* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Heart Failure With Improved Ejection Fraction: Clinical
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Rheumatic fever wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
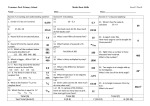
Original Article Heart Failure With Improved Ejection Fraction: Clinical Characteristics, Correlates of Recovery, and Survival Results From the Valsartan Heart Failure Trial Viorel G. Florea, MD, PhD, DSc; Thomas S. Rector, PhD; Inder S. Anand, MD, FRCP, D.Phil (Oxon.); Jay N. Cohn, MD Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 Background—Heart failure with recovered or improved ejection fraction (HFiEF) has been proposed as a new category of HF. Whether HFiEF is clinically distinct from HF with persistently reduced ejection fraction remains to be validated. Methods and Results—Of the 5010 subjects enrolled in the Valsartan Heart Failure Trial (Val-HeFT), 3519 had a baseline left ventricular EF of <35% and a follow-up echocardiographic assessment of EF at 12 months. Of these, 321 (9.1%) patients who had a 12-month EF of >40% constituted the subgroup with HFiEF. EF improved from 28.7±5.6% to 46.5±5.6% in the subgroup with HFiEF and remained reduced (25.2±6.2% and 27.5±7.1%) in the subgroup with HF with reduced ejection fraction. The group with HFiEF had a less severe hemodynamic, biomarker, and neurohormonal profile, and it was treated with a more intense HF medication regimen. Subjects who had higher blood pressure and those treated with a β-blocker or randomized to valsartan had greater odds of being in the HFiEF group, whereas those with an ischemic pathogenesis, a more dilated left ventricle, and a detectable hs-troponin had lower odds of an improvement in EF. Recovery of the EF to >40% was associated with a better survival compared with persistently reduced EF. Conclusions—Our data support HFiEF as a stratum of HF with reduced ejection fraction with a more favorable outcome, which occurs in a minority of patients with HF with reduced ejection fraction who have a lower prevalence of ischemic heart disease, a less severe hemodynamic, biomarker, and neurohormonal profile, and who are treated with a more intense HF medication regimen. Clinical Trial Registration—URL: http://www.clinicaltrials.gov. Unique identifier: NCT00336336. (Circ Heart Fail. 2016;9:e003123. DOI: 10.1161/CIRCHEARTFAILURE.116.003123.) Key Words: biomarker ■ blood pressure C urrent guidelines for the management of heart failure (HF) divide patients with HF into 2 categories: those with reduced ejection fraction (EF of ≤40%; HFrEF) and those with preserved ejection fraction (>40%; HFpEF).1 It has been recognized that a subset of patients with HFpEF previously had HFrEF.2 These patients with recovery or improvement in EF (HFiEF) may be clinically distinct from those with persistently preserved or reduced EF.1,2 ■ heart failure ■ prognosis ■ valsartan In this post hoc analysis of the Valsartan Heart Failure Trial (Val-HeFT)5 database, we characterized the subjects who had improved their EF during the first 12 months of follow-up, evaluated the independent correlates of EF improvement, and determined whether their all-cause mortality was substantially different from the subjects whose EF remained reduced. Methods See Editorial by Basuray and Fang See Clinical Perspective Study Design and Patient Selection Val-HeFT was a randomized, placebo-controlled, double-blind trial that enrolled 5010 patients with New York Heart Association functional class II to IV HF and an EF of <40% designed to evaluate the efficacy of valsartan. All-cause mortality was one of the 2 primary Val-HeFT end points5. Valsartan treatment did not exhibit a statistically significant effect on mortality, but stratification by baseline severity of left ventricular remodeling influenced the results. Patients with worse left ventricular internal diastolic diameter (LVIDd) and EF were at highest risk of an event and gained the most antiremodeling effect and clinical benefit with valsartan treatment.6 Val-HeFT was approved by the institutional review board at each center, and all subjects provided a written informed consent. In 2011, Punnoose et al2 reported that nearly 70% of patients with symptomatic HFpEF had recovered from a previously low EF. These patients were clinically distinct from those with HFpEF and more similar to the HFrEF population from which they initially arose. Further studies found that HFiEF is associated with a better biomarker profile, quality of life, and event-free survival