* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Consider sepsis in the young child with fever without
Survey
Document related concepts
Transcript
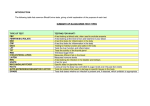
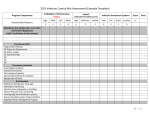
Serum procalcitonin (PCT) and Creactive protein (CRP) levels as markers of bacterial infection in hospitalized patients. EBM Guidelines Last updated: 2009-03-18 © Duodecim Medical Publications Ltd The diagnostic accuracy of PCT might possibly be higher than that of CRP to differentiate bacterial infections from viral infections and other non-infective causes of systemic inflammation in hospitalized patients. A meta-analysis 1 included 12 studies with a total of 1 386 subjects. The accuracy of determination of PCT and CRP levels for the diagnosis of bacterial infection was evaluated. The 12 enrolled studies included a total of 46 neonates, 638 children, and 702 adults in different areas of the hospital. Approximately one-half of the subjects were in intensive care units. The diagnostic criteria and the type of infections varied markedly among the studies. In the statistical analysis, PCT level was found to be more sensitive 88% (95% CI 80% to 93%) vs. 75% (95% CI 62% to 84%) and more specific 81% (95% CI to 67% to 90%) vs. 67% (95% CI 56% to 77%) than CRP level for differentiating bacterial from non-infective causes of inflammation. The Q value (obtained from SROC curves) for PCT markers was higher (0.82 vs. 0.73). The sensitivity for differentiating bacterial from viral infections was also higher for PCT markers 92% (95% CI 86% to 95%) vs. 86% (95% CI 65% to 95%); the specificities were comparable 73% (95% CI 42% to 91%) vs. 70% (95% CI 19% to 96%). The Q value was higher for PCT markers (0.89 vs. 0.83). PCT markers also had a higher positive likelihood ratio and lower negative likelihood ratio than did CRP markers in both groups. Comment: The quality of evidence is downgraded by review quality, poor reporting, inconsistency and indirectness (differences in studied patients and diagnostic criteria). References 1. Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis 2004 Jul 15;39(2):206-17. CRP and procalcitonin best for dx in febrile children Daily POEMs Published: 2011-08-01 © 2011 John Wiley & Sons, Inc. Clinical question What is the diagnostic value of laboratory tests for the diagnosis of serious infections in febrile children? Bottom line C-reactive protein and procalcitonin are the most effective laboratory tests for ruling in or ruling out serious infections in febrile children. Both tests are better at ruling out than ruling in disease. A white blood cell count is not useful, and other markers of inflammation do not provide good sensitivity or specificity. (LOE = 2a) Reference Van den Bruel A, Thompson MJ, Haj-Hassan T, et al. Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ 2011;342:d3082. Study design: Meta-analysis (other) Funding source: Government Setting: Outpatient (any) Synopsis To conduct this systematic review, the authors searched 4 databases, including DARE, to find studies that evaluated the diagnostic accuracy of tests in febrile outpatient children at least 30 days of age. They identified 14 studies, all of moderate quality or low quality. The prevalence of serious infection ranged from 4.5% to 29.3%. The tests best at ruling in serious infection were C-reactive protein, using a cut-off of 80 mg/L (positive likelihood ratio [LR+] = 8.4; 95% CI, 5.1 - 14.1), and procalcitonin greater than 2 ng/mL (LR+ [from 2 studies] = 3.6 and 13.7; 95% CIs, 7.4 - 25.3 and 1.4 - 8.9). Using a C-reactive protein cutoff of 20 mg/L (negative likelihood ratio [LR-] = 19 - .25) and a procalcitonin cutoff of .5 ng/mL (LR- = .08 - .25) is effective in ruling out serious infection. An elevated white blood cell count is not effective at ruling in or ruling out disease. Combinations of tests did not appreciably improve diagnostic accuracy. Allen F. Shaughnessy, PharmD, MMedEd Professor of Family Medicine Tufts University Boston, MA Copyright © 2011 John Wiley & Sons, Inc. CRP point-of-care testing in maxillary sinusitis EBM Guidelines Last updated: 2012-09-05 © Duodecim Medical Publications Ltd Level of evidence = B In general practice, CRP point-of-care testing compared with non-testing is effective in decreasing antibiotic prescriptions for lower respiratory tract infection (LRTI) and acute maxillary sinusitis. The quality of evidence is downgraded by imprecise results (wide confidence intervals). Summary A Dutch family practice study 1 included 32 physicians and 258 patients (107 with LRTI and 151 with rhinosinusitis). Patients were individually randomized to CRP assistance or routine care (control). Primary outcome was antibiotic use after the index consultation. Secondary outcomes included antibiotic use during the 28-day follow-up, patient satisfaction, and clinical recovery. Patients in the CRP-assisted group used fewer antibiotics (43.4%) than control patients (56.6%) after the index consultation (relative risk [RR] = 0.77; 95% confidence interval [CI], 0.56-0.98). This difference remained significant during follow-up (52.7% vs 65.1%; RR = 0.81; 95% CI, 0.62-0.99). Delayed prescriptions in the CRP-assisted group were filled only in a minority of cases (23% vs 72% in control group, P < .001). Recovery was similar across groups. Satisfaction with care was higher in patients managed with CRP assistance (P = .03). In an observational study by Danish GP:s 2, a group of GPs registered all contacts (n = 17 792) with patients who had respiratory tract infections during a 3-week period. GPs who used a CRP rapid test were compared with GPs who did not, and the treatment of their patients (n = 1444) with suspected sinusitis was compared. A CRP rapid test was used by 77% (n = 281) of the GPs. In the group of GPs using a CRP rapid test, the rate of antibiotic prescribing was 59% (95% confidence interval [CI] = 56 to 62) compared with 78% (95% CI = 73 to 82) in the group of GPs who did not use a CRP test. Performing a CRP rapid test was the factor that exerted the greatest influence on whether the patients were prescribed antibiotics, and the level of CRP had a strong influence on the prescribing rate. Date of latest search: 2012-05-14 References 1. Cals JW, Schot MJ, de Jong SA et al. Point-of-care C-reactive protein testing and antibiotic prescribing for respiratory tract infections: a randomized controlled trial. Ann Fam Med 2010;8(2):124-33. 2. Bjerrum L, Gahrn-Hansen B, Munck AP. C-reactive protein measurement in general practice may lead to lower antibiotic prescribing for sinusitis. Br J Gen Pract 2004;54(506):659-62. Sepsis (child) Essential Evidence Last Updated on 2012-08-23 © 2012 John Wiley & Sons, Inc. Interactive Tools Authors: Julie Story Byerley, MD, MPH, Assistant Professor, General Pediatrics and Adolescent Medicine, University of North Carolina at Chapel Hill Editors: Su-Ting T. Li, MD, MPH, Associate Professor of Pediatrics, Pediatric Residency Program Director and VIce Chair of Education, University of California, Davis Linda French, MD, Professor and Chair, Department of Family Medicine, University of Toledo Overall Bottom Line Fever in an infant younger than 60 days requires evaluation including complete blood count, blood culture, catheterized urinalysis, and urine culture. Lumbar puncture for CSF culture is necessary for infants younger than 30 days but can be delayed in infants older than 30 days who meet strict low-risk criteria. A Neonatal herpes infection should also be considered in infants younger than 30 days and should be treated with IV acyclovir, if necessary. A Infants younger than 2 months with fever without source being evaluated for sepsis should receive empiric ampicillin and either gentamicin or a third-generation cephalosporin. A Consider urinary tract infection (UTI) in children aged 2 months to 36 months with fever without source. If they are well appearing and no UTI is present, do not use empiric antibiotics. B Background Consider sepsis in the young child with fever without source. This chapter will address the evaluation of the outpatient with fever without source in the 0 to 36-month age range. The newborn still in the nursery immediately after delivery is not considered here. Fever is defined as rectal temperature greater than or equal to 38°C. 27Serious bacterial infection is defined as growth of a known pathogen in cultures of blood, spinal fluid, urine, or stool; new infiltrate on chest x-ray; or obvious bacterial focal infection. 