured at pH 8.2. An increase in the activity
ratio of phosphorylase kinase indicates transformation
to the activated (phosphorylated) form of the enzyme.
Cyclic AMP was assayed by the method of Wasila et al.
(19), which is based on the activation of skeletal muscle
protein kinase.
Materials.—Z-Epinephrine bitartrate (Winthrop) and
d,l-ptacto\o\ (Ayerst Laboratories) were prepared
fresh daily in a 0.9% (w/v) sodium chloride solution
containing 0.2% (w/v) sodium metabisulfite. Nucleotides were obtained from P-L Biochemicals or Boehringer Mannheim Corporation. All enzymes used for the
phosphorylase kinase and phosphorylase assays and the
•y-:t-P-ATP synthesis were from Boehringer Mannheim
Corporation. Carrier-free ( 32 P) inorganic phosphate
was purchased from Schwarz Bio-Research. Phosphorylase b, containing less than 2% of the a form, was prepared as described by DeLange et al. (20).
Statistical Methods.—Statistical analyses were performed using Student's t-test for paired or unpaired
observations. A probability of < 0.05 was accepted as a
significant difference.
Results
ISCHEMIA
In the working heart ischemia produced an
increase in the myocardial concentration of cyclic
AMP and an activation of cardiac phosphorylase
(Fig. 1). The cyclic AMP concentration increased
O.B -
from 0.55 to 0.77 /unoles/kg 5 seconds after the
termination of coronary blood flow; it then rapidly
returned to control concentrations. The control
phosphorylase activity ratio was 0.14 and increased
to 0.34 after 10 seconds of ischemia and to 0.57
after 20 seconds of ischemia. Total phosphorylase
activity (fl + b) ranged from 14 to 18 units/g for all
hearts studied and did not change during ischemia.
The activation of phosphorylase followed the
elevation in cyclic nucleotide by 5 seconds. This
activation persisted throughout the ischemic period
unlike the transient activation observed in response
to epinephrine infusion (21). Practolol (5 mg/kg,
iv) prevented the increase in cyclic AMP concentration and the phosphorylase a formation. This dose
of practolol did not appreciably influence aortic
blood pressure (100-125 mm Hg), heart rate
(300-400/min), or myocardial contractility.
In the nonworking heart ischemia elicited an
increase in the cyclic AMP concentration from 0.50
to 0.62 ptmoles/kg in 20 seconds (Fig. 2). After this
initial increase and a return toward control, the
myocardial cyclic nucleotide concentration increased again and remained elevated. The phosphorylase activity ratio increased from 0.14 to 0.34
20 seconds after the initiation of ischemia by whole
rat circulatory arrest and increased further after
0.9 -i
PRACTOLOL Sme/tg
f
0.7 -
PRACTOLOL
c
0.8 -
s
5mg/Ag
0.6 0.5 -
06 -
0.1
0.6 -
Ul
0.1
< a.
_l
2
>• <t
0.1 -
IE +
Si
O- S
0.6 GO
0.2 -
^f-—l
1
<x a.
1—11-
0.1 -
0.0
20
25
30
60
s
0.2 -
?.,
I—HI—1
TIME-Seconds
FIGURE 1
Effect of ischemia on myocardial cyclic AMP concentration
and phosphorylase activity ratio in the working rat heart
in vivo. Ischemia was induced by clamping across the base
of the heart at time zero so that the heart continued to
develop tension. Each point represents the mean of at least
five experiments with (c) or without (s) practolol. The asterisks denote significant differences (P < 0.05) from time zero.
Bars represent ±1 SE.
0.0
0
10
20
30
10
50
60
120
TIME - Seconds
FIGURE 2
Effect of ischemia on myocardial cyclic AMP concentration
and phosphorylase activity ratio in the nonworking rat heart
in vivo. Ischemia was produced by severing the descending
aorta and inferior vena cava at time zero. See legend of
Figure 1 for further explanation.
Circulation Research, Vol. XXXIII, October 1973
MECHANISMS OF PHOSPHORYLASE ACTIVATION
60-120 seconds of ischemia. Again practolol blocked
the elevation in myocardial cyclic AMP and the
formation of phosphorylase a.