than continued HFrEF and HFpEF3,4 but still experience a significant number of HF hospitalizations, suggesting persistent HF risk.3 Received January 25, 2016; accepted May 27, 2016. From the Division of Cardiology (V.G.F., I.S.A.) and Center for Chronic Disease Outcomes Research (T.S.R), Minneapolis Veterans Affairs Health Care System, MN; and Department of Medicine, University of Minnesota, Minneapolis (V.G.F., T.S.R., J.N.C.). Correspondence to Viorel G. Florea, MD, PhD, DSc, Department of Medicine, Minneapolis VA Health Care System, Cardiology 111C, One Veterans Dr, Minneapolis, MN 55417. E-mail [email protected] © 2016 American Heart Association, Inc. Circ Heart Fail is available at http://circheartfailure.ahajournals.org DOI: 10.1161/CIRCHEARTFAILURE.116.003123 1 2 Florea et al Heart Failure With Improved Ejection Fraction Table 1. Baseline Characteristics of Study Participants HFiEF (n=321) HFrEF (n=3198) 61±11 62±11 HFiEF (n=321) HFrEF (n=3198) P Value Spironolactone, % 4 5 0.50 Digoxin, % 66 68 0.48 P Value Demographics and History Age, y (mean±SD) Table 1. Continued 0.02 Male sex, % 74 80 0.02 Diuretics, % 82 86 0.05 White race, % 90 90 0.86 Aspirin, % 38 40 0.54 Ischemic pathogenesis, % 37 56 <0.001 Statin, % 26 33 0.01 H/o diabetes mellitus, % 24 25 0.62 Amiodarone, % 11 13 0.18 H/o hypertension, % 12 6 <0.001 H/o atrial fibrillation, % 15 11 0.07 H/o COPD, % 10 12 0.20 Symptoms and physical examination Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 NYHA class III or IV, % 34 37 0.34 Orthopnea, % 26 28 0.44 Edema, % 19 16 0.22 PND, % 7 8 0.27 S3, % 22 26 0.09 JVD, % 13 13 0.72 Rales, % 10 11 0.77 Systolic BP, mm Hg 127±20 124±18 <0.001 Diastolic BP, mm Hg 78±12 76±10 <0.01 Heart rate, beats per minute 74±13 73±12 0.49 BMI, kg/m 27±5 27±4 0.86 LVEF, % 28.7±5.6 25.2±6.2 <0.001 LVIDd/BSA, cm/m2 3.5±0.5 3.7±0.5 <0.001 4±2 4±2 0.92 Hemoglobin, g/dL 14±1 14±1 0.45 Hematocrit, % 41±5 41±4 0.32 Sodium, mmol/L 140±3 139±3 <0.05 Potassium, mmol/L 4.4±0.6 4.4±0.6 0.28 Total protein, g/dL 72±5 72±6 0.62 Albumin, g/dL 4.2±0.3 4.2±0.3 0.19 Creatinine, mmol/L 107±22 112±26 <0.001 7±3 8±3 <0.01 62±15 59±16 <0.001 2 Clinical chemistry BUN, mg/dL eGFR, mL/min per 1.73 m2 Uric acid, mg/dL Echocardiographic Measurements of Left Ventricular Performance Echocardiography, both the recording and interpretation, was carried out at 291 multinational sites. Participation in the trial was dependent on meeting specific core laboratory standards for recording and reading of LVIDd from 2 dimensionally directed M-mode echocardiography, and EF was derived from LV volumes using the area–length method.7 During the trial, quality control was monitored from random sampling of patient studies, and this was satisfactorily maintained.8 Serial echocardiograms in 5010 patients were obtained at baseline before randomization and at 4, 12, 18, 24, and 30 months after randomization. Biochemical Measurements Echocardiography Neutrophils, % ACE indicates angiotensin-converting enzyme; BMI, body mass index; BNP, B-type natriuretic peptide; BP, blood pressure; BUN, blood urea nitrogen; COPD, chronic obstructive pulmonary disease; eGFR, estimated glomerular filtration rate; HFiEF, heart failure with improved ejection fraction; H/o, history of; HFrEF, heart failure with reduced ejection fraction; JVD, jugular venous distention; LVEF, left ventricular ejection fraction; LVIDd/BSA, left ventricular internal diastolic dimension corrected for body surface area; NYHA, New York Heart Association; PND, paroxysmal nocturnal dyspnea; S3, third heart sound; and WBC, white blood cell. 7±2 7±2 0.22 Cholesterol, mg/dL 211±48 204±48 0.01 Triglycerides, mg/dL 197±193 190±175 0.48 Medications ACE-inhibitor, % 93 93 0.68 Valsartan,% 58 49 <0.01 β-Blocker, % 47 34 <0.001 (Continued ) A complete blood cell count and measurements of serum albumin, uric acid, creatinine, and blood urea nitrogen were performed at a central laboratory with a commercially automated system at randomization and after 4, 6, 12, 18, and 24 months. Glomerular filtration rate was estimated using the Modification of Diet in Renal Disease equation.9 Other variables used in this analysis included neurohormones (B-type natriuretic peptide [IRMA Shionogi] and N-terminal probrain natriuretic peptide [ECLIA Elecsys 2010 analyzer, Roche Diagnostics]) measured by commercially available assays,10 norepinephrine [high-performance liquid chromatography with electrochemical detection],11 endothelin I, big endothelin, plasma renin activity and aldosterone [by radioimmunoassay], high-sensitivity