25 Prevalence In infants younger than 3 months of age presenting to primary care clinics with fever ≥ 38°C, UTI was present in 5.4%, bacteremia in 1.8%, and bacterial meningitis in 0.5%. This varied by age: 4.1% of febrile infants in the first month of life had bacteremia or meningitis, compared with 1.9% in the second month and 0.7% in the third month. Not all patients with positive CSF cultures had positive blood cultures. 24 Neonatal herpes simplex virus (HSV) infection occurs in approximately 30 of 100,000 live births; 95%-98% present before 22 days of life and only 7%-14% present as fever without source. 27 Of children aged 1 month to 36 months presenting with fever > 38°C and having blood culture in a community hospital emergency department, 3.5% of blood cultures were positive and more than 80% of those positive results were considered contaminants. 23 The prevalence of occult bacteremia in febrile children aged 3 months to 36 months is approximately 1.5%-2%. 22 Serious bacterial infection is present in approximately 10% of infants aged 2 months to 6 months presenting with fever greater than 39°C. 21 Causes of the Condition | Pathogens causing bacteremia in children aged 0 to 36 months include Escherichia coli, Group B Streptococcus (GBS), Enterococcus faecalis, Staphylococcus aureus, Streptococcus pneumoniae, and other gram negative organisms. 21 Listeria is also possible in neonates younger than 2 months old. Pathophysiology | Serious bacterial infections in infants include UTI,meningitis, bacteremia, pneumonia,gastroenteritis, and other focal infections. For information on pathophysiology, see the chapters dealing with those specific infections. Sepsis (child) Essential Evidence Last Updated on 2012-08-23 © 2012 John Wiley & Sons, Inc. Authors: Julie Story Byerley, MD, MPH, Assistant Professor, General Pediatrics and Adolescent Medicine, University of North Carolina at Chapel Hill Editors: Su-Ting T. Li, MD, MPH, Associate Professor of Pediatrics, Pediatric Residency Program Director and VIce Chair of Education, University of California, Davis Linda French, MD, Professor and Chair, Department of Family Medicine, University of Toledo Overall Bottom Line Fever in an infant younger than 60 days requires evaluation including complete blood count, blood culture, catheterized urinalysis, and urine culture. Lumbar puncture for CSF culture is necessary for infants younger than 30 days but can be delayed in infants older than 30 days who meet strict low-risk criteria. A Neonatal herpes infection should also be considered in infants younger than 30 days and should be treated with IV acyclovir, if necessary. A Infants younger than 2 months with fever without source being evaluated for sepsis should receive empiric ampicillin and either gentamicin or a third-generation cephalosporin. A Consider urinary tract infection (UTI) in children aged 2 months to 36 months with fever without source. If they are well appearing and no UTI is present, do not use empiric antibiotics. B Diagnosis Fever in an infant younger than 30 days requires evaluation including complete blood count, blood culture, catheterized urinalysis, urine culture, and lumbar puncture for CSF culture. A 27 Criteria to determine low risk of sepsis in neonates are unreliable. B 9 Neonatal herpes infection should also be considered in infants younger than 30 days. C 27 Fever in infants aged 30 days to 60 days requires the same evaluation as those younger than 30 days, except that lumbar puncture can be delayed or omitted if the infant meets low-risk criteria, there is reliable follow-up in 12 hours to 24 hours, no antibiotics will be administered, and family and physician are in agreement. C 27 All children younger than 1 year with fever without source A and girls aged 1 year to 2 years B should be considered at risk of UTI. 27 Routine CBC and blood culture of well-appearing children aged 2 months to 36 months with fever but without a source is not recommended. C Differential Diagnosis | Diagnosis Features Urinary tract infection positive urine culture Meningitis positive CSF culture Bacteremia positive blood culture Herpes simplex virus infection localization of herpes simplex virus from culture or polymerase chain reaction of CSF, surface swab, or blood Pneumonia infiltrate on chest x-ray Bacterial enteritis diarrhea should be present, positive stool culture Viruses Other causes of fever Using the History and Physical | Rule out sepsis when an infant has a fever without source after history and physical examination. In acutely ill children in the primary care setting, MD opinion that "something is wrong", parent opinion that "illness is different from previous", cyanosis, impaired peripheral circulation, meningeal irritation, petechiae, and convulsions greatly increase the likelihood of serious bacterial infection. Other individual symptoms with relatively high positive predictive value for serious bacterial infection include unconsciousness, drowsiness, moaning, change in crying, decreased breathing sounds, tachypnea, and inconsolability. Obtain rectal temperatures in infants who may have sepsis. 27 Ear thermometers are unreliable 18 17 and axillary temperatures demonstrate wide variability. 16 However, subjective fever assessment by a parent is usually accurate. 27 The magnitude of fever does not reliably predict illness severity, 27 and response to antipyretics does not change the likelihood of serious bacterial infection. 28 The presence of febrile seizure likely does not significantly increase the risk of bacteremia in febrile children aged 2 months to 24 months. 15 Obtain an immunization history, especially regarding pneumococcal vaccination. Infants younger than 28 days with fever should be presumed to have a serious bacterial infection. 28 On physical examination note the Yale Observation Criteria, specifically lethargy, poor or absent eye contact, failure of child to interact with parents or environment, poor perfusion, acrocyanosis, mottling, delayed capillary refill, and respiratory rate changes. 27 Well-appearing infants and young children should smile, be alert and consolable, and without signs of dehydration. Perfusion should be good and there should be no sign of respiratory distress. Tachypnea is a sign of pneumonia and, when present, should prompt chest x-ray. 28 Selecting Diagnostic Tests | See Figure 1 and Table 1 for algorithms for evaluation of fever in an infant younger than 2 months. 27 25 Consider HSV infection in infants aged 0 to 30 days if risk factors are present or if the patient is not improving with antibiotic therapy. Often neonatal HSV infection will present with seizure, disseminated disease, or rash, although it can present with fever alone. To test for neonatal HSV order the following: blood viral culture, CSF viral culture, CSF polymerase chain reaction for HSV, conjunctiva viral culture, skin lesion viral culture, nasopharyngeal viral culture, rectal viral culture, and also consider liver function testing. Infants aged 31 days to 60 days are unlikely to have HSV. Testing in this case should be reserved for infants with suggestive clinical findings or prior HSV infection. 27 In infants >2 months who are not so ill as to require immediate antibiotics, risk of UTI 3 should be assessed. 28 Infants with a low risk of UTI with good follow-up may not require urine studies. 28 In infants not in the low-risk group, send a catheterized urine for urinalysis and culture OR obtain a urinalysis first, and obtain a catheterized urine for culture if urinalysis suggests a UTI (positive leukocyte esterase, nitrite or leukocytes/bacteria on microscopic). For girls, the probability of UTI increases to >1% with more than 1 of the following risk factors: age <12 months, absence of another source of infection, temperature >=39C, fever >=2 days, or white race. Uncircumcised boys are not low-risk. 3 For circumcised boys, the probability of UTI increases to >1% with more than 2 of the following risk factors: absence of another source of infection, temperature >=39C, fever >24 hours, or non-black race. Diagnosis of UTI requires both urinalysis that suggest UTI (pyuria +/- bacteriuria) and >50,000 cfu/ml of a uropathogen on a catheterized urine sample. 