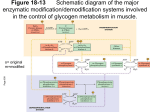
The phosphorylase kinase activity ratio increased
with ischemia from a control of 0.08 to 0.16 in the
working heart and to 0.12 in the nonworking heart
(Fig. 3). The activity of phosphorylase kinase was
highest at the time when the concentration of cyclic
AMP was increased. Total phosphorylase kinase
activity determined at pH 8.2 ranged from 95 to 120
units/g for all hearts and was not altered by
ischemia. The transformation of the enzyme to its
activated form was prevented by practolol. The f3adrenergic antagonist did not influence the control
kinase activity ratio.
ANOXIA
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
In the working heart anoxia caused an increase in
cyclic AMP concentration and an activation of
phosphorylase (Fig. 4). Cyclic AMP increased
significantly from a control value of 0.50 //.moles/kg
to 0.62//.moles/kg, 10 seconds after the substitution
of 100% N2 for 95% O2-5% CO, and returned
to control values at 15 seconds. This return was
followed by another increase that occurred after
X*
0.16
CO
NO
415
120 seconds of N2 breathing. An increase in the
phosphorylase activity ratio from 0.14 to 0.43
followed the transient elevation of cyclic AMP by 5
seconds. Thirty seconds after the onset of N2
breathing the ratio increased to 0.65 and remained
elevated. Practolol prevented the increase in cyclic
AMP but did not have any effect on the formation
of phosphorylase a. This finding is in contrast with
that observed during ischemia, since enzyme
activation was completely prevented by yS-recepto-r
blockade during ischemia. During anoxia the
phosphorylase kinase activity ratio did not differ
from control (Fig. 3), indicating that no covalent
transformation of the enzyme occurred with N2
breathing. Total phosphorylase and phosphorylase
kinase activities were not altered by anoxia or by
practolol.
Abruptly changing the respiratory gas mixture
from 95% O-t-5% CO. to 100% Na caused the arterial
Po-2 to decrease from 250-300 to 15 mm Hg in 15
seconds. The fall in arterial blood Po2 was slower
than the response time of the electrode. Thus the
Po2 of coronary arterial blood fell precipitously
during the time that cyclic AMP concentration was
augmented and the conversion of phosphorylase b
to a was initiated.
p-BL0CKtDE
0.8
PRACTOLOL 5mg/kg
0.14
1
5 0.12
cr
t
0.10
0.08
0.06
in 0.04
<t
_i
g o.oe
X
Q.
O
a.
0
T
0 7 -
s I I1
0.6 -
a.
5
0.5 -
0.4
0.8 •
-»•
a: £
a. S
ISCHEMIC
non-working
ANOXIC
working
FIGURE 3
Effect of ischemia and anoxia on phosphorylase kinase activity ratio in the rat heart in vivo. Ischemia was produced
by either clamping the base of the heart (working) or by
sectioning the abdominal aorta and the inferior vena cava
(nonworking). Anoxia was produced by respiration with
100% Ns (working). Samples for phosphorylase kinase determination were taken at the time of peak cyclic AMP concentration 5—20 seconds after onset of ischemia or anoxia.
See legend of Figure 1 for further explanation.
Circulation Research, Vol. XXXIII, October 1973
in •a.
O c
£
t—1*
0.6 •
3 1+
t
o
ISCHEMIC
working
5mg/kg
— r
e
UJ
to
CONTROL
PRACTOLOL
c
0.4 •
0.2
0.0
—I—I—I—I—I—I—I—
ZO
30
40
50
—r/y
€0
70
—I
120
TIME-Seconds
FIGURE 4
Effect of anoxia on myocardial cyclic AMP concentration
and phosphorylase activity ratio in the working rat heart in
vivo. Anoxia was produced by respiration with 100% N2
beginning at time zero. See legend of Figure 1 for further
explanation.
DOBSON, MAYER
416
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
Epinephrine caused an increase in myocardial
cyclic AMP concentration, phosphorylase kinase
transformation, and phosphorylase a formation in
the open-chest preparation (Table 1). The concentration of cyclic AMP increased from 0.50 to 0.64
/Ltmoles/kg 10 seconds after a bolus intravenous
injection of epinephrine (0.1 fig/kg). The phosphorylase activity ratio increased twofold above
control levels 15 seconds after injection. No
significant change in phosphorylase kinase was
observed. The elevations in both the cyclic AMP
concentration and the phosphorylase activity ratio
produced by this dose of epinephrine were similar
to the initial increases in cyclic nucleotide and enzyme activity elicited by ischemia or anoxia. Epinephrine (1.0 /J-g/kg) caused a greater increase in
the concentration of cyclic AMP and a marked
augmentation of phosphorylase kinase and phosphorylase activity ratios. Practolol alone did not
influence control cyclic AMP, phosphorylase kinase,
and phosphorylase but did prevent the elevation of
these three biochemical parameters following the
administration of epinephrine.