troponin T,12 high-sensitivity C-reactive protein,13 galectin-3,14 soluble ST2,15 and growth-differentiating factor 15.16 Statistical Analysis Distributions of continuous variables are described using means and SDs and categorical variables as proportions expressed as percentages. Highly skewed continuous distributions are described by the median and the interquartile range and were transformed using natural logarithms for regression analyses. Baseline characteristics of the HFiEF and continued HFrEF groups were compared using a t test, Rank-sum test or χ2 test as appropriate for the level of measurement and distribution of the variable. Stepwise forward and backward logistic regression with a P value <0.10 required for entry or removal was used to identify independent correlates of substantial improvements in EF forcing the baseline EF into the model to help control for the inverse relationship between baseline EF measurements and changes in EF. First, all 42 baseline variables described in Table 1 were tested along with an indicator of subjects in the United States. Then the baseline neurohormones and cardiac biomarkers listed in Table 2 that were measured in at least 3 Florea et al Heart Failure With Improved Ejection Fraction 80% of 3519 subjects (norepinephrine, plasma renin activity, aldosterone, B-type natriuretic peptide, C-reactive protein, and troponin) were tested for addition to the 7 independent correlates from Table 1. These regression analyses were clustered by the study center to estimate robust SEs. Discrimination provided by the logistic regression model containing the independent correlates was examined by the estimated probabilities of being in the HFiEF group and the area under the receiver operating characteristic curve. Survival in the HFiEF and continued HFrEF groups after month 12 is compared using Kaplan–Meier curves and the log-rank test. Mortality rates per 100 person-years were calculated, and the incidence rate ratio was estimated using Poisson regression clustered by the study center. The group discrimination of times to death was assessed by Harrell C index. A P value of <0.05 was considered statistically significant without adjustment for the number of comparisons being made during these exploratory analyses of data from a randomized controlled clinical trial. All analyses were done using version 12.1 of Stata software. The authors had full access to and take full responsibility for the integrity of the data. All authors have read and agree to the article as written. Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 Results Changes in Ejection Fraction Of the 5010 patients enrolled into Val-HeFT, 4997 patients had an echocardiographic assessment of left ventricular EF at baseline. Of these, 4410 met our cohort inclusion criteria of a baseline EF of <35%. Of the 4410 patients, 3519 (80%) had a 12-month EF and were included in our analysis. Of these, 321 patients (9.1%) who had a 12-month EF of >40% constituted the subgroup of patients with HFiEF, and 3198 patients (90.9%) who had a 12-month EF of ≤40% constituted the subgroup of patients with HFrEF. The EF improved from 28.7±5.6% to 46.5±5.6% in the subgroup of patients with HFiEF and remained reduced (25.2±6.2% and 27.5±7.1%) in the comparison group. The 12-month changes in EF were 17.8±8.0% (range, 6%–42%) in the HFiEF group and 2.3±6.7% (range, −27 to 27) in the continued HFrEF group. A significant difference in changes in EF between the subgroups of patients with HFiEF and HFrEF was observed by 4 months after the baseline assessment (8.8±9.0% versus 2.3±6.5% respectively, P<0.001), indicating earlier changes in EF in the 2 subgroups of patients were consistent in their direction and magnitude. Baseline Clinical Characteristics Baseline demographic and clinical characteristics of the study groups with HFiEF and HFrEF are compared in Table 1. Overall, the group with HFiEF had features of less severe HF with higher baseline left ventricular EF and lower baseline LVIDd normalized to body surface area (LVIDd/BSA). This group was marginally younger and less likely to be of male sex compared with the group with HFrEF. Fewer patients in the HFiEF group had an ischemic origin of HF. This group had a higher prevalence of hypertension but a similar prevalence of diabetes mellitus, atrial fibrillation, or chronic obstructive pulmonary disease. Apart from a higher systolic and diastolic blood pressure, subjects with HFiEF had a similar symptomatic profile in respect to orthopnea, edema, paroxysmal nocturnal dyspnea, third heart