6 31 Obtain a chest x-ray in young children with fever without source and respiratory symptoms. 28 27 A chest x-ray may be useful in children younger than 5 years with an elevated WBC count (> 20,000) and a fever higher than 39°C without source. 14 Other viral testing should be pursued if clinically appropriate. Viral testing could decrease hospitalization rates, specifically from influenza and enterovirus. Positive viral antibody testing does not eliminate the possibility of serious bacterial infection. 21 Patients with serious bacterial infection have higher average WBC count (>15,000), 29 absolute neutrophil count, CRP levels, 28 29 procalcitonin levels, 29 and Yale Observation Scores than those without serious bacterial infections. 21 Patients with CRP>80 mg/dl (LR+ 8.4; 95% CI: 5.1-14.1) or procalcitonin>2 ng/ml (LR+: 3.6-13.7; 95% CI: 1.4-25.3) are more likely to have a serious bacterial infection. Patients with CRP<20 mg/dl or procalcitonin <0.5 ng/ml are less likely to have a serious bacterial infection. 29 The utility of newer diagnostic tests such as cytokine and fibronectin levels have been explored but are not useful at this point. 13 For children aged 2 months to 36 months with fever of unknown source who are well appearing, routine CBC and blood culture are not recommended. Children aged 2 months to 36 months with fever who are not well appearing should have CBC and blood culture obtained. In children aged 3 months to 36 months a CRP test may not add diagnostic information beyond the WBC count and absolute neutrophil count, 12 though there is conflicting information in the literature. 11 Combinations of normal WBC, absolute neutrophil count, and procalcitonin results have a very good negative predictive value for ruling out bacteremia in infants aged 3 months to 36 months with fever and no obvious source. CRP and IL-6 are only moderately accurate, although normal IL-6 and normal CRP results have good negative predictive value (LR- = 0.07). Clinical Decision Rules | The Rochester criteria helps to identify neonates with fever who do not need antibiotics or hospital admission. Another set of criteria is based on a study of approximately 10,000 children aged 3 months to 36 months who presented to an emergency department with fever and had a CBC and blood culture. It uses the patient's temperature, sex, and absolute neutrophil count. The rule is 87% sensitive. Approach to the Patient | See algorithms in Figure 1 and Figure 2 for a suggested approach to the evaluation of fever without a clear source. History and Physical Tests | Fever (>= 38 C) and age <= 3 months -> bacteremia or meningitis Pretest Probability (%): 2.0 Probability of disease when test outcome is: Test Name Positive (LR+) Negative (LR-) Moderately or very ill appearance 3.5% (1.8) 1.2% (0.6) Moderately or very ill appearance OR abnl WBC 3.5% (1.8) 0.6% (0.3) moderately or very ill appearance OR abnl WBC OR abnl urinalysis 3.5% (1.8) 0.5% (0.3) Acute illness in child(primary care) -> serious bacterial infection Pretest Probability (%): 1.0 Probability of disease when test outcome is: Test Name Positive (LR+) Negative (LR-) Cyanosis 34.0% (51) 0.9% (0.9) Impaired peripheral circulation 27.7% (38) 0.9% (0.9) Meningeal irritation 20.8% (26) 1.0% (1.0) MD opinion: 'something is wrong' 18.9% (23) 0.4% (0.4) Convulsions 17.5% (21) 0.9% (0.9) Unconsciousness 16.8% (20) 0.9% (0.9) Parent: 'illness different from previous' 12.4% (14) 0.6% (0.6) Petechiae 10.8% (12) 1.0% (1.0) Changed crying 10.0% (11) 0.7% (0.7) Tachypnea 9.0% (9.8) 0.7% (0.7) Decreased breath sounds, dullness 8.6% (9.3) 0.8% (0.8) Dyspnea 8.6% (9.3) 0.6% (0.6) Drowsy 6.3% (6.6) 0.7% (0.7) Crepitations 5.7% (6.0) 0.7% (0.7) Temp >= 40 C 5.6% (5.9) 0.8% (0.8) Urinary symptoms 5.6% (5.9) 0.9% (0.9) Moaning 5.6% (5.9) 0.9% (0.9) Inconsolable 5.3% (5.5) 0.8% (0.8) Changed breathing 4.3% (4.4) 0.7% (0.7) Does not laugh any more 4.1% (4.2) 0.6% (0.6) Weight loss 2.5% (2.5) 1.0% (1.0) Dehydration 2.5% (2.5) 1.0% (1.0) Irritable 2.3% (2.3) 0.9% (0.9) Temp >= 39 C 2.3% (2.3) 0.6% (0.6) Smonolent 2.2% (2.2) 0.8% (0.8) Rash 1.9% (1.9) 1.0% (1.0) Decr eating and drinking 1.5% (1.5) 0.8% (0.8) Temp >= 38 C 1.5% (1.5) 0.4% (0.4) Coughing 1.3% (1.3) 0.7% (0.7) Vomiting 1.1% (1.1) 1.0% (1.0) Diarrhea 1.0% (1.0) 1.0% (1.0) Upper resp infection 1.0% (1.0) 1.0% (1.0) Illness >= 48 hours 0.9% (0.9) 1.1% (1.1) Tummy ache 0.4% (0.4) 1.1% (1.2) Headache 0.2% (0.2) 1.2% (1.2) Diagnostic Tests | Fever (>= 39 C) and no obvious source(3-36 months) -> bacteremia Pretest Probability (%): 7.0 Probability of disease when test outcome is: Test Name Procalcitonin >= 2 ng/ml Positive (LR+) 23.6% (4.1) Negative (LR-) 3.6% (0.5) WBC >= 15 and ANC >= 10 and/or procalcitonin >= 2 15.8% (2.5) ng/ml 0.1% (0.01) WBC >= 15,000 and ANC >= 10,000 13.6% (2.1) 3.2% (0.4) Procalcitonin >= 2 ng/ml and/or CRP >= 40 mg/L and/or WBC >= 15 and ANC >= 10 13.1% (2.0) 0.1% (0.01) WBC >= 15 and ANC >= 10 and/or CRP >= 40 mg/L 11.9% (1.8) 2.0% (0.3) Procalcitonin >= 2 ng/ml and/or CRP >= 40 mg/L 11.9% (1.8) 3.5% (0.5) C reactive protein >= 40 mg/L 8.3% (1.2) 6.2% (0.9) Sepsis suspected(< 1 yr) -> sepsis Pretest Probability (%): 20.0 Probability of disease when test outcome is: Positive (LR+) Test Name Negative (LR-) CRP>= 20 mg/L 61.2% (6.3) 14.2% (0.7) CRP >= 10 mg/L 58.8% (5.7) 9.5% (0.4) IL-6 >= 400 pg/ml OR CRP >= 20 mg/L 57.9% (5.5) 9.9% (0.4) CRP >= 5 mg/L 57.0% (5.3) 5.9% (0.3) IL-6 >= 400 pg/ml 55.6% (5.0) 14.9% (0.7) IL-6 >= 400 pg/ml OR CRP >= 20 mg/L 55.1% (4.9) 6.1% (0.3) IL-6 >= 20 pg/ml OR CRP >= 10 mg/L 36.5% (2.3) 1.7% (0.07) IL-6 >= 20 pg/ml 35.5% (2.2) 7.8% (0.3) IL-6 >= 20 pg/ml OR CRP >= 10 mg/L 34.4% (2.1) 6.5% (0.3) UTI suspected(child) -> UTI Pretest Probability (%): 30.0 Probability of disease when test outcome is: Test Name Positive (LR+) Negative (LR-) Pyuria and bacteriuria 94.1% (37) 8.3% (0.2) Nitrite AND LE positive 92.4% (28) 13.7% (0.4) Gram stain, any organisms 88.9% (19) 2.9% (0.07) Nitrite positive 87.2% (16) 17.9% (0.5) Bacteriuria 86.3% (15) 7.5% (0.2) Unspun urine >= 10 WBC/mm3 75.0% (7.0) 10.0% (0.3) Nitrite OR LE positive 72.3% (6.1) 7.9% (0.2) Pyuria 71.7% (5.9) 10.4% (0.3) LE positive 70.2% (5.5) 10.0% (0.3) Pyuria or bacteriuria 64.3% (4.2) 4.5% (0.1) Spun urine >= 5 WBC/hpf 57.8% (3.2) 15.3% (0.4) Uriscreen 57.8% (3.2) 0.4% (0.01) UTI suspected(adult) -> UTI Pretest Probability (%): 60.0 Probability of disease when test outcome is: Test Name Positive (LR+) Negative (LR-) Nitrite AND LE positive 98.5% (45) 40.3% (0.5) Nitrite positive 80.8% (2.8) 47.8% (0.6) Nitrite OR LE positive 78.9% (2.5) 35.1% (0.4) Leukocyte esterase positive 78.3% (2.4) 42.4% (0.5) > 15 WBC/HPF 76.7% (2.2) 28.1% (0.3) > 5 RBC/HPF 75.0% (2.0) 46.5% (0.6) > few bacteria 64.3% (1.2) Herpangina Essential Evidence Last Updated on 2012-10-20 © 2012 John Wiley & Sons, Inc Authors: Laura E. Hufford, MD, Assistant Clinical Professor, University of California at Davis Editors: David Slawson, MD, Vice Chair, Department of Family Medicine, University of Virginia Mark H. Ebell, MD, Associate Professor, University of Georgia Kenny Lin, Associate Editor Overall Bottom Line Patients typically present with 1- to 4-mm papulovesicular lesions with an erythematous base in the oropharynx. C Symptomatic treatment with oral and topical analgesic medications is recommended. C Fever usually resolves within 4 days of illness and oral lesions within 1 week. C Background Acute illness presenting with 2- to 4-mm papulovesicular oral lesions with an erythematous base often accompanied by fever and myalgias at the onset of illness. Incidence Largely unknown; appears to be somewhat more common in boys than in girls and usually affects children. Approximately 1 to 20 mild cases of enterovirus 71 infection per physician per week during epidemics in Taiwan between 1998 and 2005. 4 In the same study, 0.5 to 9.5 severe cases found per 100,000 population younger than 15 years. Causes of the Condition | The most common cause is group A coxsackievirus. Additional causes include group B coxsackievirus, echovirus, and other enteroviruses. 