ANOXIA AND MYOCARDIAL CONTRACTILITY
During the first 20 seconds of N2 breathing in the
open-chest preparation myocardial dP/dt decreased
from 4800 to 2600 mm Hg/sec (Fig. 5). The small
increases at time zero are artifacts of switching the
respiratory cannulas and performing injections. In
the preparation ventilated wth 95% O2-5% CO2, a
bolus injection of epinephrine (0.1 /u,g/kg) produced
an increase in dP/dt from 4800 to 6000 mm Hg/sec.
When epinephrine (0.1 /Ag/kg) was injected 8 seconds after the introduction of anoxic respiration, a
significant increase in dP/dt above that caused by
N-j breathing alone was observed between 12 and 20
seconds. There was a greater increase in dP/dt
during anoxia with the administration of epinephrine (1.0 /^g/kg) 8 seconds after the onset of Na
breathing.
Discussion
ISCHEMIA
In both the working and the nonworking
ischemic heart, the increase in cyclic AMP concentration and the concomitant transformation of
phosphorylase kinase to its activated form that
occurred in 5-20 seconds were followed by an
increase in phosphorylase a (Figs. 1-3). A low dose
of epinephrine (0.1 /ig/kg) caused a similar
increase in cyclic AMP concentration and a similar
formation of phosphorylase a (Table 1). The /3adrenergic antagonist, practolol, prevented the
increase in cyclic AMP, the transformation of
phosphorylase kinase, and the formation of phosphorylase a produced by either ischemia or
epinephrine. Therefore, these results confirm that
the observed increase in cyclic AMP is of sufficient
magnitude to be largely if not totally responsible
for the transformation of phosphorylase kinase and
the activation of phosphorylase found in the
ischemic working heart. These results are essentially
in agreement with those of Wollenberger et al. (6).
With a nonworking dog heart made ischemic by
severing the aorta, these investigators reported an
increase in cyclic AMP and phosphorylase activation within a few seconds after the onset of
ischemia. However, in their experiments the cyclic
nucleotide concentration increased to a level twice
that of control, and the elevation was maintained
for 20-30 seconds. We observed a more transient,
TABLE
Effect of Epinephrine and Praciolol on Cyclic A M P Concentration, Phosphoryhusc Kinast, and Phosphorylase
Activity Ratios in the Myocardium of the Working Hal Heart
Cyclic AMP
(wmo!es/kg)
Control
Epinephrine (0.1 /ig/kg)
Epinephrine (1.0 ^g/kg)
Practolol (n mg/kg)
Practolol (5 mg/kg) and epinephrine (1.0 ,ug/kg)
0.50
0.64
1.75
0.46
0.52
±
±
±
±
±
0.01
0.03*
0.15*
0.05
0.06
Phosphorylase kinase
(pH 6.8/8.2)
0.08
0.10
0.14
0.08
0.09
±
±
±
±
*
0.01
0.02
0.02*
O.OJ
0.01
Pbosphorylase
(-AMP/+AMP)
0.14
0.28
0.73
0.13
0.16
=fc 0 01
± 0.02
* 0.03
* 0.01
± 0.03
Epinephrine was administered intravenously as a bolus (0.2 ml) to the working open-chest rat heart preparation ventilated with 9 5 ^ Oi-^% CO.. The myocardial cyclic AMP concentration and the phosphorylase kina.se
activity ratio were determined 10 seconds after the administration of epinephrine. The phosphorylase activity
ratio was determined lo .seconds after injection of the cateeholamine. All values represent the mean =*= 1 SK
of at least four hearts.
*P < 0.05.
emulation Research, Vol. XXXIII, October 191i
417
MECHANISMS OF PHOSPHORYLASE ACTIVATION
ischemie very quickly thereby causing a rapid
release in endogenous catecholamines. Cardiac
ischemia induced by coronary occlusion also
produces a marked increase in sympathetic nerve
activity which occurs in less than 1 second (22).