sound, jugular venous distention, pulmonary rales, heart rate, and prevalence of New York Heart Association class III or IV. Clinical chemistry variables were not different between the 2 groups except for better markers of renal function (creatinine, blood urea nitrogen, and glomerular filtration rate) and higher serum sodium and cholesterol levels in the HFiEF group. More subjects with HFiEF were treated with valsartan and a β-blocker, and fewer subjects with HFiEF were treated with a statin. Neurohormones and Cardiac Biomarkers Available baseline levels of plasma neurohormones and cardiac biomarkers in each of the HF category are presented in Table 2. Overall, the HFiEF group had less severe neurohormonal activation. Plasma norepinephrine, plasma renin activity (PRA), endothelin I, big endothelin, B-type natriuretic peptide, and N-terminal probrain natriuretic peptide were significantly lower in the HFiEF group compared with the HFrEF group. Plasma aldosterone level was also lower in the HFiEF group, but the Table 2. Neurohormones and Cardiac Biomarkers in Study Participants* HFiEF, n=321 Norepinephrine, pg/mL PRA, ng/mL per hour HFrEF, n=3198 P Value 352 (257–505), n=264 381 (270–562), n=2784 0.04 4 (1–12), n=267 5 (2–16), n=2777 <0.01 Aldosterone, pg/mL 94 (62–160), n=243 103 (63–177), n=2638 0.22 Endothelin I, pg/mL 1.0 (0.5–2.4), n=115 1.6 (0.8–2.8), n=1276 <0.01 Big Endothelin, pg/mL 0.8 (0.6–0.9), n=152 0.8 (0.6–1.0), n=1502 0.03 BNP, pg/mL 61 (24–166), n=267 99 (42–234), n=2783 <0.001 565 (224–1386), n=249 903 (393–1910), n=2638 <0.001 NT-proBNP, pg/mL hs-CRP, mg/L 3 (1–7), n=257 3 (1–7), n=2740 0.62 hs-TnT, ng/mL 9 (4–16), n=247 13 (6–22), n=2606 <0.001 Gal-3, ng/mL 15 (13–19), n=100 16 (13–21), n=1082 0.07 GDF-15, ng/L sST2, ng/mL 1757 (1314–2501), n=105 22 (16–30), n=100 2018 (1410–2950), n=1147 24 (19–33), n=1081 0.02 0.02 BNP indicates B-type natriuretic peptide; Gal-3, galectin-3; GDF growth-differentiating factor; HFiEF, heart failure with improved ejection fraction; HFrEF, heart failure with reduced ejection fraction; hs-CRP, high-sensitivity C-reactive protein; hs-TnT, highsensitivity troponin T; NT-proBNP, aminoterminal probrain natriuretic peptide; PRA, plasma renin activity; and sST2, soluble ST2. *Because of skewed distribution, values are presented as median (Quartile 2–Quartile 3). 4 Florea et al Heart Failure With Improved Ejection Fraction of 3 years with a median (interquartile range) of 2 (1.6–2.4) years beyond month 12. During this period, 397 (11.3%) subjects died. Figure shows the Kaplan–Meier survival curves for the HFiEF and continued HFrEF groups. As seen, the proportion surviving was significantly higher in the HFiEF group (log-rank P value=0.005). The mortality rate was 2.9 per 100 person-years (95% confidence interval, 1.8–4.5) in the HFiEF group and 5.8 per 100 person-years (95% confidence interval, 5.3–6.4) in the continued HFrEF group. The unadjusted mortality rate ratio for HFiEF was 0.49 (95% confidence interval, 0.31–0.76; P=0.002). Harrell concordance statistic was 0.52, indicating HFiEF did not discriminate times to death. Figure. Kaplan–Meier curves of time to death in patients with heart failure with reduced ejection fraction (HFrEF) and those with improved ejection fraction (HFiEF). Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 difference did not reach statistical significance. The HFiEF group was also characterized by lower levels of B-type natriuretic peptide and N-terminal probrain natriuretic peptide, high-sensitivity troponin T, growth-differentiating factor 15, and soluble ST2. There was also a trend toward a lower level of galectin-3 in the HFiEF group, but there was no difference in the levels of highsensitivity C-reactive protein between the 2 HF groups. Independent Correlates of Recovery of Ejection Fraction The stepwise forward and backward logistic regression analysis that forced the baseline EF into the model (n=3511) identified 7 variables that were independent correlates of HFiEF: male sex (odds ratio [OR], 0.69), ischemic pathogenesis (OR, 0.41), body mass index (OR, 0.96), diastolic blood pressure (OR, 1.01), LVIDd/BSA (OR, 0.5), β-blocker therapy at baseline (OR, 1.9), and treatment with valsartan (OR, 1.5). Subjects who had higher blood pressure and those treated with a β-blocker or randomized to valsartan had greater odds of being in the HFiEF group, whereas those with an ischemic pathogenesis or more dilated left ventricle had much lower odds of a substantial improvement in EF. In addition to these 7 variables, the following