5 In a Japanese surveillance study (2004-2008), 7 enterovirus serotypes were highly associated with herpangina and hand-foot-and-mouth disease. 8 Pathophysiology | Enteroviral infections are spread by fecal-oral and respiratory routes. Outbreaks typically occur in summer and early fall in temperate climates. 6 Diagnosis Bottom Line Patients typically present with 1- to 4-mm papulovesicular lesions with an erythematous base in the oropharynx. C 4 No laboratory screening is indicated for typical cases. C Differential Diagnosis | Diagnosis Hand-foot-and-mouth disease Features Oral lesions usually involve the buccal mucosa and tongue; vesiculopapular lesions are seen on hands and feet Lesions spare the dorsum of the tongue and hard palate; fever is absent The posterior pharynx is erythematous, with tonsillar exudate and cervical adenopathy Lesions are white plaques or shallow ulcers with erythematous base; cervical adenopathy is often present Using the History and Physical | Initial symptoms include fever and malaise. Older children may complain of backache or myalgias. Papulovesicular lesions of 1 to 4 mm with an erythematous base develop within the oropharynx and are commonly present on the tonsillar pillars, uvula, or soft palate. The oral lesions are associated with pain on swallowing and sore throat. In general, this is a self-limited disease with fever resolving after 4 days and oral lesions after 1 week. Lesions on the hands, feet, and buttocks suggest hand-foot-and-mouth disease. Examine the patient for adenopathy suggestive of herpes infection or pharyngitis of viral or bacterial etiologies. Selecting Diagnostic Tests | Diagnosis is made clinically based on the history and physical examination. Identification of the viral etiology is indicated only in prolonged or complicated cases. Many enteroviruses can be isolated in viral culture; however, group A coxsackieviruses are difficult to isolate by this method, and thus polymerase chain reaction (PCR) detection is preferred. 3 A high-throughput neutralization enzyme immunoassay for detecting growth of enterovirus 71 in rhabdomyosarcoma cells has recently been developed and appears to have high sensitivity (100%) and specificity (94.9%) for this virus. 9 Clinical Decision Rules | No relevant clinical decision rules are found. Approach to the Patient | Suspect herpangina in patients who present with 1- to 4-mm papulovesicular lesions with an erythematous base in the oropharynx. The diagnosis is primarily clinical; PCR testing for group A coxsackievirus may be considered to confirm the diagnosis in patients with a prolonged or complicated course. Prevent transmission by practicing proper hand hygiene, particularly when Treatment Give symptomatic treatment with oral and topical analgesic medications. C Consider hospitalization in extreme cases of dehydration or for supportive care of rare neurologic manifestations. C Drug Therapy | Give symptomatic treatment with oral medications such as acetaminophen and topical analgesic medications such as diphenhydramine, liquid antacids, and Xylocaine solutions. Maintain adequate hydration orally or parenterally if needed. For serious, life-threatening enteroviral infections, IV immune globulin with high antibody titers for enterovirus may provide benefit. 6 Pleconaril, an enteroviral replication inhibitor, has been demonstrated to have modest effectiveness in reducing days of illness in patients with severe enteroviral meningitis. 2 When to Refer or Hospitalize | Hospitalization is indicated for dehydration from lack of oral intake or for management of rare neurologic manifestations. Epidemics of herpangina and hand-foot-and-mouth disease caused by enterovirus 71 have been associated with aseptic meningitis, meningoencephalitis, and flaccid paralysis, 1 the occurrence of fever, stiff neck and headache is also more common in patients with this virus. 10 Pulmonary edema is a rare complication of enterovirus 71 infection. A single historically controlled clinical trial with 24 children found reduced mortality with milrinone treatment (36% vs. 92%, P =.005). 7 Histoplasmosis Essential Evidence Last Updated on 2012-10-20 © 2012 John Wiley & Sons, Inc. Authors: Jeffrey E. Jarrett, MD, Pulmonary and Critical Care Fellow, Creighton University Medical Center Lee E. Morrow, MD, MS, Associate Professor of Medicine Director, Creighton University Medical Center Editors: Gary Ferenchick, MD, Chief, Division of General Medicine, Michigan State University Linda French, MD, Professor and Chair, Department of Family Medicine, University of Toledo Erik Lindbloom, Associate Editor Overall Bottom Line Infection with histoplasmosis is exceedingly rare outside of endemic areas. C Typical symptoms are nonspecific and include fever, productive cough, malaise. C Diagnosis can be accomplished by the use of urinary antigen testing, serology, histopathology and/or culture (Table 1). C Treatment is indicated in moderate to severe acute pulmonary histoplasmosis, chronic pulmonary histoplasmosis, disseminated histoplasmosis, CNS histoplasmosis, and severe cases of mediastinitis (Table 2). A Background Infection with dimorphic yeast of Histoplasmosis capsulatum can cause a variable clinical course from asymptomatic self limited infection to progressive infection which may be life threatening. Incidence Eighty percent of people living in endemic areas are skin test positive. 7 Causes of the Condition | Infection with dimorphic yeast of histoplasmosis capsulatum. Ohio and Mississippi river valleys are considered endemic areas in United States. Patients taking TNF-alpha inhibitors should be monitored closely for reactivation of histoplasmosis. The FDA required safety labeling changes to these agents as 240 cases had been reported up to September 2008 with 45 deaths due to histoplasmosis. 9 Pathophysiology | Inhalation of spores from disrupted soil, then spread hematogenously to the reticuloendothelial tissues in the first few weeks. Development of cellular mediated immunity results in spontaneous resolution in 99% of infections. Patients with poor cell-mediated immunity are at high risk for progressive infection. A high volume of inhaled spores may also cause progressive infection. Risk Factors | Risk Factor Residence in endemic area Exposure to disrupted soil in endemic area Cell-mediated immunity deficiency TNF-alpha inhibitor therapy Diagnosis Bottom Line Typical symptoms are nonspecific and include fever, productive cough, malaise. C Diagnosis requires a high index of suspicion based upon risks for deficits in cellmediated immunity (e.g. AIDS, TNF-alpha blockers) and travel to or residing in endemic areas. C Diagnosis can be accomplished by the use of urinary antigen testing, serology, histopathology and/or culture (Table 1). B 6 Differential Diagnosis | Diagnosis Features Atypical pneumonias Lack of significant mediastinal lymphadenopathy Tuberculosis Positive AFB stains Malignancy Positive cytology, pathology for malignant cells Sarcoidosis Lack of fungal elements on biopsy Using the History and Physical | Most important factor is to obtain a travel, work, and social history due to geographic preference of Histoplasmosis. Spectrum of illness ranges from asymptomatic to severe pneumonia with respiratory failure, depending on the intensity of exposure, and the immunity of the host. 1 Nonspecific symptoms of cough, fever, sputum production, weight loss, and occasional chest discomfort. Of symptomatic infections, 60% are acute pulmonary, 10% each are chronic pulmonary, pericarditis, rheumatologic, or disseminated, and less than 1% are fibrosing mediastinitis. 3 Selecting Diagnostic Tests | Diagnostic testing depends on clinical syndrome of infection. Gold standard is culture of H. capsulatum in sputum, bronchoalveolar lavage fluid, blood, or tissue specimens. However, cultures may take up to 6 weeks to show growth. Serologic testing includes both complement fixation (CF) and immunodiffusion (ID). CF is more sensitive but less specific than ID. Serologic tests are not useful in immunocompromised patients who cannot mount a response to infection. Consider bronchoscopy for moderate to severe cases with radiographic changes for histopathologic diagnosis. The best use of the urinary antigen is in AIDS patients with disseminated histoplasmosis. 