Ischemia of the central nervous system elicits an
increase in peak left ventricular pressure development, indicating enhanced cardiac sympathetic
stimulation (23). Clamping the base of the heart
also probably releases neuron al catecholamines by
direct stimulation of cardiac sympathetic fibers. In
the nonworking heart the elevation of cyclic AMP
and phosphorylase activity occurred later in time
after the onset of ischemia probably because
myocardial metabolic changes occurred more slowly. However, in both the working and the
nonworking heart the cyclic AMP and phosphorylase responses were completely prevented by /Jreceptor blockade. Therefore, the activation of
phosphorylase in ischemia appears to be mediated
via a catecholamine-induced increase in cyclic AMP
and a subsequent transformation of phosphorylase
kinase to its activated form.
6S00
6000
5500
5000
"
I
4500
I
4000
• o
3500
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
3000
2500
2000
ANOXIA
-4
0
4
8
12
16
20
TIME-Seconds
FIGURE S
Effect of anoxia and epinephrine on mijocardial contractility
(dP/dt) in the working rat heart in vivo. Nitrogen breathing
(diamonds) was introduced at time zero. Epinephrine was
injected intravenously (0.1 ug/kg, 0.2 ml) at time zero
(circles with dots) except during Ns respiration when it was
injected after 8 seconds of anoxia at 0.1 fig/kg (triangles)
and 1.0 fig/kg (dots). The data were obtained from oscillograph tracings reproduced from magnetic tape recordings
of the actual experiments. All data were normalized to the
mean dP/dt for all experiments at —4 seconds. Each point
represents the mean of at least five experiments. Single
asterisks denote significant differences (P<0.05) from —4
seconds. Double asterisks indicate significant differences
(P < 0.05) between anoxia in the presence and the absence
of epinephrine at the same time intervals. Bars represent
±1 SE.
less intense increase. Whether the disparity in
results is due to species or preparation differences is
not clear; our preparation was acutely adrenalectomized and ischemia was produced by a different
technique.
The rapid increase in cyclic AMP concentration
in the working heart in which ischemia was induced by placing a hemostat at the base of the
heart was probably due to two factors. Since the
heart was working, the myocardium became
Circulation Research, Vol. XXXIII, October I97i
Phosphorylase activation in anoxic hearts was not
prevented by /3-receptor blockade. If anything it
was slightly augmented. In addition, anoxia did not
produce a transformation of phosphorylase kinase
to its activated form. These findings support the
hypothesis we have previously proposed that the
mechanism of enzyme activation may be different
in anoxia compared with that in ischemia (4,
5). Since N^ breathing caused conversion of phosphorylase b to a that was independent of stimulation of adrenergic receptors and cyclic AMP
formation, it is difficult to assign a role to the cyclic
nucleotide. The apparent nonadrenergic component
of phosphorylase a formation in the anoxia studies
suggests that the covalent modification of phosphorylase is a result of an increase in the catalytic
activity of the nonactivated form of phosphorylase
kinase and that mediators other than cyclic AMP
such as Mg- + , Ca2 + , or an alkaline shift in pH may
be involved.
Free Mg2+ has been shown by Villar-Palasi and
Wei (24) to stimulate the nonactivated form of
phosphorylase kinase. They proposed that small
changes in the intracellular concentration of free
Mg2 + , for example when the ratio of Mg2+ to ATP
exceeds 1, could significantly change the activity of
the enzyme and thereby be responsible for the
in vivo activation of phosphorylase during muscle
418
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
contraction. The myocardial concentration of ATP
begins to decline within 15 seconds of N-> breathing
(4). Therefore, during anoxia it is possible that the
ratio of Mg2 + to ATP exceeds 1 and that the free
Mg2+ concentration is sufficient to increase nonactivated phosphorylase kinase activity.
Ca 2+ is required for myocardial phosphorylase
kinase activity (25), and increases in the concentration of this cation of about 1 yu.M produce a marked
elevation in activity of partially purified cardiac
phosphorylase kinase (26). We have previously
shown that catalytic activity of cardiac phosphorylase kinase is controlled by the extracellular concentration of Ca 2+ (27). Enhanced influx of this ion
has been shown by Bauer et al. (28) to occur
in smooth muscle during hypoxia. Therefore, an
increase in free Ca 2+ may be responsible for the
apparent enhanced activity of phosphorylase kinase
in the anoxic myocardium.
Hydrogen ions have a marked effect on phosphorylase kinase activity at physiological pH.