neurohormones were measured in a large subset of subjects (n=2380): B-type natriuretic peptide, norepinephrine, PRA, aldosterone, high-sensitivity C-reactive protein, detectable troponin, and level of hs-troponin T. Out of these variables, only a detectable hs-troponin T at baseline was independently associated with reduced odds of being in the HFiEF group (OR, 0.43). The median (interquartile range) of probabilities of being in the HFiEF group estimated using a logistic regression model with the 8 independent correlates were 0.15 (0.08–0.22) in the HFiEF group and 0.06 (0.03–0.10) in the continued HFrEF group. The area under the receiver operating characteristic curve was 0.76 (95% confidence interval, 0.72–0.79). Thus, these 8 baseline variables provided some discrimination of subjects who had a substantially improved EF >12 months of follow-up. However, only 3 subjects had >50% estimated likelihood of being in the HFiEF group. Survival The 3519 subjects who had baseline EF of <35% and a 12-month assessment of EF were followed for a maximum Discussion In this Val-HeFT population, 9% of subjects with a baseline EF of <35% recovered their EF at 12 months. This group of subjects with HFiEF had a higher prevalence of hypertension, a lower prevalence of ischemic heart disease, a less severe hemodynamic, biomarker, and neurohormonal profile, and they were treated with a more intense HF medication regimen. Subjects who had higher blood pressure and those treated with a β-blocker or randomized to valsartan had greater odds of being in the HFiEF group, whereas those with an ischemic pathogenesis, a more dilated left ventricle, and a detectable hs-troponin T at baseline had much lower odds of a substantial improvement in EF. Improvement of the EF to >40% was associated with a better survival compared with persistently reduced EF. Our data support HFiEF as a stratum of HFrEF with a more favorable outcome, which occurs in a minority of patients with HFrEF who have a lower prevalence of ischemic heart disease, a less severe hemodynamic, biomarker, and neurohormonal profile and who are treated with a more intense HF medication regimen. In our patient population, only 9% of subjects with a baseline EF of <35% recovered their EF to >40% at 12 months. This is close to 10% of patients with a baseline EF of <50%, who recovered their EF to ≥50% in the study by Basuray et al.3 Our results are consistent with others in that, compared with HFrEF, subjects with HFiEF are younger,2,3 with a lower prevalence of coronary artery disease,2 a better renal function,2,3 and a better biomarker and neurohormonal profile.3 In contrast to other reports,2,3 our subjects with HFiEF had a similar symptom profile compared with subjects with HFrEF and were more likely to be treated with a β-blocker, an agent known to improve EF and long-term survival in HFiEF.17 New in this study are the findings that patients randomized to valsartan treatment had greater odds of being in the HFiEF group. Our study identified 8 variables that were independent correlates of HFiEF: male sex, ischemic pathogenesis, body mass index, diastolic blood pressure, LVIDd/BSA, detectable hs-troponin T, β-blocker therapy at baseline, and treatment with valsartan. However, we could not determine why the EF improved. Although these variables may be useful to predict which patients are more likely to have improvement in EF, all the 8 independent correlates combined identified only a few subjects who had a high probability of improvement in EF. Their predictive performance needs to be confirmed in other patient populations. Our results are consistent with others in that, compared with HFrEF, subjects with HFiEF have a better long-term 5 Florea et al Heart Failure With Improved Ejection Fraction Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 survival.3 Other studies showed better long-term outcomes in patients with HF who have had an improvement in EF. Cintron et al18 assessed the prognostic value of serial changes in EF in patients with chronic HF in the V-HeFT (Vasodilator–Heart Failure Trial) and found a significant and proportionate relationship between the direction and magnitude of changes in EF over time and the 1-year mortality. Serial assessments of left ventricular dimensions and function in the Studies of Left Ventricular Dysfunction (SOLVD)19 and Australia–New Zealand Carvedilol Heart Failure20 echocardiographic substudies, the Metoprolol CR/XL Randomized Intervention Trial in Heart Failure (MERIT-HF) magnetic resonance imaging substudy,21 and the A-HeFT (African