4 Skin testing reagents are no longer available in the United States. Evidence of bone marrow suppression (pancytopenia) and hepatocellular enzyme elevations may be found in disseminated histoplasmosis. See Table 1 for an overview of diagnostic testing. Approach to the Patient | The vast majority of patients have asymptomatic self limited infections; only 1% of infected patients will have a clinically significant manifestation. 4 G1 Diagnosis requires a high index of suspicion based upon risks for deficits in cellmediated immunity (e.g. AIDS, TNF-alpha blockers) and travel to or residing in endemic areas. Patients with cell-mediated immunity are at a higher risk for pro Treatment Bottom Line Treatment is indicated in moderate to severe acute pulmonary histoplasmosis, chronic cavitary pulmonary histoplasmosis, disseminated histoplasmosis, and CNS histoplasmosis (Table 2). A 1 The efficacy of treatment for mediastinal granuloma or lymphadenitis and mild acute focal pulmonary infection is unknown (Table 2). C 1 G1 Drug Therapy | Mild cases are usually self limited and do not require therapy. Treatment is indicated in moderate to severe acute pulmonary histoplasmosis, chronic cavitary pulmonary histoplasmosis, disseminated histoplasmosis, CNS histoplasmosis. The efficacy of treatment for mediastinal granuloma or lymphadenitis and mild acute focal pulmonary infection is unknown. 1 See Table 2 for specific treatment recommendations. Itraconazole levels should be monitored; it is a strong CYP3A4 enzyme inhibitor. The oral suspension of itraconazole has a higher bioavailability than the capsules. 5 Surgical Therapy | In cases of fibrosing mediastinitis, surgery should be avoided. Rare case reports of stenting of great vessels and/or airways with fibrosing mediastinitis have been published, but this is generally not indicated. When to Refer or Hospitalize Patients with signs of SIRS or respiratory distress should be hospitalized. Nocardiosis Essential Evidence Last Updated on 2012-08-18 © 2012 John Wiley & Sons, Inc. Authors: Kristi M. Moore, MD, Clinical Instructor, University of Maryland Majid E. Cina, MD, Assistant Professor of Medicine , University of Maryland Editors: Henry C. Barry, MD, MS, Associate Professor, Michigan State University Mark H. Ebell, MD, Associate Professor, University of Georgia Erik Lindbloom, Associate Editor Overall Bottom Line Suspect nocardiosis when a patient presents with a brain, soft tissue, or cutaneous abscess and a recent or current radiographic pneumonia, particularly if immunocompromised. C Perform Gram stain, acid-fast staining, culture, and antimicrobial susceptibility testing on clinical samples for all patients with suspected nocardiosis. 16s rRNA PCR may be used to identify nocardia species even after antibiotic therapy has been initiated. C Appropriate imaging includes CXR or chest CT scan for suspected pulmonary nocardiosis, brain CT or MRI with contrast for suspected CNS disease, and helical CT scan to delineate mycetoma. C Immunocompetent patients with primary cutaneous nocardiosis can be empirically treated with trimethoprim/sulfamethoxazole (TMP/SMX). Empiric dual or triple therapy with TMP/SMX plus amikacin and/or imipenem is suggested for all other patients. B Mortality rates for pulmonary nocardiosis range from 30% to 40%; rates for CNS and disseminated disease approach 50% to 60%. B Background Nocardia is an aerobic, Gram-positive bacterial rod that is variably acid-fast. Nocardiosis is often an opportunistic infection but can cause disease in immunocompetent hosts. Nocardia causes a wide variety of clinical infections, including primary or chronic cutaneous disease, mycetoma (an invasive subcutaneous skin infection), pulmonary disease, CNS disease, ocular involvement, and disseminated infection. Incidence In the United States, about 500 to 1000 new cases of nocardiosis occur each year. The incidence is rapidly growing, due to increasing numbers of immunocompromised patients. 30 0.6% of all transplant recipients will develop nocardiosis; however, 2% of lung transplant recipients are affected. 29 31 28 Causes of the Condition | Nocardia species are native to soil and decaying plants. Nocardia asteroides, recently subdivided into three distinct subspecies (N. asteroides sensu stricto, N. nova, and N. farcinica), accounts for over 80% of nocardiosis infections in the United States, most of which are primary pulmonary disease. 30 24 25 26 27 N farcinica is considered the most virulent, leading to higher numbers of blood and CNS infections. 23 N brasilensis most commonly leads to cutaneous infection, causing more than 90% of chronic, invasive mycetomas. 22 Pathophysiology | Nocardiosis has a subacute time course. The average time from onset of symptoms to diagnosis is 30 to 40 days. 21 25 Cutaneous Nocardia infection results from direct innoculation of the skin with bacteria, usually from contaminated soil. The most common injury reported is pricking of the skin with a thorn or similar object. Untreated disease can lead to a chronic inflammatory state and mycetoma. 20 Inhalation of bacteria on dust particles leads to pulmonary disease. 24 25 Nocardia organisms are facultative intracellular pathogens and are inhibited by neutrophils and monocytes. T cells fight Nocardia organisms by activating cellular immunity and killing the organisms through direct contact. 19 Risk Factors | Risk Factor Immunocompromised state High-dose steroid therapy Cytomegalovirus (CMV) infection in the last 6 months High calcineurin inhibitor levels HIV/AIDS with CD4 less than 20 Male sex Tumor necrosis factor-alpha (TNF-alpha) inhibitor therapy Prior corneal trauma or surgery References: Diagnosis Bottom Line Suspect nocardiosis when a patient presents with a brain, soft tissue, or cutaneous abscess and a recent or current radiographic pneumonia, particularly if immunocompromised. C 21 Perform Gram stain, acid-fast staining, culture, and antimicrobial susceptibility testing on clinical samples for all patients with suspected nocardiosis. Notify the laboratory, as cultures take 10 to 14 days. C 14 31 16s rRNA PCR molecular techniques are used to identify Nocardia species rapidly even after antibiotic therapy has been initiated. C 13 14 Appropriate imaging includes CXR or chest CT scan for suspected pulmonary nocardiosis, brain CT or MRI with contrast for suspected CNS disease, and helical CT scan to delineate mycetoma. C 12 22 28 31 Differential Diagnosis | Diagnosis Features CUTANEOUS Bacterial infection (Staphylococcus, eripsylas, tularemia) Acute verus subacute presentation; Gram stain, acid-fast stain, culture Fungal infection (Aspergillus, Cryptococcus, Gram stain, acid-fast stain, culture, KOH Sporothrix) preparation Nontuberculous Mycobacterium (M chelonae, M fortuitum, M marinum) Acid-fast stain, culture Parasitic infection (cutaneous leishimaniasis) Gram stain, acid-fast stain, culture PULMONARY Bacterial infection (Pseudomonas, Klebsiella, Rhodococcus) Acute versus subacute presentation; Gram stain, acid-fast stain, culture; cavitary lesions on CXR Fungal infection (Cryptococcus, Aspergillus, Gram stain, acid-fast stain, culture, KOH mucormycosis) preparation Mycobacterial infection (M. tuberculosis, Acid-fast stain, culture. M. avium complex, M. kansasii) Primary malignancy or metastasis Gram stain, culture; biopsy and pathologic review CENTRAL NERVOUS SYSTEM Bacterial infection (including anaerobic organisms) Gram stain, acid-fast stain, culture; concentric ring enhancement on CT/MRI Parasitic infection (toxoplamosis, cysteriosis) Gram stain, acid-fast stain, culture Fungal infection (Cryptococcus, Aspergillus, Gram stain, acid-fast stain, culture, KOH mucormycosis, coccidiomycosis) preparation Malignancy (primary brain tumor, lymphoma, metastatic disease) Gram stain, culture; biopsy and pathologic review Using the History and Physical | Dermatologic nocardiosis presents with cellulitis, abscess formation, and subcutaneous nodules in primary disease. Chronic mycetoma, an invasive subcutaneous skin infection, develops from a painless nodule at the innoculation site, which progresses into a chronic granulomatous inflammatory state with formation of invasive sinus tracts that exude sulfur granules. Pulmonary nocardiosis presents with cough (78%), fever/night sweats (74%), dyspnea (60%), fatigue (43%), and chest pain (28%). 