Drummond and his colleagues (25) have shown
that in cardiac muscle extracts an elevation in pH of
0.5 units in the range of 7.0 to 8.0 results in more
than a twofold increase in enzyme activity. In a
series of contractions skeletal muscle first becomes
alkaline because of hydrolysis of creatine phosphate
(29). Since anoxia causes a rapid hydrolysis of
cardiac creatine phosphate (4, 5), it is conceivable
that the myocardium becomes slightly alkaline. Dog
myocardial interstitial pH increases more than
0.05 pH units approximately 30 seconds after
changing the respiratory gas from 20% O2 to
10% O2 (30). However, coronary ischemia has an
opposite effect on intercellular pH presumably
because the washout of lactic acid and other acid
metabolites is limited (30), even with rapid
hydrolysis of creatine phosphate in the ischemic
myocardium (5, 31). Therefore, alkalosis resulting
from creatine phosphate hydrolysis could participate in regulating phosphorylase kinase activity. In
fact any one of the above mediators singly or in
combination may be responsible for enhancing the
activity of nonactivated phosphorylase kinase in
cardiac anoxia and thereby promote covalent
phosphorylase modification.
Both ischemia and anoxia caused a sustained
conversion of phosphorylase b to a for at least 2
minutes. This phenomenon confirms earlier studies
(4, 5) and is unlike the transient activation of the
cardiac enzyme that occurs with continuous epinephrine infusion (21). Inhibition of phosphorylase
DOBSON, MAYER
phosphatase, the enzyme that catalyzes the conversion of phosphorylase a to b could be involved.
Haschke and colleagues (32) have shown reversible
inhibition of phosphorylase phosphatase when
phosphorylase is activated in a concentrated proteinglycogen complex from rabbit muscle. The phosphatase was inhibited by 80% when the free Ca2+^
concentration was 0.3 mM, a concentration causing
maximal rapid activation of phosphorylase in the
complex. Therefore, Ca 2+ could participate in the
inhibition of phosphorylase phosphatase and in the
regulation of phosphorylase kinase activity in the
anoxic heart.
We have not performed studies for longer than 2
minutes to determine if phosphorylase remains
activated. However, Cornblath et al. (3) have
shown that the activity of phosphorylase b increases
after several minutes of anoxia, presumably due to
the marked elevation of AMP and inorganic
phosphate that occurs under such conditions (33,
34). This observation suggests that the activation of
glycogenolysis in the anoxic heart is governed by a
continuum of mechanisms, first by the formation of
phosphorylase a and then by either a persistence of
this form of the enzyme, an increase in phosphorylase b activity, or both.
ANOXIA AND MYOCARDIAL CONTRACTILITY
The rapid, steady decline in dP/dt observed
in the anoxic working heart at a time when cyclic
AMP concentration was increased appears to represent a dissociation between the intracellular content
of the cyclic nucleotide and the inotropic state.
These results could be explained by the supposition
that, as a consequence of anoxia, the control of contractile state by cyclic AMP is disrupted. However,
when a low dose of epinephrine was administered
during N2 breathing, an increase in dP/dt was observed. This dose of the catecholamine elicited an
increase in cyclic AMP comparable in magnitude to
that observed during anoxia. Although creatine
phosphate was almost completely hydrolyzed during
the first 20 seconds of anoxia (4, 5), the availability
of high-energy phosphate apparently was not limiting and the preparation was still capable of an increase in contractility. These results do not refute
the hypothesis that the positive inotropic effects of
catecholamines are mediated by intracellular cyclic
AMP (35) but project the possibility that the
nucleotide is not the sole mediator of changes in
cardiac contractility. It may be simplistic to
visualize only one mechanism responsible for
controlling contractility when myocardial glycogen
Circulation Research, Vol. XXXIU. October
191}
419
MECHANISMS OF PHOSPHORYLASE ACTIVATION
metabolism is regulated at several levels by a
variety of mechanisms.
Hormones and Cyclic Nucleotides, edited by J. G.
Hardman and B. W. O'Malley. New York, Academic
Press, in press.
16.
References
potentiation of the cardiac inotropic and phosphorylase response to eatecholamines as related to the
uptake of H3-catecholamines. J Pharmacol Exp Ther
150:341-348, 1965.
1. DANIORTH, W.H., NAECLE, S., AND BINC, R.J.: Effect
of ischemia and reoxygenation on glyeolytic reactions
and adenosinetriphosphate in heart muscle. Circ Res
8:965-971, 1960.
2.