American Heart Failure Trial)22 have also found an association between favorable changes in left ventricular dimensions and EF and improved clinical outcome produced by enalapril, carvedilol, metoprolol, or isosorbide dinitrate and hydralazine combination. In the study by Cintron et al,18 changes in EF of >5% from baseline at 6 months (V-HeFT I) and 12 months (V-HeFT II), irrespective of whether the follow-up EF reached a certain recovery level, were the strongest predictors of survival and remained significant even after adjustment for therapy and baseline EF. Although this is perhaps the only study that addressed and found a consistent proportionality between the degree of change in the EF and the subsequent change in mortality, it suggests that any substantial improvement in EF is associated with an improvement in survival. Several available publications have defined the subset of patients with HFpEF who previously had HFrEF as heart failure with recovered ejection fraction2,3,17 or heart failure with better ejection fraction4,23 and have been using different EF cut-off points for defining this HF category (≥40%,2 ≥45%,17 and ≥50%3,4). In this article, we used the definition of heart failure with improved ejection fraction with the cut-off point of >40%, consistent with the current guideline for the management of heart failure.1 We chose to truncate the population by analyzing only patients whose baseline EF was <35%, rather than including the entire Val-HeFT population with an EF of <40% because we wanted to identify a group that clearly had an improved EF to >40%. Given the error in measurement of EF, we felt a clear improvement in EF should be at least 5%. Strengths and Limitations We used well-characterized patients in the Val-HeFT trial where outcomes were adjudicated. In addition, we were able to examine EF improvement along with several established prognostic variables, including troponin and N-terminal probrain natriuretic peptide. The use of β-blockers and mineralocorticoid receptor antagonists was lower in the Val-HeFT population compared with that seen in contemporary clinical trials as was the absence of cardiac resynchronization therapy in the Val-HeFT population. Because these therapies strongly affect reverse remodeling and recovery of systolic function, these might influence the proportion of patients with improved EF and the overall impact of our results. In addition, we were not able to present the data on whether the patients who entered this study were on target doses of β-blockers or angiotensinconverting enzyme inhibitors and for how long. Although we found only 9% of patients with a baseline EF of <35% who had a 12-month EF of >40%, this probably underestimated the true proportion of patients with systolic dysfunction who got to the recovered state because the patients who entered this study have already been on optimal HF therapy. When individuals are recruited into new trials while on background therapy and there is an EF eligibility criterion, eligible patients will predominantly be nonresponders to standard therapy and with a poor prognosis. Thus, the patients entered into the new trials may not be adequately representative of HF seen in clinical practice. Val-HeFT enrolled patients with an EF of <40%. We excluded ≈12% of the Val-HeFT subjects who did not have a baseline EF of <35% and ≈18% who did not have a 12-month EF. Thus, our findings do not represent the entire Val-HeFT cohort. Although we report several state-of-practice statistical indices for evaluating prediction models, the individual predicted probabilities and predicted event-free survival curves that are most directly applicable to clinical practice ignore the uncertainty in the estimates as is often done when prediction models are used in clinical practice. Conclusions In this sample of patients with chronic HF, a minority of subjects with a baseline EF of <35% improved their EF to >40% at 12 months. This group of subjects with HFiEF had a higher prevalence of hypertension, a lower prevalence of ischemic heart disease, a less severe hemodynamic, biomarker, and neurohormonal profile, and they were treated with a more intense HF medication regimen. Subjects who had higher blood pressure and those treated with a β-blocker or randomized to valsartan had greater odds of being in the HFiEF group, whereas those with an ischemic pathogenesis, a more dilated left ventricle, and a detectable hs-troponin T at baseline had much lower odds of a substantial improvement in EF. Improvement in the EF was associated with a