11 21 25 Symptoms of CNS infections include focal neurologic deficits (42%), seizures (30%), headache, fever, and nausea/vomiting. 10 Ocular nocardia leads to symptoms of eye pain, blurry vision, photophobia, foreign body sensation, discharge, and edema. Examination may reveal conjunctival injection, chemosis, yellowish nodules or cottonball exudates, and corneal opacification. Selecting Diagnostic Tests | Gram stain, acid-fast staining, and culture are mainstays of nocardiosis diagnosis. Cultures take an average of 10 to 14 days to grow; therefore, the clinician should notify the laboratory if nocardia is suspected. Perform susceptibility testing on all isolates to guide antimicrobial therapy. 14 31 16s rRNA PCR molecular techniques can be used to identify nocardia species rapidly, although this test is not widely available. The test is 90% sensitive and is virtually 100% specific. 14 PCR techniques can be used after antibiotic therapy, as PCR does not require viable cells. 13 HIV testing is recommended in patients with nocardiosis who do not have another predisposing risk factor for immunosuppression. 25 CXR: in patients with pulmonary disease, 27% have lobar or multilobar consolidation (which may contain ring-enhancing cavitary lesions), 83% have pulmonary nodules (31% have multiple nodules), and 19% have pleural effusions. 11 21 Brain imaging: may reveal parenchymal lesions with surrounding concentric enhancement and mass effect. 9 10 12 CT scan of mycetoma may be useful to map the depth of invasion into soft tissue, muscle, blood vessels, and bone. 22 Treatment Bottom Line Immunocompetent patients with primary cutaneous nocardiosis can be empirically treated with TMP/SMX. Empiric dual or triple therapy with TMP/SMX plus amikacin and/or imipenem is suggested for all other patients. B 7 8 15 Treat immunocompetent patients with cutaneous disease for a minimum of 6 months. Treat all other patients for up to a year or longer. B 6 25 28 Drug Therapy | Table 1 summarizes the effectiveness of various antibiotics for various Nocardia syndromes. Both in vitro and clinical data demonstrate excellent efficacy for TMP/SMX against almost all strains of Nocardia. 5 15 21 In vivo studies are lacking for most antibiotics, but favorable susceptibility profiles have been demonstrated for linezolid, moxifloxacin, tigecycline, imipenem and, to a lesser extent, meropenem, amikacin, and minocycline. 5 7 21 29 32 For localized primary cutaneous nocardiosis in immunocompetent hosts, initial monotherapy with TMP/SMX is adequate, dosed at 5 mg/kg of trimethoprim in two divided doses. Minocycline or amoxicillin/clavulanate are reasonable alternatives for patients with sulpha allergies. 7 8 15 For mycetoma, pulmonary, CNS, or disseminated disease, and for immunocompromised patients, empiric dual or even triple parenteral therapy is warranted until culture sensitivities are available. TMP/SMX (15 mg/kg IV divided into 2 - 4 doses) plus amikacin (7.5 mg/kg IV q12h) and/or imipenem (500 mg IV q6h) are good choices. 28 4 21 24 Antibiotics can be tailored to species and susceptibility data, as they become available. Continue antibiotic therapy for a minimum of 6 months for immunocompetent patients. Patients with disseminated or CNS disease and immunocompromised patients should continue therapy for at least 1 year. 6 25 28 Surgical Therapy | Back to Top Surgical resection may be required in combination with antibiotics for deep infections Treat all brain abscesses greater than 2.5 cm with aspiration in conjunction with antibiotics. If the lesions do not improve within 2 weeks of appropriate therapy, or if clinical condition worsens, craniotomy may be required. 10 When to Refer or Hospitalize | Consider an infectious disease consultation for all patients with suspected nocardiosis. Refer patients with eye involvement to an ophthalmologist. Myocardial infarction Essential Evidence Last Updated on 2012-10-15 © 2012 John Wiley & Sons, Inc. Authors: Jack Rubinstein, MD, Michigan State University Mark Ebell, MD, MS, Associate Professor Kalpana R. Prakasa, MD, Johns Hopkins University Editors: Gary Ferenchick, MD, Chief, Division of General Medicine, Michigan State University Jonathan Murrow, MD, Associate Editor, Georgia Health Sciences University, Athens, Georgia Overall Bottom Line Elevated cardiac enzymes associated with clinical or ECG evidence of ischemia is diagnostic for myocardial infarction (MI). A 79 Treat all patients with oxygen, pain control medications, and antiplatelet therapy including aspirin and heparin (or enoxaparin). A 78 Treat most patients with aspirin or clopidogrel, beta-blockers, and statins (low-density lipoprotein [LDL] target of 70-100 mg/dL) if no contraindications are noted. A 78 Patients treated promptly with adequate medical and interventional therapy have inhospital mortality rates of 2% to 4% and 1-year mortality of 8% to 10%. A 25 Background Myocardial infarction is evidence of myocardial necrosis in a patient with evidence of decreased perfusion from coronary artery disease (CAD). 79 Incidence 1.3 million patients are admitted to hospital with unstable angina/non-ST-elevation MI (UA/NSTEMI) and 350,000 with ST elevation MI (STEMI) in the United States every year. 80 Prevalence | Between 2.1% and 6.1% of the population have coronary heart disease, depending largely on geographic and socioeconomic factors. 77 Economic Impact | CAD is projected to cost an estimated $151.6 billion in direct and indirect costs in 2007 in the United States. 76 Causes of the Condition | Complete or partial occlusion of a coronary artery by plaque, typically complicated by rupture and possibly vasospasm. Increased myocardial demand with decreased supply from advanced atherosclerotic plaque. Complete or partial occlusion of a coronary artery associated with angioplasty, stent placement or thrombosis, or bypass surgery. 79 Pathophysiology | STEMI is usually caused by plaque rupture from nonobstructive but vulnerable plaques. The vulnerable atherosclerotic plaque has a rich lipid core, a thin fibrous cap, many T lymphocytes, and fewer smooth muscle cells. When the plaque erodes it exposes the thrombogenic subendothelial basement membrane to the circulation, which is followed by acute thrombosis, coronary occlusion, and myocardial necrosis. Non-ST segment elevation myocardial infarction (NSTEMI) is commonly caused by advanced atherosclerotic plaque with thrombosis that is not occlusive and may be associated with increased myocardial demand. 80 Coronary vasospasm may worsen the coronary occlusion. 75 Risk Factors | Risk Factor Odds Ratio Active smoking 2.87 (2.72-3.20) Passive smoking 1.25 (1.17-1.32) Hypertension 2.48 (2.30-2.68) Diabetes 3.08 (2.77-3.42) Abdominal obesity 2.24(2.06-2.45) Pneumonia (chlamydia) Essential Evidence Last Updated on 2012-10-06 © 2012 John Wiley & Sons, Inc. Authors: Robert Kraft, MD, Assistant Clinical Professor, University of Kansas School of Medicine, Wichita Editors: Mindy Smith, MD, MS, Professor, Department of Family Medicine, Michigan State University Linda French, MD, Professor and Chair, Department of Family Medicine, University of Toledo Overall Bottom Line No single clinical or radiographic finding or constellation of findings accurately differentiates community-acquired pneumonia (CAP) caused by Chlamydophila pneumoniae (formerly Chlamydia pneumoniae) from any other cause. C No accurate, rapid, widely available diagnostic test exists to identify C. pneumoniae. B Treatment of undifferentiated CAP should be empiric and dictated by local microbial patterns and antibiotic resistance patterns; specific coverage of C. pneumoniae in patients with undifferentiated CAP does not reduce mortality. B Treatment of culture or serologically proven C. pneumoniae includes doxycycline or a macrolide as first-line therapy, or a fluoroquinolone as an alternative. B Background Chlamydia pneumonia is a LRTI caused by the atypical pathogen Chlamydophila pneumoniae. Incidence Exact incidence is unknown; estimates are 100 cases/100,000/year. New cases, as a percentage of all cases of CAP, range from 0% to 44% and vary by population studied and diagnostic methods used. 1 Lack of standardized diagnostic methods adds to the difficulty in estimating incidence. Other Impact | C. pneumoniae is a potential cause of pneumonia outbreaks in the nursing home setting. 