KLAEWEIN, M., LAMPBECHT, W., AND LOHMANN, E.:
Der Stoffwechsel des Herzens bie experimentellam
Kammerflimmern. Z Physio! Chem 328:41-52, 1962.
3.
CORNBLATH, M., HANDLE, P.J., PARMEGCIANI, A., AND
MORGAN, H.E.: Regulation of glycogenolysis in
muscle: Effects of glucagon and anoxia on lactate
production, glycogen content, and phosphorylase
activity in the perfused isolated rat heart. J Biol
Chem 238:1592-1597, 1963.
4.
MAYEH,
S.E.,
WILLIAMS,
B.J.,
AND SMITH,
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
6. WOLLENBERCER, A., KHAUSE, E.G., AND HEIER,
17.
7. ROBISON, G.A., BUTCHER, R.W., OYE, L, MORGAN,
H.E., AND SUTHERLAND, E.W.: Effect of epinephrine
BUTCHER,
R.W.,
AND SUTHERLAND,
E.W.- Adenyl cyclase as an adrenergic receptor. Ann
NY Acad Sci 139:703-723, 1967.
9. NAMvr, D.H., AND MAYER, S.E.: Effects of epinephrine
on cardiac cyclic 3',5'-AMP, phosphorylase kinase
and phosphorylase. Mol Pharmacol 4:61-69, 1968.
10.
WALSH, D.A., PERKINS, J.P., BROSTROM, CO., Ho, E.S.,
AND KREBS, E.G.: Catalysis of the phosphorylase
lcinase activation reaction. J Biol Chem 246:19681976, 1971.
11. HAEDMAX,
J.G.,
ROBISON, G.A.,
E.W.: Cyclic nucleotides.
33:311-336, 1971.
12.
AND SUTHERLAND,
A. Role of cyclic AMP and calcium in cell
activation. CRC Crit Rev Biochem 2:95-148,
1972.
13.
SOBEL,
B.E.,
AND MAYER,
S.E.
Cyclic
14.
20.
15. MAYEH,
S.E.,
STULL,
J.T.,
WASTILA,
21. WILLIAMS, B.J., AND MAYER, S.E.: Hormonal effects of
glycogen metabolism in the rat heart in situ. Mol
Pharmacol 2:454-464, 1966.
22.
Circulation Relearch, Vol. XXXI11, October 1973
MALLJANI, A., SCHWARTZ, P.J., AND ZANCHETTI, A.:
Sympathetic reflex elicited by experimental coronary
occlusion Am J Physio! 217:703-709, 1969.
23. DEGEEST, H., LEVY, M.N., AND ZIESKE, H.:
Reflex
effects of cephalic hypoxia, hypercapnia, and ischemia upon ventricular contractility. Circ Res
17:349-358, 1965.
24. VILLAR-PALASI, C ,
AND W E I , S.H.:
Conversion
of
glycogen phosphorylase b to a bv non-active
phosphorylase b kinase: An in vitro model of the
mechanism of increase in phosphorylase a activity
with muscle contraction. Proc Natl Acad Sci USA
67:345-350, 1970.
25. DRUMMOND, G.I., DUNCAN, L., AND FRIESEN, J.D.:
Some properties of cardiac phosphorylase b kinase. J
Biol Chem 240:2778-2785, 1965.
26.
OZAWA, E., Hosoi, K., AND EBASHI, S.:
Reversible
stimulation of muscle phosphorylase b kinase by low
concentrations of calcium ions. J Biochem 61:531533, 1967.
27.
NAMM, D.H., MAYER, S.E., AND MALTBIE, M.: Role of
potassium and calcium ions in the effect of
epinephrine on cardiac cyclic adenosine 3',5'monophosphate, phosphorylase kinase, and phosphorylase. Mol Pharmacol 4:522-530, 1968.
28.
BAUER, H., GOODFORD, P.J., AND HUTER, J.: Calcium
content and 45calcium uptake of the smooth muscle
of the guinea-pig taenia coli. J Physiol (Lond)
176:163-179, 1965.
29.
DUBUISSON, M.: Les processus physique-chimiques de la
contraction musculaire. Ann Physiol Physiochem Biol
15:443-508, 1939.
W.B., AND
THOMPSON, B.: Assay of cyclic AMP by protein
kinase activation. In Methods in Enzymology:
DELANGE, R.J., KEMP, R.G., RILEY, W.D., COOPER,
R.A., AND KREBS, E.G.: Activation of skeletal muscle
phosphorylase kinase by adenosine triphosphate and
adenosine S'.S'-monophosphate. J Biol Chem
243:2200-2208, 1968.