better survival compared with persistently reduced EF. Our data support HFiEF as a stratum of HFrEF with a less severe hemodynamic, biomarker, and neurohormonal profile, who are treated with a more intense HF medication regimen, and who experience a more favorable change in LV function and long-term survival. However, additional studies are needed to determine whether HFiEF represents enduring recovery or a separate HF clinical entity that could be treated differently. Sources of Funding Novartis sponsored the Valsartan Heart Failure Trial (Val-HeFT). Dr Rector was supported by Veterans Health Administration Health Services Research and Development Grant HFP-98-001. Disclosures Drs Anand and Cohn received research grants and honoraria from Novartis. The other authors report no conflicts. References 1. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on 6 Florea et al Heart Failure With Improved Ejection Fraction Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 practice guidelines. Circulation. 2013;128:1810–1852. doi: 10.1161/ CIR.0b013e31829e8807. 2. Punnoose LR, Givertz MM, Lewis EF, Pratibhu P, Stevenson LW, Desai AS. Heart failure with recovered ejection fraction: a distinct clinical entity. J Card Fail. 2011;17:527–532. doi: 10.1016/j.cardfail.2011.03.005. 3. Basuray A, French B, Ky B, Vorovich E, Olt C, Sweitzer NK, Cappola TP, Fang JC. Heart failure with recovered ejection fraction: clinical description, biomarkers, and outcomes. Circulation. 2014;129:2380–2387. doi: 10.1161/CIRCULATIONAHA.113.006855. 4. Joyce E, Chung C, Badloe S, Odutayo K, Desai A, Givertz MM, Nohria A, Lakdawala NK, Stewart GC, Young M, Weintraub J, Stevenson LW, Lewis EF. Variable Contribution of Heart Failure to Quality of Life in Ambulatory Heart Failure With Reduced, Better, or Preserved Ejection Fraction. JACC Heart Fail. 2016;4:184–193. doi: 10.1016/j.jchf.2015.12.011. 5. Cohn JN, Tognoni G; Valsartan Heart Failure Trial Investigators. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–1675. doi: 10.1056/ NEJMoa010713. 6. Wong M, Staszewsky L, Latini R, Barlera S, Glazer R, Aknay N, Hester A, Anand I, Cohn JN. Severity of left ventricular remodeling defines outcomes and response to therapy in heart failure: Valsartan heart failure trial (Val-HeFT) echocardiographic data. J Am Coll Cardiol. 2004;43:2022–2027. doi: 10.1016/j.jacc.2003.12.053. 7. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ; Chamber Quantification Writing Group; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. 8. Wong M, Staszewsky L, Volpi A, Latini R, Barlera S, Höglund C. Quality assessment and quality control of echocardiographic performance in a large multicenter international study: Valsartan in heart failure trial (ValHeFT). J Am Soc Echocardiogr. 2002;15:293–301. 9. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. 10. Masson S, Latini R, Anand IS, Vago T, Angelici L, Barlera S, Missov ED, Clerico A, Tognoni G, Cohn JN: Direct comparison of B-type natriuretic peptide (BNP) and amino-terminal proBNP in a large population of patients with chronic and symptomatic heart failure: the Valsartan Heart Failure (Val-HeFT) data. Clin Chem 2006;52:1528–1538. 11. Anand IS, Fisher LD, Chiang YT, Latini R, Masson S, Maggioni AP, Glazer RD, Tognoni G, Cohn JN; Val-HeFT Investigators. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation. 2003;107:1278–1283. 12. Latini R, Masson S, Anand IS, Missov E, Carlson M, Vago T, Angelici L, Barlera S, Parrinello G, Maggioni AP, Tognoni G, Cohn JN. Prognostic value of very low plasma concentrations of troponin T in patients with stable chronic heart failure. Circulation 2007;116:1242–1249. 13.Anand IS, Latini R, Florea VG, Kuskowski MA, Rector T, Masson S, Signorini S, Mocarelli P, Hester A, Glazer R, Cohn JN; Val-HeFT Investigators. C-reactive protein in heart failure: prognostic value and the effect of valsartan. Circulation. 2005;112:1428–1434. doi: 10.1161/ CIRCULATIONAHA.104.508465. 14. Anand IS, Rector TS, Kuskowski M, Adourian A, Muntendam P, Cohn JN. Baseline and serial measurements of galectin-3 in patients with heart failure: relationship to prognosis and effect of treatment with valsartan in the Val-HeFT. Eur J Heart Fail. 2013;15:511–518. doi: 10.1093/eurjhf/ hfs205. 15. Anand IS, Rector TS, Kuskowski M, Snider J, Cohn JN. Prognostic value of soluble ST2 in the Valsartan Heart Failure Trial. Circ Heart Fail. 2014;7:418–426. doi: 10.1161/CIRCHEARTFAILURE.113.001036. 