2 Seropositivity to chlamydia heat shock protein-60 antibodies, a marker of chronic chlamydial infection, is associated with increased risk for subsequent lung cancer (OR, 1.30; 95% CI, 1.02-1.67). 3 A similar increased increase risk of lung cancer with C. pneumoniae infection was found in a meta-analysis (OR 1.16; 95% CI, 1.00-1.36 in prospective studies and OR 2.17; 95% CI, 1.79-2.63 in retrospective studies). 16 There is an association between both Chlamydophila pneumoniae (OR 6.34; 95% CI, 2.83-14.19; p < 0.001) and Chlamydophila psittaci (OR 29.05; 95% CI, 8.91-94.70; p < 0.001) and schizophrenia. 17 Persistent C. pneumoniae infection also appears to be associated with overweight/obesity. 18 Causes of the Condition | C. pneumoniae Pathophysiology | Chlamydia pneumonia is a CAP caused by C. pneumoniae, an obligate intracellular bacteria. C. pneumoniae infection is probably widespread (with over 50% of children testing positive for prior exposure), but symptoms are either mild or not present. Immunity to infection does not last long, making recurrent or persistent infection possible. Pneumonia (chlamydia) Essential Evidence Last Updated on 2012-10-06 © 2012 John Wiley & Sons, Inc. Authors: Robert Kraft, MD, Assistant Clinical Professor, University of Kansas School of Medicine, Wichita Editors: Mindy Smith, MD, MS, Professor, Department of Family Medicine, Michigan State University Linda French, MD, Professor and Chair, Department of Family Medicine, University of Toledo Overall Bottom Line No single clinical or radiographic finding or constellation of findings accurately differentiates community-acquired pneumonia (CAP) caused by Chlamydophila pneumoniae (formerly Chlamydia pneumoniae) from any other cause. C No accurate, rapid, widely available diagnostic test exists to identify C. pneumoniae. B Treatment of undifferentiated CAP should be empiric and dictated by local microbial patterns and antibiotic resistance patterns; specific coverage of C. pneumoniae in patients with undifferentiated CAP does not reduce mortality. B Treatment of culture or serologically proven C. pneumoniae includes doxycycline or a macrolide as first-line therapy, or a fluoroquinolone as an alternative. B Diagnosis Bottom Line No single clinical or radiographic finding or constellation of findings accurately differentiates CAP caused by C. pneumoniae from any other cause. C6-8 6 No accurate, rapid, widely available, and validated diagnostic test exists for identification of C. pneumoniae. C 1 Sputum or nasopharyngeal swab culture is considered the gold standard of diagnosis but is not recommended for routine use in patients with CAP. C Differential Diagnosis | Diagnosis Typical pneumonia (Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis) Features No clinically significant differences Atypical pneumonia ( Mycoplasma pneumoniae, Legionella No clinically significant differences spp. ) Aspiration pneumonia High-risk populations, history of choking or aspiration Viral pneumonia No clinically significant differences Zoonotic pneumonia (Chlamydia psittaci, Coxiella burnetii, Specific exposure history Francisella tularensis, Yersinia pestis) Fungal pneumonia (histoplasmosis, blastomycosis) Specific exposure history, pulmonary granulomas Tuberculosis Exposure history, positive purified protein derivative Using the History and Physical | Symptoms of C. pneumoniae pneumonia are the same as for CAP of any cause, including cough, fever, and dyspnea. Physical examination findings could include abnormal breath sounds (eg, crackles), tachypnea, and signs of hypoxemia (eg, cyanosis). Patients with C.pneumoniae LRTI tend to have symptoms that develop more gradually and have less cough than typical pathogens. However, no individual finding or constellation of signs and symptoms can accurately differentiate pneumonia caused by C. pneumoniae from any other cause of CAP. 6 Selecting Diagnostic Tests | CXR cannot differentiate CAP caused by C. pneumoniae from other pathogens, but it is used as a prognostic factor. 7-8 7 Sputum or nasopharyngeal swab culture is considered the reference standard, but it is difficult and slow, has a variable yield, and has limited availability. Polymerase chain reaction (PCR) with enzyme immunoassay is promising as a rapid diagnostic test but is not standardized or validated; 9 19 PCR and IgM serology appear to be more sensitive than culture. 10 The Centers for Disease Control and Prevention considers a single IgM titer of 1:16 or higher or a 4-fold increase in IgG titer by microimmunofluorescence as the only acceptable serologic test for C. pneumoniae, yet titers still suffer from poor sensitivity (25% compared with culture). 1 Acute and convalescent IgG titers are more sensitive than a single time-point titer but do not offer rapid diagnosis. Approach to the Patient | Follow diagnostic guidelines (history, physical examination, CXR, and other selected studies) for CAP. 11 Specific tests for chlamydia (eg, PCR or antibody titers) are not widely available or clinically useful. 1 Refer to chapter on Pneumonia (community acquired pneumonia) for more on management. Mitral insufficiency Essential Evidence Last Updated on 2012-10-06 © 2012 John Wiley & Sons, Inc. Authors: Barry Ziring, MD, Acting Director of Internal Medicine, Thomas Jefferson University Harnish Chawla, MD, Department of Internal Medicine, Thomas Jefferson University Editors: Gary Ferenchick, MD, Chief, Division of General Medicine, Michigan State University Linda French, MD, Professor and Chair, Department of Family Medicine, University of Toledo Mark Ebell, Associate Editor Jonathan Murrow, Associate Editor Overall Bottom Line Physical examination is the best initial screening for mitral regurgitation (MR). C Echocardiography is useful for diagnosing and monitoring the severity of MR (see Figure 1). A Medical therapy is reserved for symptomatic patients only and is aimed at decreasing afterload. It is not a substitute for surgical therapy. B Surgical therapy is indicated in patients with congestive heart failure (CHF) or symptoms secondary to severe MR or in asymptomatic patients with structural changes of the left ventricle. A Background Mitral insufficiency, or MR, is a valvular disorder involving any of the following: the mitral leaflets, annulus, chordae tendineae, and papillary muscles, resulting in abnormal leaking of blood across the mitral valve (MV), ie, from the left ventricle to the left atrium. Prevalence Mitral valve prolapse (MVP) is present in approximately 4% of the normal healthy population. 11 MR affects about 5 in 10,000 people and is the second most common valvular disease behind aortic stenosis. 11 Causes of the Condition | Causes of MR can be divided into primary and secondary causes. Primary: In developed countries, MVP is the most common cause of MR. In developing countries, rheumatic heart disease is the most common cause of MR. Other primary causes include infective endocarditis, trauma, drug-induced MR, and congenital MR. Certain medications that can interact with 5-hydroxytryptamine 2B receptors on cardiac valves ( eg, pergolide and cabergoline) increase the risk of valvular regurgitation by 5% to 7%. 