MAYER, S.E., STULL, J.T., AND WASTILA, W.B.: Rapid
tissue fixation and extraction techniques. In Methods
in Enzymology: Hormones and Cyclic Nucleotides,
edited by J. G. Hardman and B. W. O'Malley. New
York, Academic Press, in press.
of
Chem
D.A.: Measurement of cyclic 3',5'-adenosine monophosphate by the activation of skeletal muscle protein
kinase. J Biol Chem 246:1996-2003, 1971.
adenosine
monophosphate and cardiac contractility. Circ Res
32:407^14, 1973.
Activation
J Biol
19. WASTILA, W.B., STULL, J.T., MAYER, S.E., AND WALSH,
Ann Rev Physiol
RASMUSSEN, H., GOODMAN, D.P.B., AND TENENHOUSE,
L.:
b kinase.
and properties of rabbit skeletal muscle phosphorylase b kinase. Biochemistry 8:1022-1033, 1964.
on adenosine 3',5'-phosphate levels in the isolated
perfused rat heart. Mol Pharmacol 1:168-177,
1965.
8. ROBISON, G.A.,
AND DUNCAN,
18. KHEBS, E.G., LOVE, D.S., BRATVOLD, G.E., TRAYSER,
K.A., MEYEH, W.L., AND RISCHEH, E.H.: Purification
C:
Stimulation of 3',5'-cyclic AMP formation in dog
myocardium following anest of blood flow. Biochem
Biophys Res Comm 36:664-670, 1969.
DRUMMOND, G.I.,
cardiac phosphorylase
241:5893-5898, 1986.
J.M.:
Adrenergic mechanisms in cardiac glycogen metabolism. Ann NY Acad Sci 139:686-702, 1967.
5. MAYER, S.E.; Effect of epinephrine on carbohydrate
metabolism in the heart. In Factors Influencing
Myocardial Contractility, edited by R. D. Tanz, F.
Kavaler, and J. Roberts. New York, Academic Press,
1967, pp 443-455.
HARDMAN, J.G., MAYER, S.E., AND CLARK, B.: Cocaine
30.
GEBERT, G., BENZLVG, H., AND STROHM, M.: Changes in
the interstitial pH of dog myocardium in response to
420
DOBSON, MAYER
local ischemia, hypoxia, hyper- and hypocapnia,
measured continuously by means of glass microelectrodes. Pfluegers Arch 329:72-81, 1971.
31.
IMAI, S., RILEV, A.L., AND BEHN-E, R.M.: Effect of
ischemia on adenine nucleotides in cardiac and
skeletal muscle. Circ Res 15:443-450, 1964.
32.
HASCHKE, R., HEILMEYEH, L.M.G., JR., MEYEB, F., AND
FISCHER, H.: Control of phosphorylase activity in a
muscle glycogen particle: III. Regulation of phosphorylase phosphatase. ] Biol Chem 245:6657-6663,
1970.
33. MORGAN, H.E., AND PARMEGCIA.NI, A.: Regulation of
glycogenolysis in muscle: II. Control of glycogen
phosphorylase reaction in isolated perfused heart. J
Biol Chem 239:2435-2439, 1964.
34. NEELY, J.R., ROVETTO, M.J., AND ORAM, J.F.:
Myocardial utilization of carbohydrates and lipids.
Prog Cardiovasc Dis 15:289-329, 1972.
35. SUTHERLAND, E.W., AND RALL, T.W.: Relation of
adenosine 3',5'-phosphate and phosphorylase to the
action of catecholamines and other hormones.
Pharmacol Rev 12:265-299, 1960.
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
Circulation Research, Vol. XXXIII, October 197}
Mechanisms of Activation of Cardiac Glycogen Phosphorylase in Ischemia and Anoxia
JAMES G. DOBSON, Jr. and STEVEN E. MAYER
Downloaded from http://circres.ahajournals.org/ by guest on June 18, 2017
Circ Res. 1973;33:412-420
doi: 10.1161/01.RES.33.4.412
Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1973 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7330. Online ISSN: 1524-4571
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circres.ahajournals.org/content/33/4/412
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further information
about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation Research is online at:
http://circres.ahajournals.org//subscriptions/