16.Anand IS, Kempf T, Rector TS, Tapken H, Allhoff T, Jantzen F, Kuskowski M, Cohn JN, Drexler H, Wollert KC. Serial measurement of growth-differentiation factor-15 in heart failure: relation to disease severity and prognosis in the Valsartan Heart Failure Trial. Circulation. 2010;122:1387–1395. doi: 10.1161/CIRCULATIONAHA.109.928846. 17.de Groote P, Fertin M, Duva Pentiah A, Goéminne C, Lamblin N, Bauters C. Long-term functional and clinical follow-up of patients with heart failure with recovered left ventricular ejection fraction after β-blocker therapy. Circ Heart Fail. 2014;7:434–439. doi: 10.1161/ CIRCHEARTFAILURE.113.000813. 18. Cintron G, Johnson G, Francis G, Cobb F, Cohn JN. Prognostic significance of serial changes in left ventricular ejection fraction in patients with congestive heart failure. The V-HeFT VA Cooperative Studies Group. Circulation 1993;87:VI17–VI23. 19. Greenberg B, Quinones MA, Koilpillai C, Limacher M, Shindler D, Benedict C, Shelton B. Effects of long-term enalapril therapy on cardiac structure and function in patients with left ventricular dysfunction. Results of the SOLVD echocardiography substudy. Circulation. 1995;91:2573–2581. 20. Doughty RN, Whalley GA, Gamble G, MacMahon S, Sharpe N. Left ventricular remodeling with carvedilol in patients with congestive heart failure due to ischemic heart disease. Australia-New Zealand Heart Failure Research Collaborative Group. J Am Coll Cardiol. 1997;29:1060–1066. 21. Groenning BA, Nilsson JC, Sondergaard L, Fritz-Hansen T, Larsson HB, Hildebrandt PR. Antiremodeling effects on the left ventricle during betablockade with metoprolol in the treatment of chronic heart failure. J Am Coll Cardiol. 2000;36:2072–2080. 22. Cohn JN, Tam SW, Anand IS, Taylor AL, Sabolinski ML, Worcel M. Isosorbide dinitrate and hydralazine in a fixed-dose combination produces further regression of left ventricular remodeling in a well-treated black population with heart failure: results from A-HeFT. J Card Fail 2007;13:331–339. 23. Stevenson LW. Heart failure with better ejection fraction: a modern diagnosis. Circulation 2014;129:2364–2367. CLINICAL PERSPECTIVE Current guidelines for the management of heart failure (HF) divide patients with HF into 2 categories: those with reduced ejection fraction (EF of ≤40%) and those with preserved EF (>40%; HFpEF). It has been recognized that a subset of patients with HFpEF previously had heart failure with reduced ejection fraction. These patients with recovery or improvement in EF may be clinically distinct from those with persistently preserved or reduced EF. The authors performed a post hoc analysis of the 5010 subjects enrolled in the Valsartan Heart Failure Trial (Val-HeFT) and identified 3519 subjects who had echocardiographic assessment of EF at both baseline and 12-month follow-up. In this sample of patients with chronic HF, a minority of subjects (9%) with a baseline EF of <35% improved their EF to >40% at 12 months. This group of subjects with HF with improved EF had a higher prevalence of hypertension, a lower prevalence of ischemic heart disease, a less severe hemodynamic, biomarker, and neurohormonal profile, and they were treated with a more intense HF medication regimen. Improvement in EF was associated with a better survival compared with persistently reduced EF. The authors propose HF with improved ejection fraction as a stratum of HF with reduced ejection fraction with a less severe hemodynamic, biomarker, and neurohormonal profile, who are treated with a more intense HF medication regimen, and who experience a more favorable change in LV function and long-term survival. Additional studies are needed to determine whether HF with improved ejection fraction represents enduring recovery or a separate HF clinical entity that could be treated differently. Heart Failure With Improved Ejection Fraction: Clinical Characteristics, Correlates of Recovery, and Survival: Results From the Valsartan Heart Failure Trial Viorel G. Florea, Thomas S. Rector, Inder S. Anand and Jay N. Cohn Downloaded from http://circheartfailure.ahajournals.org/ by guest on May 2, 2017 Circ Heart Fail. 2016;9: doi: 10.1161/CIRCHEARTFAILURE.116.003123 Circulation: Heart Failure is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2016 American Heart Association, Inc. All rights reserved. Print ISSN: 1941-3289. Online ISSN: 1941-3297 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circheartfailure.ahajournals.org/content/9/7/e003123 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation: Heart Failure can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation: Heart Failure is online at: http://circheartfailure.ahajournals.org//subscriptions/