15 An enlarged ventricle can predispose a patient to MR. These secondary causes are (in order of frequency) ischemic heart disease, left ventricular (LV) systolic dysfunction, and hypertrophic cardiomyopathy. Pathophysiology | Pathophysiology largely depends on the cause of MR as described above. In general MR involves a transition from an asymptomatic compensated stage to a symptomatic decompensated stage. The rate at which this transition occurs is variable and is also dependent on the process causing the MR. Diagnosis Bottom Line The murmur of MR 3 is a holosystolic murmur heard best over the apex and radiating to the axilla, with a blowing and high-pitched quality; it becomes louder with squatting or handgrip and softer with standing or Valsalva. C Echocardiogram is the gold standard for establishing and diagnosing the severity of MR and is indicated in any patient suspected of having MR. B 17 Differential Diagnosis | Diagnosis Tricuspid Features Murmur intensity increases with inspiration regurgitation Aortic stenosis Murmur heard best in the upper right second intercostal space; harsh crescendo-decrescendo murmur Ventricular septal defect Heard best along the lower left sternal border; difficult to distinguish on auscultation from MR Diagnostic Criteria | Back to Top American Society of Echocardiography criteria for the diagnosis of severe MR: regurgitant orifice area greater than.40, regurgitant volume greater than 60 mL, regurgitant fraction greater than 50%, jet area greater than 40% of left atrial area. Severe MR should exist with left ventricular enlargement. Left atrial enlargement (LAE) may reflect duration and severity of MR. 10 Using the History and Physical | Clinical manifestations of MR depend on its severity. Patients with mild and moderate MR are often asymptomatic, and patients with severe MR can be symptomatic or asymptomatic. The most common symptoms in severe MR are exertional dyspnea and fatigue. MR can present with new-onset atrial fibrillation. The classic murmur of MR 3 is a holosystolic murmur heard best over the apex and radiating to the axilla, with a blowing and high-pitched quality. The murmur becomes louder with increased afterload ( eg, squatting, handgrip) and softer with decreases in preload (standing, Valsalva). It is also louder in patients with increased LV volume ( eg, heart failure, leg raising, lying down). The S1 is diminished secondary to inability of MV leaflets to close properly. If MR causes a dilated left ventricle, S3 may be present as well as lateral displacement of apical impulse. MVP is characterized by middle to late systolic click. However, it is only 10% sensitive and had a positive predictive value of 17% ( ie, only 17% of those with a click have MVP by ECHO). 14 Selecting Diagnostic Tests | ECG may show LAE, left ventricular hypertrophy (LVH), and ST-T segment abnormalities. CXR may show cardiomegaly from LVH and LAE. Calcification of MV may also be seen. Echocardiogram is the gold standard for establishing and diagnosing the severity of MR and is indicated in any patient suspected of having MR. 17 B-natriuretic peptide (BNP) is recommended only for patients with suspected or known heart failure. It has not been shown to have any diagnostic utility in grading the severity of MR. However, there is some evidence to suggest a correlation of elevated BNP levels with poor clinical outcome in patients with MR. 13 Clinical Decision Rules | A clinical decision rule has been developed and validated that predicts the likelihood a patient will need pacing after valve surgery. It is based on the patient's age, type of surgery, preoperative ECG, and history of previous valve surgery. Approach to the Patient | See algorithm in Figure 1 for a suggested approach to evaluation and management. History and Physical Tests | Systolic murmur -> mitral regurgiation and VSD Pretest Probability (%): 40.0 Probability of disease when test outcome is: Test Name Increase with transient bilateral brachial arterial occlusion Positive (LR+) Negative (LR-) 94.5% (26) 12.8% (0.2) Increase with 1 minute handgrip exertion 85.0% (8.5) 18.9% (0.4) Decrease with amyl nitrate inhalation 5.2% (0.2) Valve disease suspected -> mitral regurgitation 66.7% (8.0) Pretest Probability (%): 10.0 Probability of disease when test outcome is: Test Name Auscultation with stethoscope Positive (LR+) Negative (LR-) 12.6% (1.3) 9.5% (0.9) Valve disease suspected -> detecting any murmur Pretest Probability (%): 10.0 Probability of disease when test outcome is: Test Name Auscultation with stethoscope Positive (LR+) 17.4% (1.9) Negative (LR-) 4.7% (0.4) Diagnostic Tests | Cardiac disease -> LA enlargement Pretest Probability (%): 50.0 Probability of disease when test outcome is: Test Name Chest x-ray Positive (LR+) 88.5% (7.7) Negative (LR-) 29.1% (0.4) Treatment Bottom Line Vasodilators are not recommended for asymptomatic patients with chronic MR. A 9 Medical therapy is reserved for symptomatic patients and is directed at decreasing afterload with vasodilators ( ie, hydralazine and nitroprusside) as a bridge to surgery. B 8 17 Indications for surgery are the following: acute MR with CHF or cardiogenic shock, class II/III/IV symptoms with EF>30% and LV end diastolic dimension >55mm, asymptomatic with ejection fraction (EF) between 30% and 60% and end systolic dimension greater than or equal to 40 mm. A 17 18 Drug Therapy | Medical therapy is directed at increasing forward flow from the LV. Therapy is generally reserved for symptomatic patients, because in asymptomatic patients it could mask the development of symptoms and thus an indication for surgery. 9 Beneficial effect is seen in acute vasodilator therapy with nitroprusside and hydralazine for symptomatic patients as a bridge for patients who are candidates for surgery. 8 For chronic MR patients with depressed LV function who are not surgical candidates, afterload reduction with ACE-I, β blockers, diuretics should be considered. 7 For patients with MR and atrial fibrillation, calcium channel blockers, β blockers for rate control, and anticoagulation with warfarin should be used. 7 Patients who have had a mechanical heart valve replacement should undergo lifetime anticoagulation. A Cochrane review found that adding a low dose of aspirin (100 mg/day) to oral anticoagulation reduces the risk of embolism or death, but increases the risk of major bleeding. 17 Surgical Therapy | In patients with severe chronic MR, surgery is indicated for patients with symptoms, asymptomatic patients with abnormalities in LV size and LV dysfunction, pulmonary hypertension, and new-onset atrial fibrillation. 17 In asymptomatic patients with severe chronic MR, surgery is indicated for left ventricular ejection fraction (LVEF) of 30% to 60% and/or end systolic dimension greater than 40 mm. 17 In general, MV repair is preferred over MV replacement, because many studies have demonstrated improved LV function and survival in patients undergoing valve repair. This is generally better performed at an experienced surgical center. See Table 1. 12 When MV replacement is indicated, a bioprosthetic valve should be used in patients who cannot or refuse to take warfarin and in patients older than 65 years. 17 If a patient is younger than 65 years and has a history of long standing atrial fibrillation a mechanical valve is generally recommended. Among patients younger than 65 years and who are in sinus rhythm, education of the patient and patients preference plays a role as there is no clear evidence supporting one decision or the other. Coronary angiography is generally recommended for high risk coronary artery disease patients before MV surgery as bypass surgery may be recommended concurrently with MV surgery. Rehabilitation and Physical Therapy | Patients who have undergone surgery should not participate in any sport that may cause body contact because of the possibility that the MV repair will be disrupted. Prognosis Bottom Line Primary valve failure occurs in 44% receiving a bioprosthetic valve versus 4% receiving a mechanical valve ( older than 15 years). B 6 After 15 years, all-cause mortality was the same between mechanical and bioprosthesis valves (81% vs 79% ). B 6 Natural History | MVP is not associated with an increase stroke risk. 12 MVP is not associated with any adverse cardiovascular outcomes. 14 Prognosis | In a 15-year follow-up period, patients undergoing MV replacement showed primary valve failure in 44% of those receiving a bioprosthetic valve versus 4% of those receiving a mechanical valve. 5 After 15 years, all-cause mortality was the same between mechanical and bioprosthesis valves (81% and 79%, respectively). 5 Follow-up tests and monitoring | For chronic MR, serial monitoring with echocardiography is important in recognizing the transition from a compensated to decompensated state and the need for surgical intervention. Patients with mild MR should be seen yearly for history and physical. 17 Patients with moderate MR should be seen yearly and have repeat echocardiograms at these visits. 17 Patients with severe MR should be seen every 6 to 12 months or sooner if symptoms occur. 17 Advice for patients | | No contact sports; these sports may dislodge the valve. Emphasize importance of antibiotic prophylaxis and if necessary anticoagulation.